Foreign bodies should be kept as a differential in cases presenting as osteomyelitis, especially in the Indian scenario and the same is important for an orthopedic surgeon while taking history, ordering radiological investigations, and debriding such wounds.
Dr. Ansh Gupta Department of Orthopaedics, Postgraduate Institute of Medical Education and Research, Chandigarh, India. E-mail: Anshgupta770@gmail.com
Introduction: The first differential diagnosis for a chronic discharging sinus on an extremity is usually chronic osteomyelitis. These patients are usually treated with surgical debridement and intravenous antibiotics. However, all discharging sinuses are not osteomyelitis.
Case Report: We encountered two such cases, initially treated as osteomyelitis, which did not respond to initial surgical debridement and, on further workup, were found to have foreign bodies in situ that mimicked osteomyelitis. The first case is a 1 ½-year-old child with an intact rubber band inside the wrist, presenting with sinuses on the wrist, and the second one is a 12-year-old with an old penetrating injury to the foot through the sole of a rubber slipper. Both patients recovered completely once the foreign bodies were removed.
Conclusion: We stress the importance of keeping the possibility of a foreign body in mind in patients with discharging sinuses not responding adequately to debridement and antibiotics.
Keywords: Foreign body, rubber band, Dhaga syndrome, osteomyelitis, discharging sinus.
A chronic, discharging sinus is most commonly a manifestation of chronic osteomyelitis. A concomitant history of pain, fever, and intermittent discharge with bony spicules is the usual combination. It is known that children with chronic osteomyelitis often face a lengthy and tedious course of treatment involving repeated surgical debridement and a prolonged course of intravenous antibiotics. However, it is always imperative to keep in mind that not all discharging sinuses are osteomyelitis [1, 2]. A non-healing sinus should warrant further investigation, as a retained foreign body may always be a possible etiology. Specific history should be enquired for, and imaging interpreted to rule out this seemingly innocuous masquerader of chronic osteomyelitis. The previously reported foreign body culprits are thorn pricks, penetrating injuries through slippers or shoes, leaving rubber particles embedded in the foot. The rubber band, or “Dhaga syndrome,” is unique to the Indian and South Asian populations due to socio-cultural beliefs [1]. It may seem unfathomable to forget a constricting thread or rubber band on the wrist of a child. However, such a circumferential constricting foreign body is not only a concern for causing infection; it may also lead to neurovascular compromise [2]. Thus, we intend to depict two such cases who presented to us as chronic osteomyelitis and who underwent prior debridement but did not heal. Once the foreign body was extracted, both patients recovered fully without a recurrence of infection. Our case report presents a rare scenario where surgical debridement was done without keeping in mind the possibility of a foreign body, which led to a second procedure to extract it in both cases.
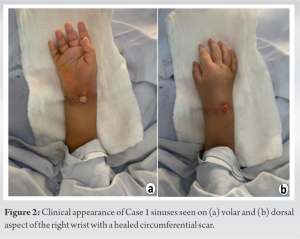
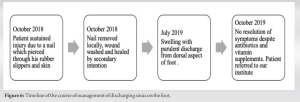
A 1⅟2-year-old male child presented with a circumferential scar over the right wrist with swelling, decreased range of motion, and three discharging sinuses (along the dorsal, volar, and ulnar surfaces), which gradually evolved over the past 6 months (Fig. 1).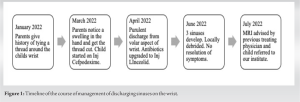
Radiology
X-rays appeared grossly normal (Fig. 3). 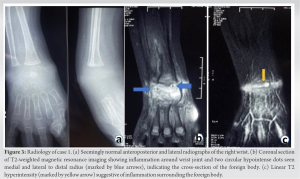
Surgical management
The patient was taken up for the foreign body removal. Dorsal and volar lazy-S-shaped incisions are given. Intraoperatively, no thread was found. However, a rubber band was found, intact, around the proximal row of carpal bones. Two adjacent markings were done, and the band cut and removed to ensure complete removal of the foreign body (Fig. 4).
Post-operative period
Wound cultures revealed methicillin-sensitive staphylococcus aureus and were given 5 days of IV cloxacillin, followed by 1 week of oral cloxacillin 250 mg QID. The wound healed well with no signs of infection or discharge. The patient has no symptoms 6-month post-operatively (Fig. 5). The pointing index has resolved, and the child is able to carry out all routine activities with the affected hand.
Case 2
A 12-year-old boy presented with gradually progressive swelling and a sinus discharging frank pus on the dorsum of the right foot for 3 months, associated with pain and decreased range of motion (Fig. 6). The patient had a history of penetrating injury to the foot due to a nail 11 months ago that pierced through his rubber slippers. The nail was removed at a local hospital, and the patient was given oral clindamycin. The wound healed, and the patient had no complaints in the intervening period. On examination, the child was well nourished. The right foot was swollen, erythematous, and tender with a local rise in temperature. A sinus of diameter 5 mm was present on the dorsal aspect of the third ray with frank pus discharge (Fig. 7). There was no distal neurovascular deficit. Leukocyte counts were normal, and ESR and CRP were borderline.
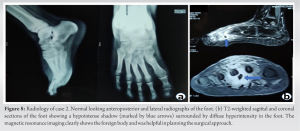
Radiology
X-rays appeared grossly normal (Fig. 8). MRI suggested soft-tissue collection/abscess formation on the palmar and dorsal aspects of the second and third rays in the midfoot region, suggestive of osteomyelitis with overlying soft-tissue edema/cellulitis (Fig. 8). A foreign body was retrospectively identified on the MRI films.
Surgical management
The patient underwent foreign body removal through the plantar approach, along with debridement of the sinus on the dorsal aspect. A continuous tract extending from the plantar to the dorsal aspect thus ensued. The foreign body removed was identified as a part of the rubber slipped, which pierced through the skin along with the nail (Fig. 9).
Postoperative period
Intra-operative cultures were sterile; the patient was given 2 days of IV and 5 days of oral cefuroxime. The patient’s symptoms resolved, and the post-op period was uneventful. The wounds healed successfully. No complaints presently at 3-year follow-up.
Foreign bodies insertion may be traumatic or atraumatic. Metallic and ceramic materials are radio-opaque and can be visualized on plain radiographs. On the other hand, rubber is a radiolucent synthetic, non-biodegradable material capable of inducing a chronic granulomatous response. Atraumatic foreign body insertions may happen, as in the case of “rubber band or Dhaga” syndrome, due to a forgotten thread or rubber band. It is mostly seen in India (due to religious beliefs) and around the wrist joint; however, cases around the ankle have also been reported [1, 3]. The rubber band acts like a self-tightening seton, cutting through the skin, fascia, tendons, and nerves rather than the scarred skin, constricting vascularity and growth of the distal limb [2]. It is usually painless. The skin rapidly re-epithelizes, making diagnosis difficult. A circumferential linear scar associated with a discharging sinus is pathognomonic [4, 5]. However, in the absence of a discharging sinus, it may mimic a congenital constriction ring [6]. Foreign bodies lodged due to trauma may be missed in cases of trivial trauma or distracting major injuries. The risk is higher in children with peripheral neuropathy, intellectual disability, and broken families due to neglect. Foreign bodies tend to incite an inflammatory response [7]. This may lead to pain, swelling, an inability to bear weight, and restricted range of motion in the adjoining joint. These features clinically overlap with osteomyelitis. On examination, fever, erythema, tenderness, and discharging sinus along with elevated pro-inflammatory markers may further channelize the treating physician toward osteomyelitis. Therefore, many such cases are often treated for osteomyelitis through antibiotics and local debridement. Cases may also be treated as tuberculosis, which is endemic in India [4]. Plain radiographs may show periosteal reactions, osteolysis, bony indentation, constriction signs, or even a fracture. However, they may not clearly be able to show a foreign body [5, 8]. USG may help in identifying the foreign body and can also be used to guide removal intraoperatively. Computerized tomography (CT) and MRI should also be taken into consideration for patients who have a vague history of trauma. MRI is the gold standard diagnostic test [6, 9, 10]. MRI helps in delineating the soft anatomy and plans the surgery for retrieval of the foreign body (Fig. 10) [11].
These cases are unique, as they highlight that a foreign body is easy to miss unless a strong clinical suspicion is kept. Both cases reported here were not only treated medically for osteomyelitis but also underwent debridement and wound care, and yet the foreign body was missed, highlighting the evasive and insidious manner of presentation. X-rays may miss the foreign body, and therefore clinicians should use better imaging techniques such as CT and MRI if there is suspicion based on history.
Rubber foreign bodies can easily be missed if proper history is not taken. Cases like the ones presented here may be treated as chronic osteomyelitis for months. Delay in diagnosis can lead to disease progression and permanent damage to neurovascular structures. Management is surgical, with complete removal of the foreign material along with antibiotic cover essential for resolution. History may not always be forthcoming, and the clinician should always keep the differential of a foreign body among suspected cases of osteomyelitis and use appropriate radiological investigations to confirm the same.
References
- 1.John R, Khurana A, Raj NG, Aggarwal P, Kanojia R, Chayapathi V. The ‘forgotten rubber band’ syndrome-a systematic review of a uniquely ‘desi’ complication with a case illustration. J Clin Orthop Trauma 2019;10:822-7. [Google Scholar]
- 2.Kumar PS, Gupta A, Singh RJ. Circumferential scar on wrist of children: An explicit warning sign of rubber band syndrome. Indian J Surg 2022;84:1323-4. [Google Scholar]
- 3.Yang G, Huang Y, Ye W, Yu H, Mei H. A rare case report of acquired rubber band syndrome due to an unnoticed rubber band on a baby’s ankle. Transl Pediatr 2020;9:66-9. [Google Scholar]
- 4.Arora A, Agarwal A. Dhaga syndrome: A previously undescribed entity. J Bone Joint Surg Br 2004;86:282-4. [Google Scholar]
- 5.Agarwal A, Kant KS, Verma I. The rubber band syndrome: The forgotten rubber band in the wrist. Hand Surg 2013;18:407-10. [Google Scholar]
- 6.Meier R, Haug L, Surke C, Mathys L, Vögelin E. Acquired constriction ring: A case of rubber band syndrome. Pediatr Emerg Care 2019;35:e113-5. [Google Scholar]
- 7.Huang YM, Yang SW, Chen CY, Hsu CJ, Chang WN. Residual foreign body in the foot causing chronic osteomyelitis mimicking a pseudotumor: A case report. J Int Med Res 2020;48:300060520925379. [Google Scholar]
- 8.Narayana Kurup JK, Shah HH. A rare case of rubber band syndrome of wrist with distal radius and ulna fracture. J Orthop 2020;20:60-2. [Google Scholar]
- 9.Regmi M, Desai S, Patwardhan S, Deshmukh W, Kapoor T, Patil N. Foreign body induced osteomyelitis in the hand-commonly missed clinical and radiological diagnosis. J Orthop Case Rep 2021;11:80-3. [Google Scholar]
- 10.Chandrashekara CM, George MA, Al-Marboi BS. Neglected foreign body, the cause of navicular osteomyelitis in a paediatric foot: A case report. J Orthop Case Rep 2013;3:26-9. [Google Scholar]
- 11.Jarraya M, Hayashi D, de Villiers RV, Roemer FW, Murakami AM, Cossi A, et al. Multimodality imaging of foreign bodies of the musculoskeletal system. AJR Am J Roentgenol 2014;203:W92-102. [Google Scholar]