The posterior root of medial meniscus is vital in maintaining the hoop stress. A non-anatomical tunnel placement will lead to the failure of the repair and accentuate cartilage degeneration; hence, a thorough knowledge of the anatomical landmarks will help in making an optimal tibial tunnel, which is essential for successful long-term surgical outcome
Dr. Rajkumar S Amaravathi, Division of Sports Injury, Joint Preservation, and Regenerative Medicine, St. Johns Medical College, Bengaluru, Karnataka, India. E-mail: rajamarvathi@gmail.com
Introduction: Meniscal root tear decreases the ability of the meniscus to convert the axial load to radially directed hoop stress. This leads to a decreased contact area and increased contact pressures, leading to early osteoarthrosis of the knee and eventually higher chances of undergoing total knee replacement. Meniscal root repair helps to restore normal knee kinematics; however, non-anatomical repair results in increased strain in the repair and causes early failure of the repair, leading to abnormal knee kinematics.
Case Report: A 45-year-old female with a body mass index of 40.6, hypothyroid, and type II diabetes mellitus presented to the outpatient department with the complaints of left knee pain and difficulty in walking. She had undergone an arthroscopic medial meniscus posterior root repair 1 year back. Clinical and radiological examinations helped to diagnose a re-tear of the medial meniscus root with a non-anatomic tibial tunnel. She then underwent arthroscopic revision root repair surgery. Currently, the patient is at a 1-year follow-up and has resumed her activities of daily living.
Conclusion: Anatomical repair of the posterior horn of the medial meniscus is important in restoring normal knee kinematics and for the ability of the meniscus to maintain the hoop stress. Non-anatomic repair leads to early failure and progression to rapid cartilage degeneration, resulting in early osteoarthritis and eventual knee replacement. Any revision surgery presents its own different set of challenges. The basic principles must be adhered to while addressing any failure of the primary surgery.
Keywords: Medial meniscus, posterior root, non-anatomic, revision, root repair.
The meniscus acts as a cushion that converts the tibiofemoral axial load into circumferential hoop stress. Meniscal roots function as anchors to the anterior and posterior meniscal horns on the tibial plateau. Pagnani and Cooper first described meniscal root tears in 1991 [1] as the radial tears located within 10 mm of the meniscus insertion or a soft/bony tissue avulsion [2]. The prevalence of posterior root tears identified during knee arthroscopy was 7–9% overall with about two-third involving the medial meniscus and one-third involving the lateral meniscus [3]. Injury to this meniscal anchor to the tibial plateau causes the alteration of the biomechanics of the knee, leading to a decreased contact area and a 25% increase in peak contact pressure as compared to the normal state. Studies show that the medial meniscus posterior root tear (MMPRT) is biomechanically equivalent to total meniscectomy. These result in accelerated cartilage degeneration and meniscal extrusion, which eventually progresses to Fairbanks degenerative changes [4]. Untreated meniscal root tears have a high risk of cartilage deterioration of the affected compartment, leading to early knee osteoarthritis which may necessitate future knee replacement [2]. Historically, meniscal root tears were managed either conservatively or with partial or total meniscectomy. Meniscal root repair aims to restore normal joint kinematics and contact pressures. There are two main surgical techniques for root repair using a suture anchor or a transtibial pull-out technique. The pull-out technique has been postulated to have the added advantage of better healing of the meniscus due to the egress of the progenitor cells and growth factors due to tunnel drilling [5].
The patient was a 45-year-old female, morbidly obese with a body mass index (BMI) of 40.6, hypothyroidism, and type II diabetes mellitus. She presented to the outpatient department with complaints of left knee pain for the past 9 months. She had undergone arthroscopic left knee medial meniscus root repair 1 year back. Three months after her index surgery, the patient slipped and had a fall while descending the stairs, landing on the inner side of her knee. The patient experienced discomfort and swelling in her left knee, for which she symptomatically took over-the-counter analgesics, without seeking any medical guidance. The pain was gradually worsening and was accompanied by swelling and inability to bear weight on her left knee. Clinical examination of the left knee revealed quadriceps wasting along with medial joint line tenderness. The range of movement (ROM) of the knee was decreased with a flexion-extension arc between 0 and 100°. McMurray’s test and Apley’s grinding test were positive. Standard anteroposterior (weight bearing) and lateral radiographs of the knee joint showed Grade 2 Kellgren–Lawrence osteoarthritis changes along with a previous suture disc on the tibial side (Fig. 1). The lower limb scannogram showed no limb malalignment. T2-weighted magnetic resonance imaging showed a radial tear in the axial plane at the medial meniscal root. The absence of the posterior root in the sagittal sections (Ghost sign) could be appreciated. In the coronal images, a linear defect in the meniscal root (truncation sign) and extrusion of the medial meniscus >3 mm was seen (Fig. 2).  Evidence of previous tibial tunnel for root repair was present. The location of the tunnel exit on the tibial intra-articular side was reported to be at the level of the medial tibial eminence (MTE) apex in the coronal plane and 0.5 mm medial to it, implying that the previous tunnel was non-anatomic (Fig. 3). Based on these clinical and radiological findings, the diagnosis of re-tear of the medial meniscal root was established, and the patient was informed about the need for a revision surgery for the same. The aim of the surgery was to restore the meniscal root attachment to its anatomical footprint (Fig. 4) [6]. The patient underwent pre-operative rehabilitation to increase the ROM and strengthen the quadriceps and hamstring group of muscles. Two weeks later, the patient underwent revision arthroscopic medial meniscus root repair.
Evidence of previous tibial tunnel for root repair was present. The location of the tunnel exit on the tibial intra-articular side was reported to be at the level of the medial tibial eminence (MTE) apex in the coronal plane and 0.5 mm medial to it, implying that the previous tunnel was non-anatomic (Fig. 3). Based on these clinical and radiological findings, the diagnosis of re-tear of the medial meniscal root was established, and the patient was informed about the need for a revision surgery for the same. The aim of the surgery was to restore the meniscal root attachment to its anatomical footprint (Fig. 4) [6]. The patient underwent pre-operative rehabilitation to increase the ROM and strengthen the quadriceps and hamstring group of muscles. Two weeks later, the patient underwent revision arthroscopic medial meniscus root repair.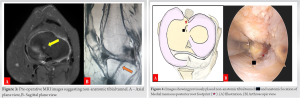
Surgical Technique
- Diagnostic arthroscopy
Under spinal anesthesia, the patient was positioned supine. Standard anterolateral and anteromedial portals were used for diagnostic arthroscopy of the knee. The anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) were both intact. There were Grade 2 (Outerbridge classification) cartilage changes on the medial femoral and tibial condyle. A MMPRT was noted (akin to type 2 Laprade et al.) [7]. The edges of the torn end were found to be rounded, and the residual stump of the root was absent. Previously used sutures were seen exiting from the tunnel which was well anterior and medial to the native footprint (Fig. 5a). It was confirmed to be in line with the MTE apex in the coronal plane and 0.5 mm medial to it.
- Repair of the MMPRT
Prior sutures were removed using a shaver. No. 2–0 fiber wire (Healthium Inc., Peenya, Bangalore) was loaded onto the self-retrieving suture passing device (Firstpass Mini, Smith and Nephew Inc., USA). The torn medial meniscus root was then captured by taking the first bite 5 mm from the edge of the torn end. Later, no. 2-0 fiber wire was railroaded with no. 2-fiber wire (Healthium Inc., Peenya, Bangalore), and a meniscal cinch loop was placed (Fig. 5b). Similarly, the second bite was taken at a distance of 5 mm from the first bite, and the second meniscal cinch loop was placed. Trephination was done to enhance healing.
- Tunnel preparation
A single transtibial tunnel technique was planned. As described earlier, the plan was to revise the tibial tunnel exit on the intra-articular side to the desired anatomical point (Fig. 5c). The meniscal footprint was prepared using the shaver and curette. Root repair jig (Smith and Nephew Inc., USA) was placed over the medial meniscus posterior root (MMPR) footprint. The 2.4 mm guide wire was advanced from the anteromedial surface of the tibia using the outside-in technique. Care was taken to achieve the articular exit of the guidewire over the center of the anatomical footprint of the MMPR as described by Johannsen et al. (9.6 mm posterior and 0.7 mm lateral to the MTE apex) [6]. Next, using a 4.5 mm reamer over the guidewire, a tibial tunnel was reamed, followed by passing a no. 2 polydioxanone suture (PDS) into the tibial tunnel. Both the fiber wires were then loaded onto the PDS and then pulled out (pull-out technique) from the anteromedial surface of the tibia. Tibial fixation was subsequently obtained by securing the fiber wires over a suture disc (Smith and Nephew, USA) on the anteromedial surface of the tibia and tied with the knee in 30° of flexion to aid in the proper reduction of the meniscus. Placement of the meniscal root over the anatomic footprint was confirmed under direct arthroscopic vision (Fig. 5d). Accessory fixation of the sutures was done by tying them over the anteromedial surface of the proximal tibia.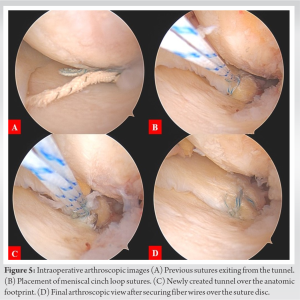
Post-operative rehabilitation
For the first 6 weeks, non-weight-bearing mobilization was allowed to protect the root repair and avoid hoop stress on the meniscus, along with knee flexion up to 60° using a knee ROM brace. For 6–9 weeks, partial weight-bearing mobilization and knee flexion up to 90° were permitted. After 9 weeks, the patient was allowed full weight-bearing mobilization, and the knee ROM brace was removed to allow free flexion as tolerated. Squatting was avoided for 4 months after the surgery to protect the root repair. Currently, the patient is at 1-year follow-up, has progressed clinically, achieving a full range of motion similar to the normal side, and has returned to her routine activities of daily living.
MMPRT accounts for 10–21% of all medial meniscus tears and 70% of all root tears. It is more often chronic and degenerative, commonly seen in middle-aged women but can also be seen in acute settings in association with multiligamentous injuries. It is the least mobile among the roots and hence has the highest incidence of tears among the meniscal roots. MMPRTs are associated with knee chondral defect 5.8 times more likely than lateral meniscus posterior root tear (LMPRT). The latter occurs in young and is 10.3 times more likely to have an associated ACL tear than MMPRT. In multiligamentous injuries, LMPRT is more common, whereas the incidence of MMPRT is only 3% [5, 8]. The risk factors for MMPRT are female sex, increased BMI, higher age, varus alignment, and increased Kellgren–Lawrence grade [9]. Iatrogenic injury to the MMPRT has been seen with the non-anatomic placement of the tibial tunnel in PCL reconstructions due to its close proximity [2]. Simultaneous assessment of cartilage health, alignment, and ligamentous factors is key to the success of root repair as failure to address these pathologies is the underlying cause of the need for a second surgery after the initial knee preservation surgery [10]. The rate of revision surgery following meniscal repair in a meta-analysis was found around 19.1% and most of the failures occurred after the second post-operative year [11]. Mechanical studies have found that a 3 mm translation of the root attachment medially from its anatomic position found a significant reduction in the conversion of tibiofemoral load into a circumferential load [12]. Similarly, the non-anatomic placement of the root attachment of the human medial meniscal transplant posteriorly has been shown to increase contact pressures in cadaveric knees [13]. Non-anatomic repair alters the tibiofemoral contact biomechanics by decreasing contact area and increasing contact pressure at all flexion angles. In the described case, the non-anatomic placement of the tibial transosseous tunnel exits on the intra-articular side on the tibial plateau was the main reason for the failure of the primary meniscus root repair surgery. Most commonly, the root repair is done either using a suture anchor or a transtibial pull-out technique. Repair using a suture anchor is technically demanding; hence, the latter is more commonly used. However, the long length of the suture causes micromotion at the root repair or the bungee effect which can interfere with the healing and hence failure of the repair [14]. Cerminara et al. have proposed that the reason for the displacement of the root is the failure of the meniscus suture rather than the bungee effect [15]. Studies have shown that the locking loop has superior strength when compared to simple sutures [10]. We used two locking cinch loop sutures with fiber wire for repair and secured by tying over a suture disc. There is a tendency for the meniscus to extrude after the root tear and get adhered posteromedially to the posterior capsule which might lead to the non-anatomic repair of the root tear. It is essential to release the extruded meniscus from posteromedial capsule adhesions to create a near-normal anatomic repair [16], but this is a double-edged sword that can compromise the vascularity of the meniscus and hence the repair.
Anatomical repair of the posterior horn of the medial meniscus is important in restoring normal knee kinematics and for the ability of the meniscus to maintain the hoop stress. Non-anatomic repair leads to early failure and progression to rapid cartilage degeneration, resulting in early osteoarthritis and eventual knee replacement. Any revision surgery presents its own different set of challenges. The basic principles must be adhered to while addressing any failure of the primary surgery.
The posterior horn of the medial meniscus is the cornerstone in maintaining hoop stress. Optimal placement of an anatomical tibial tunnel is very essential for the successful long-term outcome for the patient.
References
- 1.Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy 1991;7:297-300. [Google Scholar]
- 2.Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, et al. Meniscal root tears: Current concepts review. Arch Bone Jt Surg 2018;6:250-9. [Google Scholar]
- 3.LaPrade RF, Ho CP, James E, Crespo B, LaPrade CM, Matheny LM. Diagnostic accuracy of 3.0 T magnetic resonance imaging for the detection of meniscus posterior root pathology. Knee Surg Sports Traumatol Arthrosc 2015;23:152-7. [Google Scholar]
- 4.Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. Similar to total meniscectomy. J Bone Joint Surg Am 2008;90:1922-31. [Google Scholar]
- 5.Moatshe G, Chahla J, Slette E, Engebretsen L, Laprade RF. Posterior meniscal root injuries. Acta Orthop 2016;87:452-8. [Google Scholar]
- 6.Johannsen AM, Civitarese DM, Padalecki JR, Goldsmith MT, Wijdicks CA, LaPrade RF. Qualitative and quantitative anatomic analysis of the posterior root attachments of the medial and lateral menisci. Am J Sports Med 2012;40:2342-7. [Google Scholar]
- 7.LaPrade CM, James EW, Cram TR, Feagin JA, Engebretsen L, LaPrade RF. Meniscal root tears: A classification system based on tear morphology. Am J Sports Med 2015;43:363-9. [Google Scholar]
- 8.Matheny LM, Ockuly AC, Steadman JR, LaPrade RF. Posterior meniscus root tears: Associated pathologies to assist as diagnostic tools. Knee Surg Sports Traumatol Arthrosc 2015;23:3127-31. [Google Scholar]
- 9.Hwang BY, Kim SJ, Lee SW, Lee HE, Lee CK, Hunter DJ, et al. Risk factors for medial meniscus posterior root tear. Am J Sports Med 2012;40:1606-10. [Google Scholar]
- 10.Krych AJ, Hevesi M, Desai VS, Camp CL, Stuart MJ, Saris DB. Learning from failure in cartilage repair surgery: An analysis of the mode of failure of primary procedures in consecutive cases at a tertiary referral center. Orthop J Sports Med 2018;6:2325967118773041 . [Google Scholar]
- 11.Schweizer C, Hanreich C, Tscholl PM, Ristl R, Apprich S, Windhager R, et al. Nineteen percent of meniscus repairs are being revised and failures frequently occur after the second postoperative year: A systematic review and meta-analysis with a minimum follow-up of 5 years. Knee Surg Sports Traumatol Arthrosc 2022;30:2267-76. [Google Scholar]
- 12.Stärke C, Kopf S, Gröbel KH, Becker R. The effect of a nonanatomic repair of the meniscal horn attachment on meniscal tension: A biomechanical study. Arthroscopy 2010;26:358-65. [Google Scholar]
- 13.Sekaran SV, Hull ML, Howell SM. Nonanatomic location of the posterior horn of a medial meniscal autograft implanted in a cadaveric knee adversely affects the pressure distribution on the tibial plateau. Am J Sports Med 2002;30:74-82. [Google Scholar]
- 14.Feucht MJ, Grande E, Brunhuber J, Rosenstiel N, Burgkart R, Imhoff AB, et al. Biomechanical comparison between suture anchor and transtibial pull-out repair for posterior medial meniscus root tears. Am J Sports Med 2014;42:187-93. [Google Scholar]
- 15.Cerminara AJ, LaPrade CM, Smith SD, Ellman MB, Wijdicks CA, LaPrade RF. Biomechanical evaluation of a transtibial pull-out meniscal root repair: Challenging the bungee effect. Am J Sports Med 2014;42:2988-95. [Google Scholar]
- 16.LaPrade CM, Foad A, Smith SD, Turnbull TL, Dornan GJ, Engebretsen L, et al. Biomechanical consequences of a nonanatomic posterior medial meniscal root repair. Am J Sports Med 2015;43:912-20. [Google Scholar]