Calcium deposits can be seen in the medial collateral ligament (MCL) following trauma but atraumatic calcific tendinitis is rare. Diagnosis and treatment of MCL calcific tendinitis are not well covered in orthopedic literature. Good resolution of symptoms using conservative treatments is reported.
Dr. Carter J Berry, Department of Orthopaedic Surgery, University of Virginia, Charlottesville, Virginia, United States. E-mail: carterberry434@gmail.com
Introduction: Calcific tendinitis is a commonly treated in the shoulder and wrist, but it is rarely seen in the medial collateral ligament (MCL). There is not satisfactory orthopedic literature for diagnosis and treatment of this condition.
Case Report: A healthy 50-year-old woman presented with medial sided right knee pain. She did not have any history of trauma to the knee nor instability. She was diagnosed with calcific tendinitis of her MCL and was treated with US-guided lavage. This was her 4th documented location of symptomatic calcific tendinitis including her right shoulder, left wrist, and contralateral knee MCL.
Conclusions: We present a case of a 50-year-old female with a history of multifocal, symptomatic calcific tendinitis, who had atraumatic mineral deposition in her MCL. Ultrasound-guided lavage is a successful minimally invasive treatment for calcific tendinitis.
Keywords: Medial collateral ligament, calcific tendinitis, hydroxyapatite, knee.
Calcific tendinitis is an inflammatory condition related to the deposition of calcium hydroxyapatite crystals within tendinous structures. The disease is most common in the shoulder and hip; however, any joint is at risk [1]. The exact pathophysiology of calcific tendinitis remains unknown. There are suggestions of a relationship with endocrine disorders or extracellular organelles such as matrix vesicles [2, 3]. Typically calcific tendinitis is managed conservatively, but surgical interventions have been described for lesions recalcitrant to non-operative management [4]. Calcific tendinitis is usually diagnosed on radiographs, which is the most practical modality for initial evaluation [5]. The medial collateral ligament (MCL) is the primary medial stabilizer of the knee and is made of superficial and deep portions with consistent attachment points on the femur and tibia [6, 7]. It is important to differentiate idiopathic MCL calcific tendinitis versus calcium deposits that are present as a result of trauma or a previous valgus force MCL injury, known as a Pellegrini-Stieda lesion [8]. To the best of our knowledge, there have been no case reports of calcific tendinitis in the medial periarticular region of the knee treated successfully with US-guided lavage. We present a case of a 50-year-old woman with focal knee pain due to calcium hydroxyapatite deposition in her MCL.
A 50-year-old female presented with 1.5 years of right, medial sided knee pain interfering with sleep, and sitting for long periods. She denied any history of injury but felt some gradually worsening medial knee pain with everyday activities despite use of over the counter non-steroidal anti-inflammatory drugs (NSAIDs). Her history is significant in that she had the same symptoms on the left knee for which she had a lavage procedure 5 years ago which provided complete relief. In addition, she was treated similarly for calcific tendinitis in her left wrist following a traumatic fall onto her outstretched left arm 4 years ago. Imaging demonstrated a lobular radio-density along the extensor tendons of the dorsal wrist that was favored to represent calcific tendinosis and hydroxyapatite deposition. She was treated with splinting, US-guided lavage, and NSAIDs and her symptoms fully resolved.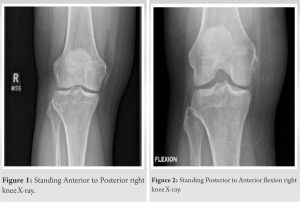
Procedural findings
The patient underwent evaluation using gray scale and color Doppler sonographic imaging where a large focus of calcium hydroxyapatite at the superior attachment of the MCL was found which measured approximately 2 cm in length with adjacent hyperemia. Utilizing local anesthesia, sterile technique, and ultrasound (US) guidance, an 18-gauge needle was advanced into the calcification within the right MCL. Following this, pump lavage and aspiration were performed with a solution of 5 cc of 0.25% preservative free bupivacaine and 5 cc of sterile saline. Three syringes were utilized. This yielded return of amorphous, chalky fluid. All needles were removed. Subsequently, a 25-gauge needle was advanced superficial to the MCL utilizing local anesthesia, sterile technique, and US guidance. A mixture of 1 cc of 0.25% preservative free bupivacaine and 0.5 cc (20 mg) of triamcinolone 40 mg/mL was injected. The patient felt immediate pain relief and tolerated the procedure well.
Post-procedural course
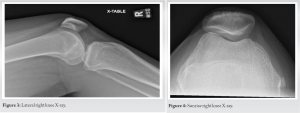
At 4 months post-procedure, she continued to report no pain and was able to return to all activities without issue, sleep was no longer pain limited. In addition to resolution of symptoms in her knee, the patient reported no recurrence of pain or dysfunction in her wrist, contralateral knee, or shoulder at over 3 years follow-up. Her physical examination was symmetric and unremarkable. She had full pain free range of motion without effusion or lower extremity edema. She remained stable to varus and valgus stress at 0 and 30° of flexion without discomfort. She had no tenderness about the medial or lateral aspects of her knee. Standing PA, Rosenberg, and sunrise X-ray views of both knees demonstrated interval resolution of calcium deposits within the MCL (Fig. 5 and 6).
We present this case of a patient with a history of multi-focal calcific tendinitis with treatment of calcific tendinitis in the MCL. This presentation of knee pain from calcific tendinitis is unique and US-guided injection with lavage proved an effective option for treatment. X-ray views showing well-maintained joint space and no soft-tissue swelling along with the absence of joint line tenderness rule out osteoarthritis as a diagnosis in this case. The lobular calcification within the proximal, medial periarticular region of the MCL origin makes MCL calcific tendinitis the most likely diagnosis. Calcific tendinitis predominantly presents as shoulder pain with deposits found most commonly in the tendons of the rotator cuff. Non-operative management is the gold standard with recalcitrant lesions requiring operative intervention. This patient’s multi-focal calcific tendinitis and atraumatic MCL calcific tendinitis is a unique presentation. Few studies have commented on the treatment of MCL calcific tendinitis; however, Fernández-Cuadros et al. [9] described a 64-year-old woman who underwent radial electroshock wave therapy plus iontophoresis which objectively improved her pain and was effective in decreasing the calcification present after treatment. The authors did not state the frequency or length of treatments required for a successful outcome. Kamawal et al. [10] described another 50-year-old woman with MCL calcific tendinitis and simultaneous shoulder calcific tendinitis who’s knee was managed conservatively with analgesics, NSAIDs, electro-therapy, and shock wave therapy. These treatment modalities did not provide adequate relief; thus, surgery was recommended. Knee arthroscopy with additional open removal of the calcified lesion was performed. She was full weight-bearing by 2 weeks post-operative and by 4 weeks was pain free. The etiology of calcific tendinitis remains uncertain, and there is a paucity of literature reporting on atraumatic calcific tendinitis in the MCL and treatment options and outcomes. This study provides one such case report to assist with clinical decision making. After failure of comprehensive non-operative interventions, the patient was able to achieve pain relief and return to activity without undergoing a surgical intervention. There remains a need for more robust studies reporting on these topics.
Our patient had a unique symptomatic presentation of multi-focal calcific tendinitis with successful resolution of symptoms using non-surgical measures. She was able to return to all activities and sleep without pain. We report US-guided lavage with aspiration as a successful treatment for MCL calcific tendinitis without any known complications.
MCL calcific tendinitis can be a cause of medial sided knee pain, which is a frequent clinical complaint. Diagnosis and conservative treatment using US-guided lavage is novel in orthopedics. This case provides a new discussion of knee pathology with associated treatment.
References
- 1.Siegal DS, Wu JS, Newman JS, Del Cura JL, Hochman MG. Calcific tendinitis: A pictorial review. Can Assoc Radiol J 2009;60:263-72. [Google Scholar]
- 2.Harvie P, Pollard TC, Carr AJ. Calcific tendinitis: Natural history and association with endocrine disorders. J Shoulder Elbow Surg 2007;16:169-73. [Google Scholar]
- 3.Burner T, Gohr C, Mitton-Fitzgerald E, Rosenthal AK. Hyperglycemia reduces proteoglycan levels in tendons. Connect Tissue Res 2012;53:535-41. [Google Scholar]
- 4.Ark JW, Flock TJ, Flatow EL, Bigliani LU. Arthroscopic treatment of calcific tendinitis of the shoulder. Arthroscopy 1992;8:183-8. [Google Scholar]
- 5.Faure G, Daculsi G. Calcified tendinitis: A review. Ann Rheum Dis 1983;42 Suppl 1:49-53. [Google Scholar]
- 6.Warren LA, Marshall JL, Girgis F. The prime static stabilizer of the medical side of the knee. J Bone Joint Surg Am 1974;56:665-74. [Google Scholar]
- 7.LaPrade RF, Engebretsen AH, Ly TV, Johansen S, Wentorf FA, Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am 2007;89:2000-10. [Google Scholar]
- 8.Altschuler EL, Bryce TN. Images in clinical medicine. Pellegrini-Stieda syndrome. N Engl J Med 2006;354:e1 [Google Scholar]
- 9.Fernández-Cuadros ME, Albaladejo-Florín MJ, Álava-Rabasa S, Pérez-Moro OS. Calcification of the medial collateral ligament of the knee: Rehabilitative management with radial electro shock wave therapy plus iontophoresis of a rare entity. Clinical case and review. Rehabilitacion (Madr) 2022;56:388-94. [Google Scholar]
- 10.Kamawal Y, Steinert AF, Holzapfel BM, Rudert M, Barthel T. Case report-calcification of the medial collateral ligament of the knee with simultaneous calcifying tendinitis of the rotator cuff. BMC Musculoskelet Disord 2016;17:283. [Google Scholar]









