Management of closed mallet thumb injury. Comparison between the outcomes of various studies of mallet thumb injuries.
Dr. Harshitha S Reddy, Department of Orthopaedic Surgery, MS Ramaiah Medical College, Bengaluru - 560 054, Karnataka, India. E-mail: harshitha7reddy@gmail.com
Introduction: Mallet thumb injuries are uncommon. Traumatic avulsion injury of the extensor pollicis longus leads to significant difficulty.
Case Report: A 55-year-old male patient presented with a closed hyper flexion injury to the thumb, resulting in pain and loss of active extension. Clinical examination and x-rays confirmed a soft-tissue mallet injury. The patient was treated non-operatively by immobilizing the interphalangeal joint of the thumb. The patient regained full range of motion.
Conclusion: Non-operative treatment for acute closed mallet injury of the thumb provides satisfactory outcomes. It is suitable when a patient presents acutely.
Keywords: Mallet thumb injury, closed thumb injury, Extensor pollicis longus rupture, mallet finger injury.
Traumatic avulsion injury of the extensor pollicis longus (EPL) leads to significant disability. Very few cases of closed soft tissue mallet thumb injuries have been reported in the literature. About 2% of all mallet injuries occur in the thumb [1]. Both surgical and non-surgical management have been reported for this injury. Due to the rarity of the injury, standardized protocol for treatment is unavailable, and despite the course of treatment, the patient must be educated on the failure of conservative treatment [2].
A 55-year-old, dominant right-hand male patient presented to the outpatient clinic with pain and an inability to extend his right thumb 2 days post-injury. The patient sustained a hyper flexion injury while helping his daughter finish a do-it-yourself project. The patient’s chief complaint was loss of active extension and pain. On examination, the injury was closed, and the thumb was in 30° of flexion at the interphalangeal joint (IPJ). The patient had moderate swelling and tenderness around the IPJ. While the patient was able to flex at the IPJ, he was unable to actively extend the thumbs. The X-ray showed no fractures or osseous defects. Based on the clinical examination and no evidence of bony injuries, it was deemed to be a closed mallet thumb injury. The injury was managed conservatively. A malleable aluminum splint was used to immobilize the IPJ. The splint was placed full-time for a period of 8 weeks and was followed by 4 weeks of night-only splinting. The patient was advised to maintain the position of the thumb when the splint was taken off. A 12-week follow-up had positive outcomes as the normal range of movement of his right thumb was restored. During the final follow-up at 12 months, examination of the EPL showed normal power. The patient showed no extension lag. The patient was confirmed to have an excellent Crawford’s score.
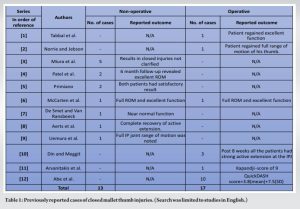
A literature review (in English) on Mallet thumb over the last 40 years has been summarized in Table 1 [1-12]. A total of seven [3-9] studies (Table 1) had satisfactory results with non-operative treatment. Miura et al. [3] reported that patients who received treatment within 2 weeks of the reported injury had better outcomes compared to those treated after the initial 2 week period.
The study noted perfect extension in 84% of cases where the splint was placed for the entire day for 4–6 weeks and later reduced to 8–12 h for the following 3–6 months. Patel et al. [4] successfully managed to achieve a satisfactory outcome with a Stack splint, immobilizing only the IPJ for 8 weeks, followed by 2 weeks of night splinting. At the 6-month follow-up, all patients in their series had a satisfactory outcome. These case reports agree with the remaining articles about the efficacy of non-operative treatment for closed mallet thumb injuries [3-9]. Differential diagnoses of closed soft tissue mallet injury include
- Seymour fracture
- Osteoarthritis
- Rheumatoid arthritis is a swan-neck deformity.
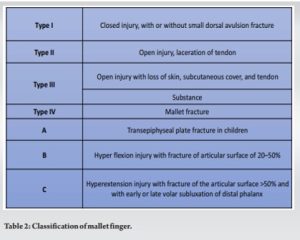
We found six [1, 2, 6, 10-12] studies (Table 1) where surgery was the preferred mode of treatment. Two were due to tendinous gaps [1, 11], and two were due to delayed presentation [2, 6]. A systematic review by Abe et al. [12] reported a shorter duration of immobilization for surgically treated mallet thumb injuries (4.9 weeks for surgery vs. 9.5 for weeks non-surgical). Surgical methods include placing sutures on the EPL with various kinds of core sutures and epitendinous sutures. In cases where the EPL tendon detaches from the distal phalangeal bone, it is reattached with suture anchors and epitendinous sutures. After the incision is closed, the IPJ is immobilized by either a splint or Kirschner wire (K-wire) for a period of 4–6 weeks. Parameters like QuickDASH score, range of motion, and immobilization method did not show significant differences between different treatment modalities. Doyle [14] classified mallet injuries into four types, as explained in Table 2.
Our report discusses the management of a type 1 mallet injury and a literature review of closed injuries without bony avulsion. Tabbal et al. [1] recommend a routine MRI to enable early identification of cases with large tendinous gaps. Imaging may help in making better decisions for treatment. Platelet-rich plasma (PRP) and stem cells are being increasingly utilized in the management of tendon pathology. A meta-analysis and systematic review by Chen et al. [13] looked at the efficacy of PRP on tendon healing. The review shows it may provide both short-term and long-term pain relief for tendon and ligament injuries. We recommend further studies to look at the role of PRP and other biologics in the treatment of this uncommon injury.
Non-operative treatment for an acute closed mallet injury of the thumb provides satisfactory outcomes. It is suitable when a patient presents acutely.
Soft-tissue mallet thumb is an uncommon condition. Clinical examination and X-ray evaluation can confirm the difference between soft tissue and bony mallet injuries. When detected early, this condition may be successfully treated conservatively with good outcomes.
References
- 1.Tabbal GN, Bastidas N, Sharma S. Closed mallet thumb injury: A review of the literature and case study of the use of magnetic resonance imaging in deciding treatment. Plast Reconstr Surg 2009;124:222-6. [Google Scholar]
- 2.Norrie BA, Jebson PJ. Mallet thumb. J Hand Surg Am 2013;38:1219-21. [Google Scholar]
- 3.Miura T, Nakamura R, Torii S. Conservative treatment for a ruptured extensor tendon on the dorsum of the proximal phalanges of the thumb (mallet thumb). J Hand Surg Am 1986;11:229-33. [Google Scholar]
- 4.Patel MR, Lipson LB, Desai SS. Conservative treatment of mallet thumb. J Hand Surg Am 1986;11:45-7. [Google Scholar]
- 5.Primiano GA. Conservative treatment of two cases of mallet thumb. J Hand Surg Am 1986;11:233-5. [Google Scholar]
- 6.McCarten GM, Bennett CS, Marshall DR. Treatment of mallet thumb. Aust N Z J Surg 1986;56:285-6. [Google Scholar]
- 7.De Smet L, Van Ransbeeck H. Mallet thumb. Acta Orthop Belg 2003;69:77-8. [Google Scholar]
- 8.Aerts BR, Somford MP, Beumer A. Mallet thumb: Report of a case. OA Case Rep 2014;2:156. [Google Scholar]
- 9.Uemura T, Kazuki K, Hashimoto Y, Takaoka K. Skiing-induced rupture of the extensor pollicis longus tendon: A report of three cases. Clin J Sport Med 2008;18:292-4. [Google Scholar]
- 10.Din KM, Meggitt BF. Mallet thumb. J Bone Joint Surg Br 1983;65:606-7. [Google Scholar]
- 11.Arvanitakis M, Calcagni M, Giesen T. Closed mallet thumb injury treated surgically: A case report. Case Reports Plast Surg Hand Surg 2017;4:27-9. [Google Scholar]
- 12.Abe Y, Rokkaku T, Tokunaga S, Yamada T, Okamoto S. Closed mallet thumb injury: Our experience of 10 patients treated with surgery and a systematic review. J Plast Reconstr Aesthet Surg 2016;69:835-42. [Google Scholar]
- 13.Chen X, Jones IA, Park C, Vangsness CT Jr. The efficacy of platelet-rich plasma on tendon and ligament healing: A systematic review and meta-analysis with bias assessment. Am J Sports Med 2018;46:2020-32. [Google Scholar]
- 14.Doyle JR. Extensor tendons: Acute injuries. In: Green DP, Pederson CW, Hotchkiss RN, editors. Green’s Operative Hand Surgery. 4th ed. New York: Churchill Livingstone; 1999. p. 195-8. [Google Scholar]