Recurrent soft-tissue swelling after limb surgery should arise the suspicion of arterial pseudoaneurysm.
Dr Gaurav Kumar Upadhyaya, Department of Orthopaedics, AIIMS, Raebareli, Uttar Pradesh, India. E-mail: drgkupadhyaya@yahoo.co.in
Introduction: Arterial pseudoaneurysm is a hematoma that is formed after damage to the arterial wall. We report a rare case of peroneal artery pseudoaneurysm after open reduction and internal fixation with interlocking nailing and partial fibulectomy for non-union for the right tibia in a 31-year-old male. The patient presented with a bleeding sinus over the leg swelling, and it was managed with an exploration of the pseudoaneurysm and ligation of the peroneal artery.
Case Report: A 30-year-old male patient presented with a non-union tibia on the right side and had undergone plating of the tibia at another institute for a fracture of both bone legs approximately 18 months ago. The revision surgery was performed in which a previously inserted implant was removed and an interlocking nail was inserted, along with a partial fibulectomy. The post-operative period was uneventful. At 8 weeks after the second surgery, the patient came with a complaint of swelling at the outer aspect of the right leg. Computed tomography and angiography confirmed a peroneal artery pseudoaneurysm of 3.2 × 2.8 × 3.8 cm. Pseudoaneurysm was explored, and the artery was overrun with a Figure-8 stitches using a monofilamentous, and non-absorbable suture.
Conclusion: This case report highlights the occurrence of pseudoaneurysm after an orthoapedic procedure such as a partial fibulectomy. A high level of clinical suspicion, proper imaging, and early endovascular or surgical intervention is recommended to prevent complications.
Keywords: Pseudoaneurysm, peroneal artery, partial fibulectomy.
Arterial pseudoaneurysm is a hematoma that is formed after damage to the arterial wall. The covering of pseudoaneurysm does not include all three layers of the arterial wall; instead, it is formed by the clotting products and surrounding tissue. Arterial pseudoaneurysm is formed either after trauma or infection. Trauma, either blunt or penetrating, may cause damage to the arterial wall and contribute to the formation of pseudoaneurysms [1,2]. Peroneal artery pseudoaneurysm is a rare entity. We report a rare case of peroneal artery pseudoaneurysm after open reduction, internal fixation with interlocking nailing, and partial fibulectomy for non-union of right, tibia in a 31-year-old male. The patient presented with a bleeding sinus over the leg swelling, and it was managed with an exploration of the pseudoaneurysm and ligation of the peroneal artery.
The patient, a healthy male in his early thirties, sustained a fracture of the right tibia and fibula, for which he underwent plating of the tibia at another institute. Following the non-union of the tibia, he sought a second opinion with us approximately 18 months after his index surgery. Radiographs confirmed the diagnosis of non-union of the right tibia with the plate in situ (Fig. 1).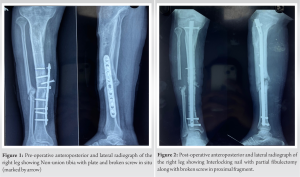 The revision surgery was performed, in which plate and screws were removed from the medial approach. One screw was found broken in the proximal fragment. An attempt was made to remove the broken screw, but it could not be removed. A longitudinal lateral incision was made along the fibular shaft at mid-leg level. Soft-tissue dissection was done. The fibula was exposed, and a partial fibulectomy with the removal of approximately 1.5 cm of fibula was performed. Antegrade insertion of an interlocking nail was performed after reaming, followed by proximal and distal locking (Fig. 2). The post-operative period was uneventful. The patient was discharged after 7 days, and stitches were removed after 2 weeks. At 8 weeks after the second surgery, the patient came with a complaint of swelling at the outer aspect of the right leg (Fig. 3).
The revision surgery was performed, in which plate and screws were removed from the medial approach. One screw was found broken in the proximal fragment. An attempt was made to remove the broken screw, but it could not be removed. A longitudinal lateral incision was made along the fibular shaft at mid-leg level. Soft-tissue dissection was done. The fibula was exposed, and a partial fibulectomy with the removal of approximately 1.5 cm of fibula was performed. Antegrade insertion of an interlocking nail was performed after reaming, followed by proximal and distal locking (Fig. 2). The post-operative period was uneventful. The patient was discharged after 7 days, and stitches were removed after 2 weeks. At 8 weeks after the second surgery, the patient came with a complaint of swelling at the outer aspect of the right leg (Fig. 3). On examination, there was fullness at the outer aspect of the mid-leg, which was warm, tender, and fluctuant. The swelling was non-pulsatile. The foot was warm, distal pulses were palpable, and there was no neurological deficit. There was no history of fever. A clinical diagnosis of an abscess was made. 20 mL of serosanguinous fluid was aspirated and sent for culture. The patient was prescribed anti-inflammatory medications and antibiotics. The culture was sterile. The patient again presented after 1 month with a discharging sinus at the site of aspiration. Around 30 mL of serosanguinous fluid was aspirated, and a sample for Gram stain and culture sensitivity was sent. A compression bandage was applied. Swelling subsided with repeat aspiration and a compression bandage. Culture reported methicillin-resistant coagulase-negative Staphylococci sensitive to linezolid.
On examination, there was fullness at the outer aspect of the mid-leg, which was warm, tender, and fluctuant. The swelling was non-pulsatile. The foot was warm, distal pulses were palpable, and there was no neurological deficit. There was no history of fever. A clinical diagnosis of an abscess was made. 20 mL of serosanguinous fluid was aspirated and sent for culture. The patient was prescribed anti-inflammatory medications and antibiotics. The culture was sterile. The patient again presented after 1 month with a discharging sinus at the site of aspiration. Around 30 mL of serosanguinous fluid was aspirated, and a sample for Gram stain and culture sensitivity was sent. A compression bandage was applied. Swelling subsided with repeat aspiration and a compression bandage. Culture reported methicillin-resistant coagulase-negative Staphylococci sensitive to linezolid. Antibiotics were started according to the culture and sensitivity report. The patient presented again after a gap of 1 week with a complaint of blood loss through the sinus after a walk of approximately 1 km. A Doppler study was advised, and it showed a hematoma of 10 × 5 cm in size with a peroneal artery pseudoaneurysm of 4 × 3 × 3 cm in size. Computed tomography (CT) angiography further delineated the peroneal artery pseudoaneurysm of 3.2 ´ 2.8 ´ 3.8 cm, approximately 17 cm distal to the knee joint (Fig. 4 and 5).
Antibiotics were started according to the culture and sensitivity report. The patient presented again after a gap of 1 week with a complaint of blood loss through the sinus after a walk of approximately 1 km. A Doppler study was advised, and it showed a hematoma of 10 × 5 cm in size with a peroneal artery pseudoaneurysm of 4 × 3 × 3 cm in size. Computed tomography (CT) angiography further delineated the peroneal artery pseudoaneurysm of 3.2 ´ 2.8 ´ 3.8 cm, approximately 17 cm distal to the knee joint (Fig. 4 and 5).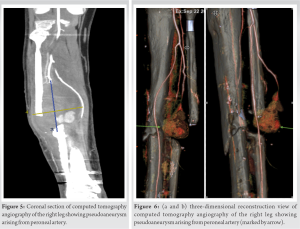 Patient’s hemoglobin was 7.4 g%. It may be assumed that bleeding pseudoaneurysms will cause anemia. Two units of packed red blood cells were transfused. The patient was optimized, and pseudoaneurysm was explored under tourniquet control. A large pseudoaneurysm was noted, with layered clots and a 0.5 cm rent in the wall of the peroneal artery. Clots were evacuated. Due to the friable nature of the tissues around the peroneal artery opening, the artery was overrun with a Fig. 8 stitch, using monofilamentous non-absorbable suture. The cavity was thoroughly irrigated and packed. The pack was removed on the 2nd post-operative day. Secondary closure was performed after 4 days. Sutures were removed after 14 days. Tibia is united at 1-year follow-up, and the patient is asymptomatic now at 1-year follow-up (Fig. 6 and 7).
Patient’s hemoglobin was 7.4 g%. It may be assumed that bleeding pseudoaneurysms will cause anemia. Two units of packed red blood cells were transfused. The patient was optimized, and pseudoaneurysm was explored under tourniquet control. A large pseudoaneurysm was noted, with layered clots and a 0.5 cm rent in the wall of the peroneal artery. Clots were evacuated. Due to the friable nature of the tissues around the peroneal artery opening, the artery was overrun with a Fig. 8 stitch, using monofilamentous non-absorbable suture. The cavity was thoroughly irrigated and packed. The pack was removed on the 2nd post-operative day. Secondary closure was performed after 4 days. Sutures were removed after 14 days. Tibia is united at 1-year follow-up, and the patient is asymptomatic now at 1-year follow-up (Fig. 6 and 7). In this case report, it is postulated that the peroneal artery was partially injured during a partial fibulectomy, either by drill bit or osteotome. The injury may have caused the artery to go into spasm, due to which it went unrecognized during surgery and formed a pseudoaneurysm in due course of time.
In this case report, it is postulated that the peroneal artery was partially injured during a partial fibulectomy, either by drill bit or osteotome. The injury may have caused the artery to go into spasm, due to which it went unrecognized during surgery and formed a pseudoaneurysm in due course of time.
Review of Literature
On searching the English literature, 16 cases of traumatic pseudoaneurysm of the peroneal artery or perforating branches of the peroneal artery have been reported. However, only eight case reports out of those have proposed the cause of pseudoaneurysm of the peroneal artery or perforating branch of the peroneal artery as an iatrogenic injury during surgery [3-10] Table 1.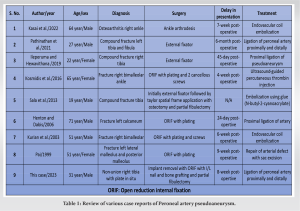 Pseudoaneurysm of the peroneal artery is a rare entity. Pseudoaneurysm covering does not have all three layers of the arterial wall as found in true aneurysm. This makes the aneurysm sac weaker and prone to rupture. Aneurysms connect to the parent artery through a narrow opening. The diameter of this opening is small as compared to the aneurysm sac. Blood enters the aneurysm sac during systole and leaves the sac during diastole. However, when emptying of the sac is incomplete, it leads to the expansion of aneurysm and complications of bleeding. This may occur when an intimal flap tear acts as a valve, preventing the complete emptying of the aneurysm sac during diastole [1]. Traumatic pseudoaneurysms are the most common. It can be either a blunt or penetrating injury. Penetrating trauma in the form of injury by intravenous drug abuse, vascular interventions, fracture ends, or orthopedic surgical interventions including manipulation of fractures, drill bits, osteotomes, or screws is the reasons for the pathogenesis of pseudoaneurysm [4, 11, 12]. Traumatic arterial pseudoaneurysm has a male preponderance. The most common clinical presentation is painful swelling followed by pulsatile mass and painful pulsatile mass. The clinical presentation may vary with the location and size of the pseudoaneurysm as well as the presence of surrounding structures. The median time delay in the clinical presentation is 30 days. Accompanying clinical findings may include systolic bruit, thrill, and ecchymosis. Approximately 20% of the patients may have complications such as nerve palsy, compartment syndrome, and rupture [4, 11]. In this case, it is also reported that the location of aneurysms in close proximity may cause pressure necrosis on the surrounding skin and can lead to infection and sinus formation. In cases of secondary infection of pseudoaneurysm, staphylococcus aureus is the most common organism to colonize the wound, followed by Escherichia coli and Pseudomonas [12]. Recurrent bleeding in the pseudoaneurysm may also lead to anemia, as reported in this case report.
Pseudoaneurysm of the peroneal artery is a rare entity. Pseudoaneurysm covering does not have all three layers of the arterial wall as found in true aneurysm. This makes the aneurysm sac weaker and prone to rupture. Aneurysms connect to the parent artery through a narrow opening. The diameter of this opening is small as compared to the aneurysm sac. Blood enters the aneurysm sac during systole and leaves the sac during diastole. However, when emptying of the sac is incomplete, it leads to the expansion of aneurysm and complications of bleeding. This may occur when an intimal flap tear acts as a valve, preventing the complete emptying of the aneurysm sac during diastole [1]. Traumatic pseudoaneurysms are the most common. It can be either a blunt or penetrating injury. Penetrating trauma in the form of injury by intravenous drug abuse, vascular interventions, fracture ends, or orthopedic surgical interventions including manipulation of fractures, drill bits, osteotomes, or screws is the reasons for the pathogenesis of pseudoaneurysm [4, 11, 12]. Traumatic arterial pseudoaneurysm has a male preponderance. The most common clinical presentation is painful swelling followed by pulsatile mass and painful pulsatile mass. The clinical presentation may vary with the location and size of the pseudoaneurysm as well as the presence of surrounding structures. The median time delay in the clinical presentation is 30 days. Accompanying clinical findings may include systolic bruit, thrill, and ecchymosis. Approximately 20% of the patients may have complications such as nerve palsy, compartment syndrome, and rupture [4, 11]. In this case, it is also reported that the location of aneurysms in close proximity may cause pressure necrosis on the surrounding skin and can lead to infection and sinus formation. In cases of secondary infection of pseudoaneurysm, staphylococcus aureus is the most common organism to colonize the wound, followed by Escherichia coli and Pseudomonas [12]. Recurrent bleeding in the pseudoaneurysm may also lead to anemia, as reported in this case report.
Doppler ultrasound, arteriography, CT angiography, and magnetic resonance imaging (MRI) can be used for diagnosing pseudoaneurysm. The Doppler study is the first line investigation to be performed for confirming the diagnosis. It has the advantage of being inexpensive, radiation-free, quick, portable, and non-invasive. However, the disadvantage is that it is operator-dependent and cannot provide three-dimensional images for assessment. CT angiography provides more information about the pseudoaneurysm but carries the risk of high radiation doses. Arteriography is an invasive investigation but has the advantage of being therapeutic in performing endovascular procedures. MRI is also an excellent investigation in providing the required anatomical details but is costly, time-consuming, and difficult to perform in the presence of metallic implants [4, 11, 12]. Various treatment modalities have been described in the literature, ranging from conservative ultrasound-guided thrombin injection to endovascular procedures such as coil/glue embolization or intraluminal stent placement, ligation of the artery, arterial repair, and arterial reconstruction [4, 6, 9, 11, 12, 13]. As the pseudoaneurysm is usually full of layers of clots, the size of the true cavity is often grossly underestimated on color on Doppler and angiograms. Open surgery provides the benefit of clot evacuation and the management of elements of local infection (if any) over endovascular procedures. Surgery for distal pseudoaneurysms carries low morbidity and mortality while remaining simple, expeditious, and curative. Pseudoaneurysms of vessels that may require laparotomy or thoracotomy or in moribund patients may benefit more from endovascular interventions.
This case report highlights the occurrence of a pseudoaneurysm after an orthopedic procedure such as a partial fibulectomy. Delayed presentation and non-specific complaints make it challenging to diagnose. A high level of clinical suspicion, proper imaging, and early endovascular or surgical intervention is recommended to prevent complications.
It is that high index of suspicion is required for the diagnosis of arterial pseudoaneurysm of peroneal artery after surgery involving the leg.
References
- 1.Kronzon I. Diagnosis and treatment of iatrogenic femoral artery pseudoaneurysm: A review. J Am Soc Echocardiogr 1997;10:236-45. [Google Scholar]
- 2.Sueyoshi E, Sakamoto I, Nakashima K, Minami K, Hayashi K. Visceral and peripheral arterial pseudoaneurysms. AJR Am J Roentgenol 2005;185:741-9. [Google Scholar]
- 3.Kasai T, Higashida T, Hayashi T, Yasui T. Pseudoaneurysm of the peroneal artery after ankle arthrodesis treated by endovascular coil embolization: A case report. JBJS Case Connect 2022;12(3):doi: 10.2106/JBJS.CC.22.00206. . [Google Scholar]
- 4.Pathinathan K, Sivakumaran D, Dimantha WH, Nishanthan AA, Chanaka KA, Munidasa D. Late-onset pseudoaneurysms of lower limb arteries following late complications of orthopaedic constructs-two cases and review of literature. Int J Surg Case Rep 2021;87:106457. [Google Scholar]
- 5.Ileperuma MR, Hewavithana B. Proximal peroneal artery traumatic pseudoaneurysm following a compound proximal tibial shaft fracture managed with an external fixator: A case report. J Orthop Trauma Rehabil 2020;27:89-92. [Google Scholar]
- 6.Kosmidis IA, Kourkoutas K, Stouki S, Flokatoula M. Pseudoaneurysm of the perforating peroneal artery after ankle fracture fixation: Case report and review of the literature. J Foot Ankle Surg 2016;55:1083-6. [Google Scholar]
- 7.Sala F, Salerno CF, Albisetti W. Pseudoaneurysm of the peroneal artery: An unusual complication of open docking site procedure in bone transport with taylor spatial frame. Musculoskelet Surg 2013;97:183-6. [Google Scholar]
- 8.Henton J, Dabis HS. Pseudoaneurysm of the peroneal artery following os calcis fixation. Inj Extra 2006;37:419-21. [Google Scholar]
- 9.Kurian J, Pillai SC, Chapple D, Frost RA. Pseudoaneurysm of peroneal artery following ankle fracture. Foot Ankle Surg 2003;9:233-5. [Google Scholar]
- 10.Pai VS. Traumatic aneurysm of the perforating peroneal artery following ankle fracture. J Foot Ankle Surg 1999;38:417-9. [Google Scholar]
- 11.Raherinantenaina F, Rajaonanahary TM, Ratsimba HN. Management of traumatic arterial pseudoaneurysms as a result of limb trauma. Formos J Surg 2016;49:89-100 [Google Scholar]
- 12.Luther A, Kumar A, Negi KN. Peripheral arterial pseudoaneurysms-a 10-year clinical study. Indian J Surg 2015;77 Suppl 2:603-7. [Google Scholar]
- 13.Gangadharan AN, Sekhar R, Bhanushali JP, Thusay PC. Pseudoaneurysm of posterior tibial artery management: Case report and review of literature. J Curr Surg 2015;5:209-12. [Google Scholar]











