An internal bracing construct and early rehabilitation may lead to a good or excellent outcome following an isolated hamate dislocation.
Trenden Flanigan, Department of Orthopaedic Surgery, Loma Linda University Health Consortium, 11406 Loma Linda Drive, Suite 214A, Loma Linda, California 92354. E-mail: tflanigan@llu.edu
Introduction: Isolated hamate dislocation is a rare case with potentially devastating complications, given the resultant instability of the carpus following the injury. This has been reported in the literature before with varying constructs and varying results but never with an internal bracing construct and early rehabilitation.
Case Report: A 26-year-old male injured his left hand in an all-terrain vehicle accident. After initial misdiagnosis and subsequent persistent pain, he was diagnosed with a chronic dorsal hamate dislocation. An open reduction and internal brace fixation were performed resulting in an anatomic and stable reduction. By the final follow-up visit, the patient had no pain with near full range of motion and had returned to work with good to excellent outcome scores.
Conclusion: Open reduction with ligament reconstruction utilizing an internal bracing technique provides a stable fixation and anatomic repair of the intercarpal and carpometacarpal ligaments. This is a feasible treatment option for hamate dislocations that allows for early rehabilitation in comparison to previously described methods and may result in good to excellent outcomes.
Keywords: Hamate, dislocation, internal brace.
The hamate bone is a wedge-shaped bone located within the distal carpal row. It articulates with the capitate bone radially, the triquetrum proximally, and the ring and small finger metacarpals distally [1]. The hook of the hamate, a curved bony projection extending from the volar surface of the hamate body, forms the radial border of the ulnar tunnel (Guyon’s canal) and the ulnar border of the carpal tunnel [2]. In general, hamate injuries are rare. Among hamate injuries, fracture is the most common injury pattern, despite accounting for only 2–4% of all carpal bone fractures [3]. This report is of an isolated hamate dislocation. These are an even more rare occurrence within the orthopedic literature, with only 23 cases reported to date [4]. Because these injuries are so rare, there is a paucity of evidence on the ideal method of treatment. The first isolated hamate dislocation was described by Buchanan in 1882 [5]. Since that time, there have been a variety of treatment modalities used, ranging from conservative (no reduction) [6] to surgical excision [7], closed reduction and immobilization, closed reduction with surgical fixation, and open reduction with internal fixation [8]. Within the limited available literature, Kirschner wire fixation was found to be the most common method of surgical fixation though no consistent pattern of results has been found with any specific method of fixation.
A 26-year-old right-hand dominant Caucasian male without significant medical history landed on his outstretched left hand when crashing his all-terrain vehicle, resulting in immediate pain and swelling. An outside urgent care center found no fractures or dislocations on plain radiographs and subsequently splinted the left wrist due to pain. He presented to an orthopedic hand surgery outpatient office 4 weeks after the injury with persistent pain and decreased range of motion. No obvious deformity was noted, but the patient was tender to palpation over the dorsal carpus as well as the carpal tunnel. The patient was neurovascularly intact at the time of presentation. New plain radiographs were obtained, demonstrating an isolated dorsal hamate dislocation in the absence of any fracture, as noted in Fig. 1 and 2. Given the chronicity of the injury, closed reduction was not attempted due to the high likelihood of failure. The patient underwent an open reduction with internal fixation of the isolated hamate dislocation.
Operation
A standard longitudinal dorsal approach to the wrist was performed. The diastasis between the capitate and triquetrum was easily visualized. The hamate, which had dislocated dorsal and ulnar, was found dorsal to the triquetrum in a bed of fibrinous debris. The interposed blocking fibrinous debris from the resultant void between the capitate and triquetrum was removed and the hamate bone carefully dissected and reduced to its anatomic position. Two Kirschner wires were used for provisional fixation. Under direct visualization, it could be seen that the ring and small finger carpometacarpal ligaments had avulsed off the carpus, creating dynamic carpometacarpal instability. The metacarpals were subsequently reduced and held in place using Kirschner wires to the distal hamate. This was verified both visually and on intraoperative fluoroscopy.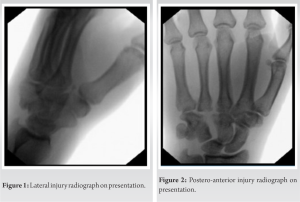
Definitive fixation was achieved by utilizing multiple suture tape bridges and fixation with bone anchors to reinforce the failed dorsal carpal and carpometacarpal ligaments in an internal bracing method. This is an augmentation method that uses high-strength non-absorbable suture tape to overlay the ruptured ligaments and provide support during ligamentous healing and scar formation. The first bone anchor (3.5-mm DX SwiveLock SL; Arthrex, Naples, FL) was placed in the hamate. This was attached to a suture tape (FiberTape; Arthrex, Naples, FL) that was subsequently anchored into the capitate with one limb and a second limb anchored to the triquetrum, as shown in Fig. 3. 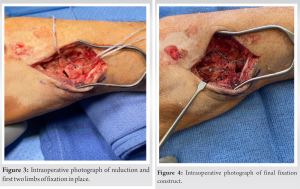 This completed the internal bracing of the hamate to the capitate and lunate. Another anchor was then placed distally on the hamate, in conjunction with two more suture tape and anchor constructs into the ring finger and small finger, respectively. This stabilized the failed carpometacarpal ligaments and maintained reduction of the carpometacarpal joints. Fig. 4 is an intraoperative photograph demonstrating the final, stable construct.
This completed the internal bracing of the hamate to the capitate and lunate. Another anchor was then placed distally on the hamate, in conjunction with two more suture tape and anchor constructs into the ring finger and small finger, respectively. This stabilized the failed carpometacarpal ligaments and maintained reduction of the carpometacarpal joints. Fig. 4 is an intraoperative photograph demonstrating the final, stable construct.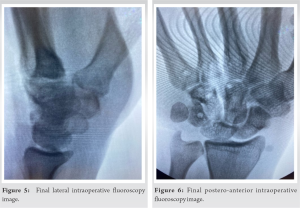 Figs. 5 and 6 show the final intraoperative fluoroscopy images after removal of the provisional fixation. The patient was placed in a post-operative splint and was kept with the wrist immobilized and fingers free for 6 weeks, followed by aggressive hand therapy to treat any subsequent stiffness and weakness. The rehabilitation protocol followed in this case consisted of 6 weeks of immobilization followed by 3 weeks of range of motion stretching. This was followed by light strengthening with progression to full release of all activities at 3 months post-operatively.
Figs. 5 and 6 show the final intraoperative fluoroscopy images after removal of the provisional fixation. The patient was placed in a post-operative splint and was kept with the wrist immobilized and fingers free for 6 weeks, followed by aggressive hand therapy to treat any subsequent stiffness and weakness. The rehabilitation protocol followed in this case consisted of 6 weeks of immobilization followed by 3 weeks of range of motion stretching. This was followed by light strengthening with progression to full release of all activities at 3 months post-operatively.

The patient was followed at various time intervals up to 14 months post-operatively. On his final return to clinic, range of motion (Figs. 7 and 8) was painless and nearly equal to contralateral wrist with 52° of flexion, 67° of extension, 15° of radial deviation, 26° of ulnar deviation, 83° of supination and pronation, and the ability to make a strong composite fist. Grip strength was 62.5 kg on the right and 47.6 kg on the affected left side. Key pinch was 12.7kg on the right and 11.7 kg on the left. Tip pinch was 8.1 kg on the right and 7.2 kg on the left. This disparity in strength is within normal limits for variance between hands when taking handedness into account. The quick DASH score was 4.5% and DASH score was 5/100. The Michigan Hand score was 65.2. The patient returned to work as a truck driver with no limitations. Figs. 9 and 10 are final outpatient post-operative radiographs demonstrating a well-positioned and well-vascularized hamate with no change in alignment and no collapse compared to prior films.
In general, the mechanism of dislocation results from a high-energy force transmitted directly through the carpal bones [4]. Wang et al. postulated that the direction of dislocation may be dependent on the integrity of the transverse carpal ligament – if the transverse carpal ligament remains intact, the hamate may dislocate volarly, whereas if the transverse carpal ligament is disrupted, the hamate will then dislocate dorsally [9]. This was reinforced in this case as the transverse carpal ligament was likely disrupted in the setting of a dorsal dislocation. Given the high-energy mechanism involved in producing this injury pattern and the proximity of the hamate to both the ulnar and carpal tunnels, it is not surprising that cases of ulnar nerve dysfunction [4, 10] and compartment syndrome [11] have been noted in the literature. Outcome data are mixed after reduction and surgical fixation of hamate dislocations. In their literature review, Wang et al. [4] found disparate results of post-reduction pain and functionality – 7 of the 20 cases; they reviewed had resolution of pain and return of full functionality [8]. The aforementioned suture tape and anchor technique for stabilization and reconstruction of the dorsal hamate ligaments have not been described in published literature. The internal bracing technique is well established as a successful method of treatment for ligamentous ruptures in the joints of the upper limb. It provides the inherent stability and support required during ligamentous healing and scar formation. It was therefore reasoned that this same principle could be applied to ligamentous ruptures on the hamate bone. It should be noted that Arnaud et al. [12] utilized extensor carpi ulnaris tendon autograft to reconstruct the hamate ligaments and achieve good clinical outcomes (10° loss of extension compared to contralateral hand at 12-month follow-up) in a patient with a chronic hamate dislocation diagnosed at 3-month post-injury. The patient presented in this report achieved similar good results without the morbidity of a harvested tendon graft. This may suggest that patients heretofore traditionally treated with Kirschner wire immobilization may benefit from ligament reconstruction. In addition, this patient did well in the initial post-operative period despite being released from all immobilization at 6 weeks post-operatively in comparison to previous reports of 2–3 months of immobilization with other fixation methods. This early rehabilitation was likely a factor in his regaining a large portion of his range of motion without pain, significant stiffness, or other morbidity.
This case demonstrates that early detection, stable reconstruction with the internal brace construct, and early rehabilitation may lead to a good or excellent outcome following an isolated hamate dislocation, as occurred for the patient described in this report. The patient had good resolution of pain, return of functionality, and excellent patient-reported outcomes at 14 months post-operatively. Based on these findings, a stable and anatomic reduction can be achieved and maintained with an internal bracing technique.
The goal of this case report is to demonstrate a modern fixation alternative to traditional fixation methods that allow for an early rehab option and good to excellent results following the rare injury of an isolated hamate dislocation.
References
- 1.Abrego M, De Cicco F. Hamate fractures. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544314/#_NBK544314_pubdet. Accessed 05 February 2023. [Google Scholar]
- 2.Davis DL. Hook of the hamate: The spectrum of often missed pathologic findings. AJR Am J Roentgenol 2017;209:1110-8. [Google Scholar]
- 3.Price MB, Vanorny D, Mitchell S, Wu C. Hamate body fractures: A comprehensive review of the literature. Curr Rev Musculoskelet Med 2021;14:475-84. [Google Scholar]
- 4.Wang X, Jia X, Zhang X, Liu B, Zhang Z, Sang H. Isolated complete dislocation of hamate bone with an ulnar nerve injury: A case report and literature review. Ann Transl Med 2022;10:385. [Google Scholar]
- 5.Buchanan J. Luxation of the unciform bone. Phil Med Surg Rep 1882;46:418-9. [Google Scholar]
- 6.Ebermayer F. Ueber (isolierte) verletzungen der hand-wurzelknochen. Fortschritte auf dem Gebiet der Röntgen-strahlen. Ergänzungsband 1908;12:1-22. [Google Scholar]
- 7.Murphy JB. Dislocation of the left unciform bone. Surg Clin 1915;4:423-7. [Google Scholar]
- 8.Zieren J, Agnes A, Müller J. Isolated dislocation of the hamate bone. Case report and review of the literature. Arch Orthop Trauma Surg 2000;120:535-7. [Google Scholar]
- 9.Wang L, Xiong G, Dai L. Dislocation of the hamate and its possible mechanism. J Hand Surg Eur 2013;38:556-7. [Google Scholar]
- 10.Matsumoto T, Tsunoda M, Yamaguchi S, Koso K, Matsushita S, Kurosaka M, et al. Traumatic dislocation of the hamate and pisiform: A case report and review of the literature. J Orthop Trauma 2005;19:282-5. [Google Scholar]
- 11.Saiz AM Jr., Wuellner JC, Bayne CO. Isolated dislocation of hamate with hook fracture in setting of acute hand compartment syndrome: A case report and review of the literature. J Orthop Case Rep 2020;10:76-9. [Google Scholar]
- 12.Arnaud JP, Girou P, Mabit C, et al. Luxation of the hamate bone. Apropos of a case with review of the literature. Ann Chir Main 1987;6:222-4. 10.1016/S0753-9053(87)80063-7. [Google Scholar]









