Due to its significant recurrence potential, it is imperative to perform a meticulous excision of the tumor (GCTTS) to minimize the chances of its reappearance.
Dr. Naveen Sathiyaseelan, Department of Orthopaedics, Saveetha Medical College and Hospital, Chennai, Tamil Nadu, India. E-mail: spnaveen17@gmail.com
Introduction: Giant cell tumor of tendon sheath (GCTTS), also known as tenosynovial giant cell tumor or pigmented villonodular tenosynovitis, is a rare benign soft-tissue tumor with an unclear cause. It is the second most frequent soft-tissue tumor in the hand after ganglion cyst.
Case Report: We described a female patient, age 19, who has had a 3 cm × 2 cm firm swelling on the palmer aspect of the right second metacarpal region for 7 years. The bulge developed spontaneously and moved quite slowly. It is required to do a histological and radiographic evaluation to determine whether or not to pursue additional treatment. Excision surgery was done, and the tumor was entirely removed. According to histopathology, this mass was compatible with GCTTS without being malignant.
Conclusion: It is an uncommon instance of GCTTS at the hand, to sum up. The tumor should be entirely excised due to its high risk of recurrence to lower the likelihood of recurrence and restore hand function.
Keywords: Giant cell tumor of tendon sheath, tenosynovial giant cell tumor, pigmented villonodular tenosynovitis, soft-tissue tumor.
A single, hard, extra-articular benign soft-tissue tumor called giant cell tumor of tendon sheath (GCTTS) has been studied for many years. GCTTS, also known as tenosynovial giant cell tumor or pigmented villonodular tenosynovitis, is the second most common soft-tissue tumor in the hand after ganglion cysts [1,2,3,4]. It can happen at any age, but the third to fourth decades see the highest occurrence. With a female-to-male ratio of 3:1, it is more prevalent among females [5]. It is split into two types: Localized form and diffuse form, depending on the clinical and biological characteristics. Extra-articular and intra-articular are the other two categories. The hand and fingers are affected by the benign localized form, whereas the aggressive diffuse type only affects big joints [6]. Gaining local tumor control, regaining hand function, and maintaining good cosmetics are the objectives of treatment for giant cell tumors of the hand bones. Here, we provide a rare case report of GCTTS in a female that was found in the right second metacarpal region and reviewed the relevant academic literature. The patient and her family provided their informed consent, and the hospital ethics committee authorized this report.
A 19-year-old right-handed female patient with enlargement over the right thenar metacarpal region for 7 years presented to the orthopedic department of our hospital. Without any prior injury or thorn puncture, the swelling appeared on its own. It grew steadily and did not interfere too much with daily routines. The patient also complained of the right index finger discomfort brought on by a developing lump, as well as trouble holding a pen and writing. Quick DASH scoring was used to assess the hand function, pre-operative scoring was 85. Physical examination revealed a 3 × 2 cm enlargement at the volar aspect of the right thenar metacarpal (Fig. 1). There was no localized temperature increase or skin involvement. The swelling was well-defined, with a uniformly solid firmness and a smooth surface. A physical check revealed some little edema and soreness. The index finger flexed and extended normally. No family members had a history of illnesses relevant to the patient’s condition, and neither did they smoke or misuse alcohol. Hand’s X-ray (Fig. 2), localized soft-tissue shadow, was visible in AP and oblique images without any bone erosion. The hospital’s FNAC examination identified the enlargement as GCTTS. Surgical treatment was attempted by the patient’s needs and symptoms. After applying the tourniquet, we made a 4 cm curvilinear incision on the thenar crease. It was possible to see the mass at the second metacarpal’s volar aspect (Fig. 3).
There was no localized temperature increase or skin involvement. The swelling was well-defined, with a uniformly solid firmness and a smooth surface. A physical check revealed some little edema and soreness. The index finger flexed and extended normally. No family members had a history of illnesses relevant to the patient’s condition, and neither did they smoke or misuse alcohol. Hand’s X-ray (Fig. 2), localized soft-tissue shadow, was visible in AP and oblique images without any bone erosion. The hospital’s FNAC examination identified the enlargement as GCTTS. Surgical treatment was attempted by the patient’s needs and symptoms. After applying the tourniquet, we made a 4 cm curvilinear incision on the thenar crease. It was possible to see the mass at the second metacarpal’s volar aspect (Fig. 3).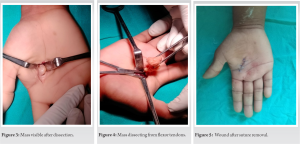 The flexor tendons were completely encircled by these masses (Fig. 4). The masses had eroded the bone and tendon sheath. The affected tendon sheath and the masses were removed. Two layers of closures were used, and the tourniquet was loosened. The tumor’s sliced segment revealed 3 × 2 cm of pale, reddish fibro-fatty tissue. After the surgery, the wound recovered without becoming infected. Standard post-operative care included active finger motion at the end of the 1st week, suture removal by the end of the 2nd week, and physiotherapist-supervised recovery up until a full range of active motion was achieved (Fig. 5). Histopathology (Fig. 6 and 7) of a GCTTS, typically contains the following information:
The flexor tendons were completely encircled by these masses (Fig. 4). The masses had eroded the bone and tendon sheath. The affected tendon sheath and the masses were removed. Two layers of closures were used, and the tourniquet was loosened. The tumor’s sliced segment revealed 3 × 2 cm of pale, reddish fibro-fatty tissue. After the surgery, the wound recovered without becoming infected. Standard post-operative care included active finger motion at the end of the 1st week, suture removal by the end of the 2nd week, and physiotherapist-supervised recovery up until a full range of active motion was achieved (Fig. 5). Histopathology (Fig. 6 and 7) of a GCTTS, typically contains the following information:
Gross description
The tumors appeared as well-circumscribed multi-lobulated lesions partially encapsulated by a pseudocapsule.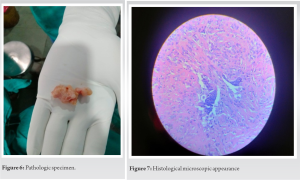
Microscopic examination
- Giant cells: The presence of osteoclastic multinucleated giant cells, which are scattered throughout the tumor. Focal areas reveal clusters of xanthoma cells associated with cholesterol cleft deposition.
- Stromal cells: The tumor also contains stromal cells, which are sheets of bland round oval to spindle mononuclear cells that surround the giant cells. The background fibrocollagenous stroma tissue shows hyalinization.
- Cellular atypia: Absence of cellular atypia.
- Mitotic activity: Mitotic figures are inconspicuous.
Final diagnosis
Based on the microscopic findings, these masses were consistent with GCTTS without malignancies. Every month, the patient underwent post-operative follow-up, and he or she made a full recovery with little to no edema or movement restriction. After the procedure, the proximal interphalangeal joint of the index finger and the flexion and extension of the metacarpophalangeal joint were both normal. The right and left sides both had strong grips and a smooth glide. There was no clinical or radiologic evidence of recurrence in the interim. Post-operative Quick DASH score was 35, showing significant improvement in hand function.
The teno-synosheath bursae and joint synovium are the origin of the benign fibrous tissue tumor known as GCTTS [2]. This tumor is more common in women than men and can develop at any age, with the third to fourth decade showing the highest incidence [7]. The cause of GCTTS is unknown; however, it may be associated with an inflammatory reaction process, a local abnormality of lipid metabolism, osteoclastic growth, trauma, infection, etc., [8]. In general, GCTTS manifests as a mass that grows slowly. Recurrence and joint injury are the main risks of GCTTS and necessitate surgical resection [9,10]. At present, radical surgical intervention is crucial to lowering recurrence. In our investigation, full excision of these lesions with tendon sheaths was performed to prevent recurrence. At the 6-month follow-up, which was carried out in the subsequent research, no recurrence was discovered. Here, we emphasize the need for aggressive removal of the tumor together with any tendon sheath and bone erosions. The patient’s hand flexion and extension movements were observed to be normal after surgery.
Our scenario is a unique instance of GCTTS at hand. In addition, because of its high probability of recurrence, the tumor should be thoroughly excised to minimize the likelihood of recurrence. The tumor must also undergo radiographic and histological testing; it is found to be benign and does not need any additional medical attention. To minimize the loss, the hand’s functionality should finally be restored.
We suggest to ensure complete excision of the tumor to minimize the chances of its reappearance and restore the functionality of the hand.
References
- 1.Ushijima M, Hashimoto H, Tsuneyoshi M, Enjoji M. Giant cell tumor of the tendon sheath (nodular tenosynovitis). A study of 207 cases to compare the large joint group with the common digit group. Cancer [Internet]. 1986;57(4):875–84. Available from: http://dx.doi.org/10.1002/1097-0142(19860215)57:4<875::aid-cncr2820570432>3.0.co;2-y [Google Scholar | PubMed | CrossRef]
- 2.Lanzinger WD, Bindra R. Gaint cell tumor of the tendon sheath. J Hand surg Am. 2013;38(1):154–7. [Google Scholar | PubMed]
- 3.Al-Qattan M. Giant cell tumors of tendon sheath: classification and recurrence rate. J Hand Surg. 2001;26B:72–75. [Google Scholar | PubMed]
- 4.Lucas DR. Tenosinovial giant cell tumor: case report and review. Arch Pathol Lab Med. 2012;136:901–6. [Google Scholar | PubMed]
- 5.Koutserimpas C, Kastanis G, Ioannidis A, Filippou D, Balalis K. Giant cell tumors of the tendon sheath of the hand: an 11-year retrospective study. J BUON. 2018;23:1546–51. [Google Scholar | PubMed]
- 6.Al Farii H, Zhou S, Turcotte R. The surgical outcome and recurrence rate of tenosynovial giant cell tumor in the elbow: a literature review. J Shoulder Elbow Surg. 2019;28(9):1835–40. [Google Scholar | PubMed]
- 7.Gouin F, Noailles T. Localized and diffuse forms of tenosynovial giant cell tumor (formerly giant cell tumor of the tendon sheath and pigmented villonodular synovitis). Orthop Traumatol Surg Res [Internet]. 2017;103(1):S91–7. Available from: http://dx.doi.org/10.1016/j.otsr.2016.11.002 [Google Scholar | PubMed | CrossRef]
- 8.Kerfant N, Bardin T, Roulot E. Multiple giant cell tumors of the tendon sheath:separate volar and dorsal lesions involving three digits of the same hand following repetitive trauma. J Hand Microsurg. 2015;7(1):233–5. [Google Scholar | PubMed]
- 9.Stiehl JB, Hackbarth DA. Recurrent pigmented villonodular synovitis of the hip joint. Case report and review of the literature. J Arthroplasty [Internet]. 1991;6 Suppl:S85-90. Available from: http://dx.doi.org/10.1016/s0883-5403(08)80061-7. [Google Scholar | PubMed | CrossRef]
- 10.Di Grazia S, Succi G, Fraggetta F, Perrotta RE. Giant cell tumor of tendon sheath: study of 64 cases and review of literature. G Chir. 2013;34:149–52. [Google Scholar | PubMed]