Clinical implications and management of an unusual recurrence of spinal tuberculosis.
Dr. Lav Mehta, Department of Orthopaedics, Post Graduate Institute of Medical Education and Research, Chandigarh, India. E-mail: mehta.lav@gmail.com
Introduction: Spinal tuberculosis (TB) recurrence in subjacent vertebral segments in a post-operative case is one of the atypical presentations of this common disease.
Case Report: A 63-year-old gentleman presented with fever and bilateral lower limb weakness for 10 days. The patient was on anti-tubercular therapy for the past 18 months and had a history of surgical decompression and posterior instrumentation for D12 and L1 vertebrae spinal TB. Radiological investigations showed new-onset TB in D9 and D10 vertebral levels. Management with revision surgery was done.
Conclusion: Recurrence of spinal TB in segments of vertebrae subjacent to previously operated segments in a patient on long-term anti-tubercular treatment is a rare and undescribed presentation of the common disease. High index of suspicion is required for early diagnosis and prompt management to prevent long-term morbidities.
Keywords: Spinal tuberculosis, anti-tubercular therapy, post-operative recurrence.
One of the earliest diseases that humans have ever encountered is spinal tuberculosis (TB), which has been discovered in Egyptian mummies that date back to 3400 BC [1]. The literature shows that combined medicinal and surgical methods are frequently used to treat spinal TB [2]. Post-operative recurrence of spinal TB poses various challenges and has been reported in the literature with a variable rate ranging from 1.25% to 25% [3, 4]. However, most of these studies included cases with recurrence/relapse of TB in the same vertebral segments which were operated on earlier [5, 6]. There is a paucity of literature about the post-operative recurrence of spinal TB [7]. Recurrence of spinal TB in an individual – when caused by a different strain, is known as reinfection, and when caused due to a regrowth of the same strain of Mycobacterium tuberculosis that caused the previous TB episode is known as relapse [8]. Here, we describe a rare case of dorso-lumbar spinal TB managed surgically, completed 18 months of anti-tuberculosis treatment (ATT) course, and subsequently diagnosed with TB of vertebral segments subjacent to the operated segment.
This case involves a 63-year-old gentleman who complained of backache along with fever and loss of appetite 2 years back which lasted around 4–5 months. The patient took over-the-counter medications for the above complaints during the initial period of 4–5 months. As the symptoms were not relieved, the patient got MRI done at the consult of an Orthopaedic surgeon, and a diagnosis of tubercular spondylitis involving D-12 and L-1 vertebral bodies and intervening disc along with pre- and para-vertebral collection was made (Fig. 1). The patient was started on anti-tubercular therapy based on the clinicoradiological diagnosis of TB spine. Even after 6 months of anti-tubercular chemotherapy, the patient developed gradual onset weakness in bilateral lower limbs and was referred to our center. Due to the failure of chemotherapy as evidenced by progressive lower limb weakness even after 6 months of medical management, the patient was planned for surgery. Posterior decompression and pedicle screw fixation was done (Fig. 2). Pedicle screws were put in D11, D12, and L2 vertebrae. Post-operative course was uneventful and he was discharged with the continuation of anti-tubercular therapy. The patient was put on ATT regimen which consisted of HRZE (tablet isoniazid+tablet rifampicin+tablet pyrazinamide+tablet ethambutol) for initial 2 months followed by HRE for 7 months and then H+R for 9 months. At a 3-week follow-up visit, suture removal was done and the patient was mobilized using a walker. Till 15-month post-surgery, the patient was able to mobilize himself with the assistance of a cane or walker. He continued taking rifampicin and isoniazid combination drug during this period as per protocol. After 15 months of symptom-free period, the patient again presented to our OPD with complaints of fever and weakness in bilateral lower limbs and unable to walk for the past 10 days. On examination, the patient had spastic paralysis in extension in bilateral lower limbs, and UMN signs such as ankle clonus, patellar clonus, and Babinski sign were positive in both lower limbs. Deep tendon reflexes in bilateral lower limbs were exaggerated. The sensory loss was seen below the D10 level. The patient was catheterized due to urinary retention. Routine blood investigations, ESR, and CRP were found to be within normal limits. Radiological investigations were done (Fig. 3, 4, 5).
The patient was started on anti-tubercular therapy based on the clinicoradiological diagnosis of TB spine. Even after 6 months of anti-tubercular chemotherapy, the patient developed gradual onset weakness in bilateral lower limbs and was referred to our center. Due to the failure of chemotherapy as evidenced by progressive lower limb weakness even after 6 months of medical management, the patient was planned for surgery. Posterior decompression and pedicle screw fixation was done (Fig. 2). Pedicle screws were put in D11, D12, and L2 vertebrae. Post-operative course was uneventful and he was discharged with the continuation of anti-tubercular therapy. The patient was put on ATT regimen which consisted of HRZE (tablet isoniazid+tablet rifampicin+tablet pyrazinamide+tablet ethambutol) for initial 2 months followed by HRE for 7 months and then H+R for 9 months. At a 3-week follow-up visit, suture removal was done and the patient was mobilized using a walker. Till 15-month post-surgery, the patient was able to mobilize himself with the assistance of a cane or walker. He continued taking rifampicin and isoniazid combination drug during this period as per protocol. After 15 months of symptom-free period, the patient again presented to our OPD with complaints of fever and weakness in bilateral lower limbs and unable to walk for the past 10 days. On examination, the patient had spastic paralysis in extension in bilateral lower limbs, and UMN signs such as ankle clonus, patellar clonus, and Babinski sign were positive in both lower limbs. Deep tendon reflexes in bilateral lower limbs were exaggerated. The sensory loss was seen below the D10 level. The patient was catheterized due to urinary retention. Routine blood investigations, ESR, and CRP were found to be within normal limits. Radiological investigations were done (Fig. 3, 4, 5).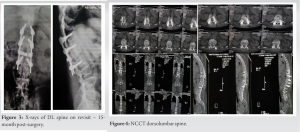 Based on the clinicoradiological findings, the patient was diagnosed with D9-D10 tubercular spondylitis with cord compression and neural deficits. Revision surgery was planned and the patient was prepared accordingly. Posterior decompression was done at D9-D10 level and pedicle screws were put in D7 and D8 level and the connecting rods interconnected to the previous rods at a lower level (Fig. 6). Post-operative stay was uneventful and the patient was discharged on post-operative day 4.
Based on the clinicoradiological findings, the patient was diagnosed with D9-D10 tubercular spondylitis with cord compression and neural deficits. Revision surgery was planned and the patient was prepared accordingly. Posterior decompression was done at D9-D10 level and pedicle screws were put in D7 and D8 level and the connecting rods interconnected to the previous rods at a lower level (Fig. 6). Post-operative stay was uneventful and the patient was discharged on post-operative day 4.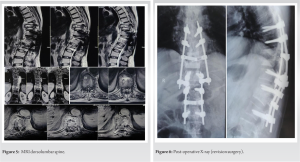
In the herein report, we present a rare case of recurrence of TB spine with neurological involvement in an adjacent segment in a post-operative case who was in the last phase of 18-month course of ATT. To the best of our knowledge, this is the first report of such a case in the anglophonic, contemporary orthopedic literature. We believe the resultant increased vascularity in segments adjacent to instrumented segments predispose them to TB recurrence. Yin et al. in their study about the reasons and the treatment of post-operative relapse of spinal TB found a recurrence rate of 9% [9]. Moreover, he gave certain factors that are associated with increased risk of TB spine recurrence: Malnutrition, non-standard chemotherapy, non-radical debridement, immobilization, and inappropriate surgical indications. Initial, good clinical response to the chemotherapy formed the basis to rule out multidrug-resistant TB. However, in this study, no case of a recurrence at a different spinal segment was reported. Another study from China reported that the duration of pre-operative chemotherapy is not associated with increased risk of post-operative relapse or non-healing disease [10].
TB recurrence in subjacent spinal segments in an already operated case who was on long-term chemotherapy is a rare presentation of a common disease. Reporting this case aims to enlighten clinicians about its clinical implications and management. This case makes clinicians wary of an unusual presentation of common disease and needs urgent intervention to prevent further deterioration.
To make physicians aware of the clinical features and implications of this unusual presentation of spinal TB in a post-operative case on anti-tubercular therapy.
References
- 1.Taylor GM, Murphy E, Hopkins R, Rutland P, Chistov Y. First report of Mycobacterium bovis DNA in human remains from the Iron Age. Microbiology (Reading) 2007;153:1243-9. [Google Scholar]
- 2.Fuentes Ferrer M, Gutiérrez Torres L, Ayala Ramírez O, Rumayor Zarzuelo M, del Prado González N. Tuberculosis of the spine. A systematic review of case series. Int Orthop 2012;36:221-31. [Google Scholar]
- 3.Tuli SM. Tuberculosis of the spine: A historical review. Clin Orthop Relat Res 2007;460:29-38. [Google Scholar]
- 4.Lan X, Liu XM, Ge BF. Debridement and bone grafting with internal fixation via anterior approach for treatment of cervicothoracic tuberculosis. Int Surg 2011;96:358-62. [Google Scholar]
- 5.Yang L, Liu Z. Analysis and therapeutic schedule of the postoperative recurrence of bone tuberculosis. J Orthop Surg Res 2013;8:47. [Google Scholar]
- 6.Ling T, Liu L, Yang X, Qiang Z, Hu X, An Y. Revision surgery for spinal tuberculosis with secondary deformity after treatment with debridement, instrumentation, and fusion. Eur Spine J 2015;24:577-85. [Google Scholar]
- 7.Wang B, Kong L, Zhu Z, Gao W, Guo H, Wang X, et al. Recurrent complex spinal tuberculosis accompanied by sinus tract formation: Causes of recurrence and clinical treatments. Sci Rep 2018;8:6933. [Google Scholar]
- 8.Afshar B, Carless J, Roche A, Balasegaram S, Anderson C. Surveillance of tuberculosis (TB) cases attributable to relapse or reinfection in London, 2002-2015. PLoS One 2019;14:e0211972. [Google Scholar]
- 9.Yin XH, Liu ZK, Hao D. The reasons and clinical treatments of postoperative relapse of Pott’s disease. Medicine (Baltimore) 2018;97:e12471. [Google Scholar]
- 10.Ren HL, Jiang JM, Wang JX, Qu DB, Chen JT. Is duration of preoperative anti-tuberculosis treatment a risk factor for postoperative relapse or non-healing of spinal tuberculosis? Eur Spine J 2016;25:3875-83. [Google Scholar]








