This case report demonstrates the successful conversion of a non-tolerated first metatarsal-phalangeal joint arthrodesis to arthroplasty utilizing decellularized dermal allograft, highlighting a potential salvage option.
Dr. John P Walsh, Department of Orthopaedic Surgery, Valley Hospital Medical Center, 620 Shadow Lane, Suite 450, Las Vegas, Nevada 89121, United States. E-mail: jwalsh@doclv.com
Introduction: Arthrodesis remains the gold standard for most first metatarsal-phalangeal joint (1MTPJ) pathologic conditions due to its high patient satisfaction, low complication rates, and consistent data. 1MTPJ arthroplasty remains a pursued procedure given the advantages described above, but the literature remains complicated and controversial as a primary surgical treatment. To the authors’ knowledge, there is no prior report describing utilization of arthroplasty as an approach to managing clinical failure of a successful fusion in the setting of a technically successful procedure without a post-operative complication.
Case Report: We present a case report of a 70-year-old female patient who underwent a successful 1MTPJ arthrodesis for hallux valgus and hallux rigidus and extensive tarsometatarsal arthrodesis for midfoot arthritis. Although the patient had radiographic evidence of successful fusion and had no surgical complications, she presented with dissatisfaction and pain due to functional limitations imposed by the procedure sequelae. The patient was diagnosed with right foot hallux interphalangeus with painful retained hardware. Conservative management failed to improve dissatisfaction or symptoms, and the patient opted for surgical takedown of her fusion with conversion to metatarsal-phalangeal joint arthroplasty, removal of hardware, and second toe proximal phalanx exostectomy. A stepwise surgical technique is described for the procedure, which was successful in addressing the patient’s perceived clinical failure.
Conclusion: Our case report describes a rare example of a patient who did not tolerate successful arthrodesis of the 1MTPJ, which was successfully revised to recreate the joint using a decellularized dermal allograft. The procedure resulted in fantastic patient satisfaction and long-term outcomes. This case report highlights a potential salvage option for patients who do not tolerate a 1MTPJ arthrodesis.
Keywords: Case report, first metatarsal-phalangeal joint fusion, revision arthroplasty, interpositional arthroplasty, hallux interphalangeus.
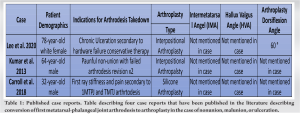
There is a rich body of literature that has consistently reported favorable surgical outcomes following arthrodesis procedures that have been durable and reliable over time with low complication rates [1, 2]. Consequently, arthrodesis became the gold standard for a myriad of first metatarsal-phalangeal joint (1MTPJ) pathology and with recommendations informed by high-level evidence [3, 4, 5]. Surgical decision-making requires careful navigation of diagnostic and therapeutic challenges while considering the degree of uncertainty imposed by evidence limitations [4, 6]. There is a dearth of literature investigating complications following a primary arthrodesis procedure [2, 7] and fewer describe an approach to management (Table 1) [2, 8, 9, 10, 11]. The most common complications are malunion/non-union and hardware-related complications [8, 12] and limited in scope to factors implicated in the technical failure of surgery. Technical factors that contribute to surgical failure are but one dimension of clinical failure and incompletely explain the difference between expectations and fulfillment of expectation [11, 13]. In the era of evidence-based medicine, there has been a paradigm shift in outcome assessment and redefined through patient perceptions with a clear difference in definition and expectation between patient and surgeon [9, 10]. To the authors’ knowledge, there is no prior report describing an approach to managing clinical failure in the setting of a technically successful procedure without a postoperative complication. From the patient’s perspective, the clinical failure was secondary to the sequela of a well-healed arthrodesis procedure without complicated post-operative course and complete resolution of symptoms. The purpose of this report is to provide a cautionary note on strict adherence to evidence-based practice and failure to incorporate patient perspectives in the surgical decision-making process. We describe our approach to planning a second surgery in the setting of a well-healed arthrodesis without hardware failure to address the perceived clinical failure of an asymptomatic patient. We provide a stepwise surgical technique that is previously unreported and emphasize the importance of considering unique patient perceptions that may influence the lens clinical outcomes which are interpreted through.
This is a case report of a 70-year-old retired female non-smoker with a history of breast cancer, anemia, hyperthyroidism, neuropathy, and s/p right 1MPTJ arthrodesis for hallux valgus and hallux rigidus and first tarsometatarsal (TMT) arthrodesis for midfoot arthritis 3 years ago. She presented with dissatisfaction and pain secondary to functional limitations imposed by her extensive fusion. She stated her foot felt rather stiff. The patient had an interval of symptom relief following the index procedure and radiographic evidence of successful fusion without experiencing a surgical complication. She reported that she had been compliant with index surgery postoperative protocols. She insidiously developed stiffness 2 years postoperatively that progressively worsened since onset. The patient believed that she experienced surgical failure and was dissatisfied with her altered gait and believed ipsilateral knee and hip pain were a consequence of her hallux stiffness. Clinical examination demonstrated well-healed surgical scars without signs of infection, a fused hallux metatarsal-phalangeal joint (MTPJ) in good position with pain overlying the dorsal aspect of the first toe and residual second toe deformity with skin irritation. Weight-bearing radiographs showed that hardware was maintained in proper alignment without signs of failure or loosening with radiographic evidence of successful fusion at the MTPJ and midfoot (Fig. 1a and b).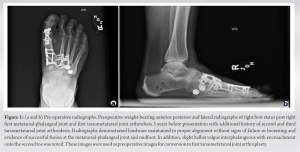
Technique
The patient was positioned supine and a thigh tourniquet was utilized. Surgery was done through a medial approach and hardware was removed without difficulty. Bone was resected from the metatarsal head and neck as well as the proximal phalanx. The tibial sesamoid was found to be partially fused and as a result partially resected to improve motion and relieve some of the patient’s plantar medial foot pain. A 4 mm wedge of symmetric bone was removed. The Guidewire for the metatarsal head reamer was inserted and metatarsal head subsequently reamed to recreate a metatarsal head like shape in the cancellous bone. Two guide wires were positioned into the metatarsal neck and overdrilled with a 2.5 mm drill (Fig. 2) to establish holes for suture passing. A luggage tag suture was placed through the ArthroFlex 3 mm patch after soaking the decellularized dermal allograft in irrisept and chlorhexidine solution. The graft was slid plantarly between the sesamoids and metatarsal heads. Suture passers were then used to pass sutures from plantar to dorsal. The dorsal flap of the graft was brought around and the plantar sutures brought up dorsally were secured in place with 3.0 mm bioabsorbable anchors (Fig. 3).



To the best of our knowledge, take down of a 1MTPJ arthrodesis and conversion to 1MTPJ arthroplasty has not been performed following a minimally symptomatic and well-healed 1MTPJ arthrodesis. There are several case reports highlighting conversion of 1MTPJ arthrodesis to arthroplasty in the case of nonunion, malunion, or ulceration (Table 1) [14-16]. Lee et al., describe a case of arthrodesis takedown and conversion to interpositional arthroplasty due to chronic pressure ulceration presumed from hardware prominence and comorbidities 4 years following initial arthrodesis [14]. After the arthrodesis takedown and interpositional arthroplasty, the patient presented with complications of an infectious wound dehiscence that was successfully treated with IV antibiotics [14]. 16 months following the salvage procedure, she presented without any evidence of ulceration, infection, non-union, or the recurrence of her hallux abductovalgus deformity [14]. Kumar and Clough highlights a case of a 64-year-old male who had previously failed 1MTPJ arthrodesis, including two attempts at interpositional bone grafting, and was left with pseudoarthrosis and was eventually treated with silastic arthroplasty as a salvage technique [15]. 6-months following the procedure, the patient reported good satisfaction, resolution of the “cock-up” deformity, hallux lengthening, and improvement in range of motion [15]. Carroll and Sharpe describes a case of 1MTPJ arthrodesis malunion treated with a 2-stage procedure, silicone implant arthroplasty in a 32-year-old male [16]. 15-months following his procedure, he reported improvement of his pain, better gait pattern, satisfaction of his procedure, and returning to light military duties [16]. While all the cases discussed above had successful short-term outcomes, none of the cases highlight outcomes >16 months following arthroplasty as a revision or salvage procedure. Regarding our case report, it is important to consider why the patient did not tolerate a successful arthrodesis. Our patient had a 1MTPJ arthrodesis, in addition to, a more proximal first TMT joint arthrodesis through a modified Lapidus procedure. We suspect that the combination of 1MTPJ and TMT joint fusion may have led to significant medial column stiffness and rigidity, eventually altering her gait causing hip and knee pain. A biomechanical gait study following 1MTPJ arthrodesis showed forefoot and hindfoot compensation to maintain a normal gait [12]. Therefore, additional fusion of the proximal midfoot could potentially alter her gait enough to cause intolerance of the arthrodesis. However, it has been demonstrated that biomechanical motion at the medial column of the foot is largely at the intermediate cuneiform and second metatarsal, as well as, the medial cuneiform and intermediate cuneiform, rather than the first TMT joint [8]. The modified Lapidus procedure does not compromise the former joints, which, therefore, should not hinder medial column motion. Nonetheless, medial column stiffness cannot be ruled out in our case. One study which included 18 feet which underwent 1MTPJ arthrodesis in combination to a proximal correction for severe hallux valgus was evaluated and found good patient satisfaction at 1 year, as well as satisfactory anatomic correction radiographically [9]. However, the study is somewhat limited given the small patient population used and the limited follow-up of a year, considering the patient in our case presented with gait changes, hip and knee pain, and metatarsalgia many years following her procedures. Much of the data specific to 1MTPJ arthroplasty is controversial and contradictory but surgeons continue to investigate this procedure given the potential advantages which include non-restricted footwear to be worn, normal gait pattern, assist in balance, impact reduction, and a normal stance. The controversial data are likely due to limited studies and a large variety of arthroplasty techniques which include excisional arthroplasty, interpositional arthroplasty, and implant arthroplasty which may present with different outcomes [10, 11, 17]. Often, hallux MTPJ arthrodesis versus arthroplasty is a decision for primary surgical treatment. Primary hallux arthroplasty often can be converted to an arthrodesis in the event of failure and is well-described in the literature [11, 13]. Our case described above is unique, in that an arthrodesis takedown was performed to recreate the joint and motion with the hope of decreasing some of the patient’s complaints in her forefoot. Fortunately, the arthrodesis take-down and joint recreation with a decellularized dermal allograft bio-implant was successful and our patient has enjoyed satisfaction, a complication free post-operative 3-year period, and resolution of her ipsilateral hip and knee pain. She reports returning to many of her daily activities that she was unable to do with her arthrodesis due to mobility issues, gait changes, and the development of hip and knee pain.
Arthrodesis remains the gold standard for most 1MTPJ pathologic conditions due to its high patient satisfaction, low complication rate, and durable outcomes. 1MTPJ arthroplasty remains an option with controversial data as a primary surgical treatment. Our case report describes a rare example of a patient who did not tolerate successful arthrodesis of the hallux MTPJ, which was successfully revised to recreate the joint using a decellularized dermal allograft. The procedure resulted in a satisfied patient with mid-term clinical and radiographic outcomes. This case report highlights a potential salvage option for patients who do not tolerate hallux MTPJ arthrodesis. When considering surgical treatment options of 1MTPJ pathological conditions, the question proposed by Hanft et al., remains, “Are we trying to satisfy patients or reconstruct an anatomic first metatarsophalangeal joint?” [18].
This case report will change clinical practice as it highlights a potential salvage option for patients who do not tolerate hallux MTPJ arthrodesis.
References
- 1.Rammelt S, Panzner I, Mittlmeier T. Metatarsophalangeal joint fusion: Why and how? Foot Ankle Clin 2015;20:465-77. [Google Scholar]
- 2.Roukis TS. First metatarsal-phalangeal joint arthrodesis: Primary, revision, and salvage of complications. Clin Podiatr Med Surg 2017;34:301-14. [Google Scholar]
- 3.Petrisor BA, Keating J, Schemitsch E. Grading the evidence: Levels of evidence and grades of recommendation. Injury 2006;37:321-7. [Google Scholar]
- 4.Guyatt GH, Oxman AD, Kunz R, Vist GE, Falck-Ytter Y, Schünemann HJ, et al. What is “quality of evidence” and why is it important to clinicians? BMJ 2008;336:995-8. [Google Scholar]
- 5.Griffin XL, Haddad FS. Evidence-based decision making at the core of orthopaedic practice. Bone Joint J 2014;96-B:1000-1. [Google Scholar]
- 6.Makridakis S, Kirkham R, Wakefield A, Papadaki M, Kirkham J, Long L. Forecasting, uncertainty and risk; perspectives on clinical decision-making in preventive and curative medicine. Int J Forecast 2019;35:659-66. [Google Scholar]
- 7.Kelikian AS. Technical considerations in hallux metatarsalphalangeal arthrodesis. Foot Ankle Clin 2005;10:167-90. [Google Scholar]
- 8.Clews CN, Kingsford AC, Samaras DJ. Autogenous capsular interpositional arthroplasty surgery for painful hallux rigidus: Assessing changes in range of motion and postoperative foot health. J Foot Ankle Surg 2015;54:29-36. [Google Scholar]
- 9.Parker J, Nester CJ, Long AF, Barrie J. The problem with measuring patient perceptions of outcome with existing outcome measures in foot and ankle surgery. Foot Ankle Int 2003;24:56-60. [Google Scholar]
- 10.MacMahon A, Cody EA, Caolo K, Henry JK, Drakos MC, Demetracopoulos CA, et al. Comparison of patients’ and surgeons’ expectations in foot and ankle surgery. Foot Ankle Int 2020;41:1173-80. [Google Scholar]
- 11.Anderson MR, Baumhauer JF, DiGiovanni BF, Flemister S, Ketz JP, Oh I, et al. Determining success or failure after foot and ankle surgery using patient acceptable symptom state (PASS) and patient reported outcome information system (PROMIS). Foot Ankle Int 2018;39:894-902. [Google Scholar]
- 12.Baumhauer JF, Singh D, Glazebrook M, Blundell C, De Vries G, Le ILD, et al. Prospective, randomized, multi-centered clinical trial assessing safety and efficacy of a synthetic cartilage implant versus first metatarsophalangeal arthrodesis in advanced hallux rigidus. Foot Ankle Int 2016;37:457-69. [Google Scholar]
- 13.Chrea B, Day J, Henry J, Cody E, HSS Orthopaedic Foot and Ankle Surgery Group, Ellis S. Influence of complications and revision surgery on fulfillment of expectations in foot and ankle surgery. Foot Ankle Int 2021;42:859-66. [Google Scholar]
- 14.Lee J, So E, Logan DB. Conversion of first metatarsophalangeal joint arthrodesis to interpositional arthroplasty with acellular dermal matrix for first ray ulceration: A case report. J Foot Ankle Surg 2020;59:634-7. [Google Scholar]
- 15.Kumar V, Clough T. Silastic arthroplasty of the first metatarsophalangeal joint as salvage for failed revisional fusion with interpositional structural bone graft. BMJ Case Rep 2013;2013:bcr2013008993. [Google Scholar]
- 16.Carroll PJ, Sharpe JJ. First metatarsophalangeal arthrodesis malunion revision to silicone implant arthroplasty. Int J Foot Ankle 2018;2:14. [Google Scholar]
- 17.Watson TS, Panicco J, Parekh A. Allograft tendon interposition arthroplasty of the hallux metatarsophalangeal joint: A technique guide and literature review. Foot Ankle Int 2019;40:113-9. [Google Scholar]
- 18.Hanft JR, Merrill T, Marcinko DE, Mendicino R, Gerbert J, Vanore JV. Grand rounds: First metatarsophalangeal joint replacement. J Foot Ankle Surg 1996;35:78-85. [Google Scholar]