Synovial hemangioma is a rare benign soft-tissue tumor occurring commonly in the knee joint. The symptoms are variable and the tumor is characteristic on a magnetic resonance imaging. Simultaneous two discrete in the same joint is a rare presentation of such tumor. Complete excision is the treatment of choice
Dr. Mantu Jain, Department of Orthopedics, AIIMS, Bhubaneswar, Odisha, India. E-mail: montu_jn@yahoo.com
Introduction: Synovial hemangioma (SH) is a rare benign soft-tissue tumor of vascular origin. That can be extraarticular, juxta-articular, or intraarticular. The knee joint is the most common joint involved. Symptoms can be variable and diagnosis can be made using magnetic resonance imaging. Differentials can be ruled out by biopsy and the gold standard treatment is complete excision of the lesion.
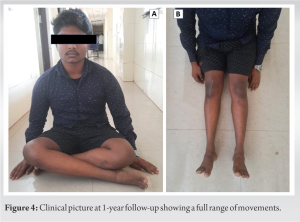
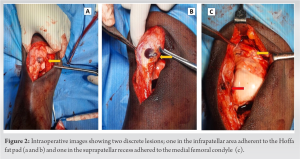
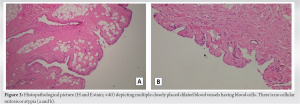
Case Report: A 20-year-old male presented to outpatient clinic with a chief complaint of right-sided anterior knee pain for 2 years aggravated for 2 months. Ultrasonography and magnetic resonance imaging showed two discrete intra-articular lesions. The lesion was hypointense on T1W and hyperintense on T2W and STIR sequence that was enhancing on contrast. There were adjoining dilated vessels. With a provisional diagnosis of hemangioma, FNAC was done and then complete excision was done using a medial parapatellar arthrotomy. The patient is doing well at 1-year follow-up.
Conclusion: Knee joint SH is a rare presentation to orthopedic outdoors and has slight female predominance with pre-existing history of trauma. In the present study, both cases were of patella-femoral type (anterior and infra-patellar fat pad). For such lesions, en bloc excision is the gold standard procedure to prevent recurrence, same procedure was followed in our study, and good functional outcome was achieved.
Keywords: Synovial hemangioma, knee joint, multiple, soft-tissue tumor.
Synovial hemangioma (SH) of the knee is a rare, benign tumor that can occur in the knee joint’s synovial lining, usually seen in young adults and children [1]. It is characterized by an abnormal growth of blood vessels within the synovial membrane, which can lead to pain, swelling, spontaneous hemarthrosis, and restricted joint movement. It is often misdiagnosed with other conditions such as lipoma arborescence, giant cell tumor of the tendon sheath, pigmented villonodular synovitis, synovial chondromatosis, and osteochondromatosis which mimics SH in clinical presentation [2, 3]. Diagnosing an SH of the knee typically involves a combination of imaging tests, such as magnetic resonance imaging (MRI) or ultrasound, and a biopsy to confirm the diagnosis [4]. Treatment options may include surgery to remove the tumor, radiation therapy, or joint replacement in severe cases due to hemorrhagic arthropathy [4, 5]. We report SH of the knee joint that occurred in an adolescent individual.
A 20-year-old male came to our outpatient department with progressively increasing pain in the right knee joint for the past 2 years; recently, in the past 2 months, he also noticed a swelling in the knee joint for which he has not received any prior medical treatment. The pain was constant, dull aching in character, non-radiating; and it has been changed and was aggravated on walking or climbing stairs. There was no history of trauma, fever, loss of appetite, or weight loss. On physical examination, we found a 2 cm × 2 cm swelling over the anterior aspect of the knee joint, which got prominent in full flexion. The knee joint line was non-tender, and there was no local rise in temperature. There were no signs of instability and the range of motion was full. There was no leg length discrepancy. On investigations, his complete blood parameters, including the coagulation profile and inflammatory markers, were found normal. The radiograph of the knee did not show any abnormality. An ultrasonogram of the knee joint revealed a thick-walled hypoechogenic lesion (14.4 mm × 5 mm) inferomedial to lower margin of patella having tortuous vascular channels and another small lesion in the suprapatellar recess. Further investigations with an MRI confirmed the presence of two lesions – one within the Hoffa’s fat pad and another one in the suprapatellar pouch area adhered to the lateral femoral condyle. Both lesions appeared hypointense on T1-weighted (T1w) and hyperintense on T2-weighted (T2w) and fat-suppressed (PDFS) images with contrast-enhancement (Fig. 1).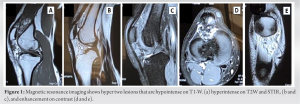
An hemangioma is a tumor‐like mass resulting from the proliferation of the blood vessels [6, 7]. SH accounts for 0.07% of all soft-tissue tumors, <1% of all hemangiomas, and 0.78% of all resected hemangiomas [6, 8]. The most common site is knee but it can occur in other joints as well [6, 8]. SH commonly occurs in children and young adults predominantly in males [8]. Symptoms are often non-specific but the most common presentation is chronic and persistent knee pain which is typically a mechanical type of pain progressing by remissions and exacerbations [8, 9]. Other symptoms are a limitation in the range of motion, joint swelling, or atraumatic intra-articular hemarthrosis [6, 7, 8]. SH does not affect the activities of daily living except at the times of exacerbations [8]. Our case presented with knee pain after prolonged sitting and on climbing stairs for the past 2 years. However, pain used to get relieved on standing and did not much affect his daily activities. A history of trauma has been considered as a significant factor after which SH was seen among several studies and Moon et al. showed that 35% of patients had a history of injury in the past [5, 10]. Our case also had a history of injury to his knee 6 months before presentation following which his symptoms exacerbated. An anatomical classification which can be considered in relation to the joint is intra-articular, juxta-articular, and intermediate type [1, 4]. Juxta-articular hemangiomas are found outside the joint capsule and presenting often as joint swelling as its main symptom. Intra-articular hemangiomas are found in the joint capsule. The intermediate type can show features of both [1, 4]. The juxta-articular and intermediate types are mostly reported [1]; however, our case was an intra-articular type. A review of the literature is provided in Table 1.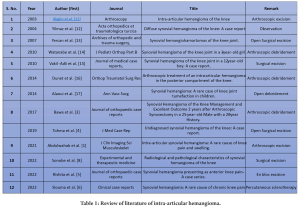
SH of the knee should be a differential diagnosis in case of non-specific and long-standing knee pain, even though it is a rare entity. If SH is, suspected MRI is the crucial investigation to be done, and the knee radiograph is of poor diagnostic value. Computer tomography angiography can be done to know the vascularity of the lesion and will help in embolization in case of a large lesion. Even though there are multiple treatment options for SH, the preferred method is surgical excision. Arthroscopic excision can be done if the lesion is intra-articular and pedunculated. The treatment should be initiated as early as possible to prevent cartilage damage as the disease advances.
SH is a rare presentation in orthopedic practice. The tumor is characteristic on MRI. Complete excision is the treatment of choice.
References
- 1.Abdulwahab AD, Tawfeeq DN, Sultan OM. Intra-articular synovial hemangioma: A rare cause of knee pain and swelling. J Clin Imaging Sci 2021;11:26. [Google Scholar]
- 2.Greenspan A, Azouz EM, Matthews J 2nd, Décarie JC. Synovial hemangioma: Imaging features in eight histologically proven cases, review of the literature, and differential diagnosis. Skeletal Radiol 1995;24:583-90. [Google Scholar]
- 3.Bawa AS, Garg R, Bhatnagar K, Singal S. Synovial hemangioma of the knee management and excellent outcome 2 years after arthroscopic synovectomy in a 25-year-old male with a 20-year history. J Orthop Case Rep 2017;7:17-20. [Google Scholar]
- 4.Tohma Y, Mii Y, Tanaka Y. Undiagnosed synovial hemangioma of the knee: A case report. J Med Case Rep 2019;13:231. [Google Scholar]
- 5.Rishita, Singh D, Singhvi A, Bharwani N, Jain H, Bhati M. Synovial hemangioma presenting as anterior knee pain-a case series. J Orthop Case Rep 2022;12:61-4. [Google Scholar]
- 6.Slouma M, Hannech E, Msolli A, Dhahri R, Kouki S, Metoui L, et al. Synovial hemangioma: A rare cause of chronic knee pain. Clin Case Rep 2022;10:10.1002/ccr3.6007. [Google Scholar]
- 7.Jain M, Sahoo J. Intramuscular cavernous haemangioma of the adductor brevis-a case report. J Med Sci 2016;2:123-7. [Google Scholar]
- 8.Sonobe T, Hakozaki M, Kaneuchi Y, Yamada H, Hasegawa O, Yamada S, et al. Radiological and pathological characteristics of synovial hemangioma of the knee. Exp Ther Med 2023;25:23. [Google Scholar]
- 9.Arslan H, İslamoğlu N, Akdemir Z, Adanaş C. Synovial hemangioma in the knee: MRI findings. J Clin Imaging Sci 2015;5:23. [Google Scholar]
- 10.Raj G, Deodhar MS, Chauhan A, Avasthi S, Rawat A, Verma C. Synovial hemangioma: A pictorial essay of two cases. Int J Res Med Sci 2017;5:2264. [Google Scholar]
- 11.Akgün I, Kesmezacar H, Oğüt T, Dervişoğlu S. Intra-articular hemangioma of the knee. Arthroscopy 2003;19:E17. [Google Scholar]
- 12.Yilmaz E, Karakurt L, Ozdemir H, Serin E, Incesu M. Dizde yaygin sinovyal hemanjiyom: Olgu sunumu [Diffuse synovial hemangioma of the knee: A case report]. Acta Orthop Traumatol Turc 2004;38:224-8. [Google Scholar]
- 13.Yercan HS, Okcu G, Erkan S. Synovial hemangiohamartomas of the knee joint. Arch Orthop Trauma Surg 2007;127:281-5. [Google Scholar]
- 14.Watanabe S, Takahashi T, Fujibuchi T, Komori H, Kamada K, Nose M, et al. Synovial hemangioma of the knee joint in a 3-year-old girl. J Pediatr Orthop B 2010;19:515-20. [Google Scholar]
- 15.Vakil-Adli A, Zandieh S, Hochreiter J, Huber M, Ritschl P. Synovial hemangioma of the knee joint in a 12-year-old boy: A case report. J Med Case Rep 2010;4:105. [Google Scholar]
- 16.Dunet B, Tournier C, Pallaro J, Boullet F, Fabre T. Arthroscopic treatment of an intra-articular hemangioma in the posterior compartment of the knee. Orthop Traumatol Surg Res 2014;100:337-9. [Google Scholar]
- 17.Alaoui NM, Lamalmi N, Saouab R, Gourinda H, Dendane MA. Synovial hemangioma: A rare case of knee joint tumefaction in children. Ann Vasc Surg 2014;28:260.e1-4. [Google Scholar]
- 18.Saxena P, Agarwal R, Nain G, Khurana N, Lal P, Tudu SK. Synovial hemangiomas of wrist and ankle joint: A report of two rare cases. Indian J Pathol Microbiol 2018;61:604-6. [Google Scholar]