Young patients suffering from patellar maltracking and patellofemoral arthritis are expected to have significant improvement both in terms of the “target organ” as well as body image after undergoing patellofemoral joint arthroplasty.
Dr. Elias Mazzawi, Orthopedic Surgery Division, Rambam Health Care Campus, Haifa, Israel. E-mail: eliasmazzawi@gmail.com
Introduction: Patellofemoral joint arthroplasty (PFJA) is mainly used to treat older patients suffering from osteoarthritis. However, this case report sheds light on the implications of this treatment for young patients suffering from patellar maltracking and secondary patellofemoral osteoarthritis (PFOA).
Case Report: A female patient in her late 3rd decade of life presented with long-standing bilateral knee pain and significant functional impairment, including difficulty walking and stair climbing. She also expressed concern as a young female about her walking esthetics. Medical records indicated she underwent bilateral MPFL reconstruction in both knees simultaneously when she was 8 years old. Imaging studies revealed a bilateral complete patellar dislocation accompanied by bilateral patellofemoral joint osteoarthritis worse in the right knee. Various conservative treatment attempts were made with no or minimal relief. Consequently, bilateral PFJA was conducted, resulting in an overall transformational improvement in life quality at 39 months of follow-up on the right knee and 7 months of follow-up on the left knee.
Conclusion: PFJA is extremely beneficial for treating young patients suffering from patellar maltracking and patellofemoral arthritis. This is an original case report of interest to orthopedic surgery. Not only does PFJA treat osteoarthritis, but it also improves patellar tracking and may even decrease the progression of tibiofemoral osteoarthritis.
Keywords: Patella dislocation, patellofemoral joint replacement, knee laxity, patellofemoral pain, ligament laxity.
Recurrent instability of the patella is a debilitating disorder that mostly affects the young [1, 2]. While high-energy trauma is often required to induce patellar dislocation, it may also occur as a result of insignificant trauma in individuals with preexisting conditions such as trochlear or patellar dysplasia, increased Q angle, ligamentous laxity, or patella alta [3]. The stabilizers of the patella can be divided into bony and soft tissue structures. While the bony framework of the patellofemoral joint guides the patellar movement mainly in flexion angles, the soft tissue stabilizes the patella around extension [4], with the MPFL being the main passive stabilizer preventing the patella from lateral subluxation [5]. Persistent patellar instability unresponsive to conservative treatment may be treated surgically, as there are numerous procedures for stabilizing the patella, including tibial tubercle osteotomies, trochleoplasty, plication of tendons and ligaments, lateral retinacular release, and MPFL reconstruction [6]. However, failure or delay in treating the above-mentioned condition will inevitably cause early PFOA, which tends to worsen gradually and rarely responds to joint-preserving treatment, rendering patellofemoral joint arthroplasty (PFJA) the only lasting solution. In the following report, we present a young patient suffering from long-standing bilateral patellofemoral dislocation and secondary osteoarthritis who was successfully treated with PFJA.
A female patient in her late 3rd decade of life presented to our outpatient clinic with bilateral painful knees, walking and stair climbing difficulty, perceptible mechanical discomfort, and chronic increasing pain symptoms of both knees. She also expressed concern as a young female about her walking aesthetics. Medical records indicated she underwent bilateral MPFL reconstruction in both knees simultaneously when she was 8 years old. No documented follow-up was available for the interim two decades, except for personal and parental reports that surgery has not improved the situation from a very early stage. Clinical examination showed normal physical developmental status, bilateral midline old longitudinal surgical scars (Fig. 1 Clinical presentation of lower limbs axis and old surgical scars), BMI-30, symmetric valgus axis of lower limbs, bilateral knee extension lag of 10 degrees correctable passively to full symmetric extension. 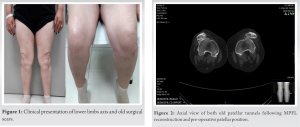 Fixed lateralized dislocated patella on the right knee. Patella dislocation on each extension motion of the left knee, producing a gross positive J sign. On CT examination, two tunnels drilled in the patella bilaterally were demonstrated in the sagittal view (Fig. 2 Axial view of both old patellar tunnels following MPFL reconstruction and pre-operative patellar position) following MPFL reconstruction. In addition, advanced-for age patellofemoral osteoarthritis (PFOA) with fixed dislocation on the right knee and dislocationof the patella on the left knee with milder osteoarthritic changes were visible. Moreover, bilateral Patella Alta and shallow trochlea were present bilaterally (Fig. 3 Pre-operative Computed Tomography, coronal and sagittal planes demonstrating joint lines and Patella Alta bilaterally).
Fixed lateralized dislocated patella on the right knee. Patella dislocation on each extension motion of the left knee, producing a gross positive J sign. On CT examination, two tunnels drilled in the patella bilaterally were demonstrated in the sagittal view (Fig. 2 Axial view of both old patellar tunnels following MPFL reconstruction and pre-operative patellar position) following MPFL reconstruction. In addition, advanced-for age patellofemoral osteoarthritis (PFOA) with fixed dislocation on the right knee and dislocationof the patella on the left knee with milder osteoarthritic changes were visible. Moreover, bilateral Patella Alta and shallow trochlea were present bilaterally (Fig. 3 Pre-operative Computed Tomography, coronal and sagittal planes demonstrating joint lines and Patella Alta bilaterally).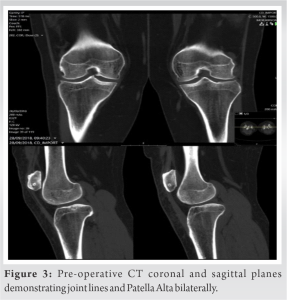 Various attempts at conservative treatments with physiotherapy, patella taping, and medication have yielded little relief, while progressive functional disability has compounded the general discomfort. Right knee PFJA with a trochlear implant and retaining the natural patella (Gender Solution, Zimmer Biomet) was performed with uneventful early follow-up. At 12 weeks, she presented with well centered patella tracking and an active range of motion from 0 to 120 degrees’ flexion. At 3 years’ post-op, the right knee maintained full range of motion, with no extension lag and no signs of patellar maltracking. A significant subjective improvement was reported regarding daily and recreational activity. However, the patient reported growing pain in the left knee and suffered from a progressive loss of extension ability. Thus, 3 years after PFJA of the right knee, a left PFJA with a similar implant and natural patella retention was performed. Early post-operative follow-up was uneventful (Fig. 4 and 5 Postoperative X-rays with implant position and centered patella bilaterally).
Various attempts at conservative treatments with physiotherapy, patella taping, and medication have yielded little relief, while progressive functional disability has compounded the general discomfort. Right knee PFJA with a trochlear implant and retaining the natural patella (Gender Solution, Zimmer Biomet) was performed with uneventful early follow-up. At 12 weeks, she presented with well centered patella tracking and an active range of motion from 0 to 120 degrees’ flexion. At 3 years’ post-op, the right knee maintained full range of motion, with no extension lag and no signs of patellar maltracking. A significant subjective improvement was reported regarding daily and recreational activity. However, the patient reported growing pain in the left knee and suffered from a progressive loss of extension ability. Thus, 3 years after PFJA of the right knee, a left PFJA with a similar implant and natural patella retention was performed. Early post-operative follow-up was uneventful (Fig. 4 and 5 Postoperative X-rays with implant position and centered patella bilaterally).  Presently, 40 months following right PFJA and 8 months following left PFJA, occasional discomfort is reported, with no effect on her ability for free social and recreational activity. A striking change regarding multiple elements concerning body image and self-perception is clearly visible. Furthermore, a substantial improvement in quality of life is apparent.
Presently, 40 months following right PFJA and 8 months following left PFJA, occasional discomfort is reported, with no effect on her ability for free social and recreational activity. A striking change regarding multiple elements concerning body image and self-perception is clearly visible. Furthermore, a substantial improvement in quality of life is apparent.
Patella maltracking in childhood is often the result of constitutional impairments, among which persistent fetal alignment, hypoplasia of the trochlea, and lower limb valgus alignment with ligamentous laxity are leading factors [7]. In the active growth physis period, surgical correction is based on soft tissue repair or reconstruction of the lax and stretched MPFL. The latter procedure has a failure rate that may reach as high as 10% in patients without any predisposing factors [8]. The combination of early-age patellar maltracking, presence of developmental risk factors, and failure of surgical correction inevitably results in early-age patellofemoral joint osteoarthritis, causing anterior knee pain, stiffness, and functional limitations [9]. Early-age patellofemoral arthroplasty is an appropriate solution for gross, late, post-operative failed patellar malalignment correction, complicated by patellofemoral arthritis. Sparing the relatively healthy tibiofemoral joint and resolving the arthritic changes as well as the dysplastic architecture of the joint are achievable goals of this type of surgery. While total knee arthroplasty (TKA) is widely considered the gold standard for treating primary PFOA unresponsive to conservative treatment, the use of PFJA in this setting is somewhat controversial [10, 11, 12], as first-generation PFJA showed higher revision rates and more complications compared to TKA, including patellar maltracking in the short term and progression of tibiofemoral arthritis in the long term. Mont showed that 97% of cases operated for TKA had a Knee Society score higher than 80 at a mean of 6.5 years with no revisions [13]. In addition, a meta-analysis including 374,934 arthroplasties concluded that the proportion of revisions was lower for TKA when compared to PFJA (0.49% and 1.75% respectively) [14]. Nevertheless, recreational activities and impairments in quality of life were not evaluated in these studies. As opposed to TKA, PFJA conserves native knee anatomy and kinematics since it maintains the tibiofemoral joint and the cruciate ligaments. Thus, PFJA probably provides a higher-functioning knee in young, active individuals. In fact, Ledbetter showed that PFJA patients engage in sports such as tennis and skiing [15]. First-generation PFJA implants (“in-lay” design) replaced the trochlear cartilage solely while sparing the subchondral bone. Thus, rotational alignment was dictated by the native trochlear orientation. Moreover, the technique was mostly free hand, and the mediolateral coverage was relatively narrow [16]. Outcomes were poor, with more than half of the implants failing in mid- and long-term follow-up [17]. The second-generation “on-lay” implants were designed to completely replace the anterior compartment of the knee, had a wider trochlear flange, and had better patellar tracking throughout the entire range of motion of the knee [18]. Therefore, these implants are more versatile, address different anatomic variations, and are suitable for most patients. Consequently, on-lay implants had better results, with Ackroyd et al. reporting a 96% survival rate of the second-generation Avon prosthesis at 5 years [19]. Currently, on-lay implants are widely indicated for PFJA. Modern PFJA is beneficial for patients with patellofemoral maltracking and dysplastic trochlea, as these disorders are corrected. Moreover, Dahm et al. showed that this group of patients, when operated on for patellofemoral arthroplasty, had a decreased progression of tibiofemoral arthritis [16], thus finding them ideal candidates for PFJA. In our case, we used the Zimmer Gender prosthesis, which has a flange that extends more proximally than the cartilage and therefore provides better engagement and excursion of the patella in extension. As a result, the patella tracks better and is less likely to subluxate through the entire range of motion [17].
Modern PFJ arthroplasty implants are inherently designed to resolve maltracking of the patella as well as treat PFJ osteoarthritis. In addition, young patients suffering from the above-mentioned conditions are expected to have significant improvement both in terms of the “target organ” as well as body image. Finally, consideration should be addressed to whether PFJ arthritis is primary or secondary.
Young patients suffering from patellar maltracking and patellofemoral arthritis are expected to have significant improvement both in terms of the “target organ” as well as body image after undergoing PFJA. Our article emphasizes the value of PFJA in treating this particular group of patients.
References
- 1.Fithian DC, Paxton EW, Stone ML, Silva P, Davis DK, Elias DA, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. [Google Scholar]
- 2.Hawkins RJ, Bell RH, Anisette G. Acute patellar dislocations. The natural history. Am J Sports Med 1986;14:117-20. [Google Scholar]
- 3.Carson WG Jr., James SL, Larson RL, Singer KM, Winternitz WW. Patellofemoral disorders: Physical and radiographic evaluation. Part II: Radiographic examination. Clin Orthop Relat Res 1984;185:178-86. [Google Scholar]
- 4.Heegaard J, Leyvraz PF, Van Kampen A, Rakotomanana L, Rubin PJ, Blankevoort L. Influence of soft structures on patellar three-dimensional tracking. Clin Orthop Relat Res 1994;299:235-43. [Google Scholar]
- 5.Conlan T, Garth WP Jr., Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am 1993;75:682-93. [Google Scholar]
- 6.Hautamaa PV, Fithian DC, Kaufman KR, Daniel DM, Pohlmeyer AM. Medial soft tissue restraints in lateral patellar instability and repair. Clin Orthop Relat Res 1998;349:174-82. [Google Scholar]
- 7.Wynne-Davies R. Familial joint laxity. Proc R Soc Med 1971;64:689-90. [Google Scholar]
- 8.Parikh SN, Nathan ST, Wall EJ, Eismann EA. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med 2013;41:1030-8. [Google Scholar]
- 9.Duncan R, Peat G, Thomas E, Wood L, Hay E, Croft P. Does isolated patellofemoral osteoarthritis matter? Osteoarthritis Cartilage 2009;17:1151-5. [Google Scholar]
- 10.Rodriguez-Merchan EC. Surgical treatment of isolated patellofemoral osteoarthritis. HSS J 2014;10:79-82. [Google Scholar]
- 11.Meding JB, Wing JT, Keating EM, Ritter MA. Total knee arthroplasty for isolated patellofemoral arthritis in younger patients. Clin Orthop Relat Res 2007;464:78-82. [Google Scholar]
- 12.Keltz E, Ofir D, Beer Y, Gruber N, Falah M, Nierenberg G. Surgical correction of non-traumatic patella maltracking. midterm clinical follow-up. Rambam Maimonides Med J 2022;13:e0010. [Google Scholar]
- 13.Mont MA, Haas S, Mullick T, Hungerford DS. Total knee arthroplasty for patellofemoral arthritis. J Bone Joint Surg Am 2002;84:1977-81. [Google Scholar]
- 14.Chawla H, van der List JP, Christ AB, Sobrero MR, Zuiderbaan HA, Pearle AD. Annual revision rates of partial versus total knee arthroplasty: A comparative meta-analysis. Knee 2017;24:179-90. [Google Scholar]
- 15.Leadbetter WB, Kolisek FR, Levitt RL, Brooker AF, Zietz P, Marker DR, et al. Patellofemoral arthroplasty: A multi-centre study with minimum 2-year follow-up. Int Orthop 2009;33:1597-601. [Google Scholar]
- 16.Dahm DL, Kalisvaart MM, Stuart MJ, Slettedahl SW. Patellofemoral arthroplasty: Outcomes and factors associated with early progression of tibiofemoral arthritis. Knee Surg Sports Traumatol Arthrosc 2014;22:2554-9. [Google Scholar]
- 17.Lonner JH, Bloomfield MR. The clinical outcome of patellofemoral arthroplasty. Orthop Clin North Am 2013;44:271-80, vii. [Google Scholar]
- 18.Walker T, Perkinson B, Mihalko WM. Patellofemoral arthroplasty: The other unicompartmental knee replacement. J Bone Joint Surg Am 2012;94:1712-20. [Google Scholar]
- 19.Ackroyd CE, Newman JH, Evans R, Eldridge JD, Joslin CC. The Avon patellofemoral arthroplasty: Five-year survivorship and functional results. J Bone Joint Surg Br 2007;89:310-5. [Google Scholar]