ABC of C2 vertebra is rare and it often alludes to diagnostic as well as therapeutic dilemma, especially in the pediatric age group. Percutaneous intralesional injection offers a safer and non-invasive modality for diagnosis and treatment with favorable outcomes.
Dr. Himanshu R Prasad, Department of Spine Surgery, KIMS - Sunshine Hospital, Secunderabad, Telangana, India. E-mail: prasadhimanshu@gmail.com
Introduction: Aneurysmal bone cyst (ABC) of cervical spine is rare in the pediatric age groups. It brings along a gamut of problems in management such as growth disturbances, instability, deformities, and neurological deficiencies. We report a case that was successfully managed by intralesional injection, making it safe and reproducible.
Case Report: A 12-year-old girl presented with pain and swelling around the nape of neck that increased in size over 1 year. Imaging and biopsy were suggestive of ABC. She was managed with selective embolization and percutaneous injection of methylprednisolone and calcitonin. Injections were given twice over 2 months period. At 1½ year follow-up, the patient was asymptomatic and swelling had shrunk in size and lesions ossified.
Conclusion: ABC’S are rare lesions that can create therapeutic dilemma in the pediatric population. Intralesional injection of calcitonin and methylprednisolone can prove to be a safer and efficacious treatment modality.
Keywords: Pediatric spinal tumors, aneurysmal bone cyst, intralesional injection, calcitonin, methylprednisolone.
Aneurysmal bone cysts (ABCs) are benign, expansile osteolytic lesion that cause blown out “soap-bubble” appearance. They form about 20–30% of primary spinal tumors, 2–3% of them are located in cervical spine. These lesions are expansile and can extend into the vertebral body, occasionally compressing spinal cord, leading to neurological deficit [1]. Managing such cases in the pediatric age group can be challenging. A variety of treatment options have been described in the literature including surgical excision and curettage, embolization, radiation therapy, and injections with various sclerosants. However, these methods are fraught with risks and complications. We report a case of ABC involving C2 vertebra globally in a 12-year-old female that was managed with intralesional injection of methyl prednisolone with calcitonin, subsequently producing ossification and shrinkage of the lesion with symptomatic improvement.
A 12-year-old girl child presented with complaints of swelling around the nape of the neck associated with pain. The swelling, as reported by the parents, progressively increased in size over the period of 1 year. Pain was constant and dull aching in nature. Plain radiograph showed an expansile lytic lesion arising from the posterior elements of C2 vertebra (Fig. 1).
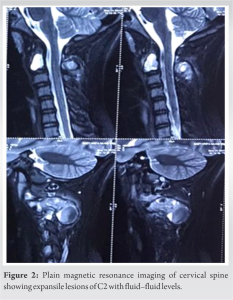
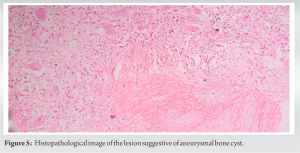
Van Arsdale in 1893 first reported ABC and called it as ossifying hematoma [2]. Later, Jaffe and Lichtenstein in 1942 coined the term ABC, defining it as a lesion that has a “blown out” appearance similar to saccular aneurysm [3]. The ABC majorly affects female patients of first decades. ABCs are benign, highly vascular lesions that affect specifically long, flat bone, leading to an expansile lytic lesion. In spine, dorsal, and lumbar segments are involved most commonly. Cervical spine forms 2–3% of spinal involvement [4]. The ABCs primarily affect the posterior elements of vertebrae and then extend through pedicle to the body. Although some literature report that these lesions originate in the pedicles. These lesions are expansile, lytic with thinning of cortices, and in some cases even causing neural compression. They have complete or incomplete endothelial lining but lack the elastic lamina or muscular layer as in true vessels [4, 5]. In case of secondary ABCs, apart from regular histology, there may be additional benign or malignant features such as those of GCT, fibrous dysplasia, chondroblastoma, chondrosarcoma, Ewing’s tumor, or metastatic carcinoma. The septations in primary ABCS in contrast to secondary are smooth, hypervascular with the absence of nodularities [4, 5]. The above pathology is characteristically demonstrated in CT/MRI showing sharp, well-defined expansile osteolytic lesions with thin smooth septations and cavities filled with fluid–fluid levels caused by hemorrhage into cavities. These are highly suggestive of ABC, though not specific. It may also be seen in GCT, chondroblastoma, and telangiectatic osteosarcomas. Nodularities in septations suggest secondary ABC [6]. In our study too, the lesion at C2 appeared as egg shelling of posterior arch and expanding in to the vertebral body with multiple fluid–filled level. There was no breach of spinal canal, and the patient was neurologically intact. Complete surgical curettage of the lesion as a modality of treatment has been described in the majority of the literature. However, recurrence remains a concern despite thorough curettage [6, 7]. Such aggressive surgery near craniovertebral junction necessitates spinal instrumentation and fusion to prevent the inherent instability, the procedure colludes with, apart from risk to neural elements [5]. However, in a growing child, offering such procedure may be undesirable. Radiation therapy alone or as an adjuvant has been advocated at some centers but carries an inherent risk of growth abnormalities or malignant transformation in these young population groups. Recurrence after radiation therapy is another significant concern [7]. Perioperative selective arterial embolization forms an essential step in the management algorithm of ABC. In addition, embolization alone has been known to remit the lesion in some cases, although repeated procedure may be needed [7]. In our case, the patient received selective arterial embolization as a pre-procedure workup. Intralesional injection therapy with sclerosants has been described in ABC lesions of spine. However, using sclerosants can be detrimental in the outcomes if it leaks into the spinal canal or craniovertebral vascular system [7, 8]. Injecting calcitonin and methylprednisolone have been described by some authors. Gladden et al. had presented a case report of ABC of lateral mass of C1 vertebra that was managed with intralesional steroid and calcitonin injection [9]. Ohashi et al. in 2008 reported a case of pathological fracture of C2 with ABC that was managed conservatively with halo vest. They also reported fracture healing and ossification of the lesion using injection of calcitonin and methyl prednisolone. However, the authors deferred pre-operative embolization to negate the risk of embolizing spinal cord and brain stem vascular supply. Selective embolization of such lesions is well described and should be utilized to avoid significant blood loss that may happen even during biopsy. They also concluded that the injection method was effective, less invasive, and much safer for ABC [10]. Steroid acts by inhibiting fibroblastic action and reducing angiogenesis. Calcitonin, on the other hand, acts by inhibiting osteoclastic activity [9, 10]. Based on this philosophy, we used calcitonin 200IU and methylprednisolone 120 mg combination for intralesional injection. During the procedure, contrast medium was used to rule out any leakage into the spinal canal. Furthermore, navigation was used to guide the needle into the lesion safe from breaching the canal. Navigation helps in providing safe trajectory; CT guided can also be used; however, there is a concern of radiation in the pediatric age groups. At the latest follow-up of 18 months, there was dense osteoblastic activity filling up most of the cavities. Clinically, the patient has reduction in pain and decrease in the size of the lesion. As in our case, this method can take years to remit the lesion. Despite the time, this modality is less aggressive and risky, especially in the pediatric age group [9, 10, 11]. Most importantly, the alignment and stability of the spine remain unaffected. In our case, we gave two injections at 2-month interval. A multicenter study would be required to lay guidelines for the same.
ABCs are rare lesions of vertebral column that can create therapeutic dilemma in the pediatric population. Intralesional injection of calcitonin and methylprednisolone can prove to be a safer and efficacious alternative treatment modality and without affecting the native stability and alignment of cervical spine. However, long-term follow-up is intended to watch for recurrence or bony remodeling in these growing children. A multicenter study can help in laying down the guidelines and possibly change the way these lesions are managed in the pediatric age groups.
Percutaneous intralesional injection in ABC of vertebra can be a safer and non-invasive treatment modality, especially in the pediatric age groups with good outcome.
References
- 1.Mankin HJ, Hornicek FJ, Ortiz-Cruz E, Villafuerte J, Gebhardt MC. Aneurysmal bone cyst: A review of 150 patients. J Clin Oncol 2005;23:6756-62. [Google Scholar]
- 2.Van Arsdale WW. II. Ossifying haematoma. Ann Surg 1893;18:8-17. [Google Scholar]
- 3.Jaffe H, Lichtenstein L. Solitary unicameral bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg 1942;44:1004-25. [Google Scholar]
- 4.Boriani S, De Iure F, Campanacci L, Gasbarrini A, Bandiera S, Biagini R, et al. Aneurysmal bone cyst of the mobile spine: Report on 41 cases. Spine (Phila Pa 1976) 2001;26:27-35. [Google Scholar]
- 5.Liu JK, Brockmeyer DL, Dailey AT, Schmidt MH. Surgical management of aneurysmal bone cysts of the spine. Neurosurg Focus 2003;15:E4. [Google Scholar]
- 6.Kransdorf MJ, Sweet DE. Aneurysmal bone cyst: Concept, controversy, clinical presentation, and imaging. AJR Am J Roentgenol 1995;164:573-80. [Google Scholar]
- 7.Garg S, Mehta S, Dormans JP. Modern surgical treatment of primary aneurysmal bone cyst of the spine in children and adolescents. J Pediatr Orthop 2005;25:387-92. [Google Scholar]
- 8.Peraud A, Drake JM, Armstrong D, Hedden D, Babyn P, Wilson G. Fatal ethibloc embolization of vertebrobasilar system following percutaneous injection into aneurysmal bone cyst of the second cervical vertebra. AJNR Am J Neuroradiol 2004;25:1116-20. [Google Scholar]
- 9.Gladden ML Jr., Gillingham BL, Hennrikus W, Vaughan LM. Aneurysmal bone cyst of the first cervical vertebrae in a child treated with percutaneous intralesional injection of calcitonin and methylprednisolone. A case report. Spine (Phila Pa 1976) 2000;25:527-30. [Google Scholar]
- 10.Ohashi M, Ito T, Hirano T, Endo N. Percutaneous intralesional injection of calcitonin and methylprednisolone for treatment of an aneurysmal bone cyst at C-2. J Neurosurg Pediatr 2008;2:365-9. [Google Scholar]
- 11.Topouchian V, Mazda K, Hamze B, Laredo JD, Penneçot GF. Aneurysmal bone cysts in children: complications of fibrosing agent injection. Radiology 2004;232:522-6. [Google Scholar]