Autografts can be used successfully for lateral femoral condyle bone defects in young patients undergoing CAS TKA.
Dr. Anoop Jhurani, Director, Department of Joint Replacement Services, Fortis Escorts Hospital, JLN Marg, Malviya Nagar - 302 015, Jaipur, India. E-mail: anoopjhurani@gmail.com
Introduction: Neglected distal femur fractures often present with significant uncontained bone defects of the lateral femoral condyle (LFC) leading to a valgus deformity and lateral compartment arthritis.
Case Report: Bone defect can be managed with the help of autogenous bone graft harvested from a distal femur cut and shaped in the form of an augment. The objective of using bone graft along with the primary femur was to restore bone stock in a young patient and prevent the use of an augment with a revision femur and intramedullary rod.
Conclusion: The use of computer navigation helped in getting accurate components and overall alignment thus facilitating compression at the bone graft site and early union.
Keywords: Lateral femoral condyle fracture, bone graft, computer navigation.
Fractures of the lateral femoral condyle (LFC) account for nearly one-third of all intra-articular fractures of the distal femurThe most common complication associated with these fractures is malunion or nonunion leading to lateral compartment arthritis, valgus deformity, and progressive ambulatory dysfunction [3, 4]. Most of these patients are young and may require a total knee arthroplasty (TKA) to restore alignment, balance, and function. The main challenge is the resulting bone defect of the LFC which needs to be addressed appropriately to ensure longevity of the prosthesis. There are four potential methods to handle the defect of the LFC. First is to build up the defect with screws and cement. This method can be employed if the bone defect is less than 5 mm. In both the cases we present, the bone defect measured more than 5 mm precluding the use of screws and cement. The second technique is to use allograft to build up the defect of the LFC. Allografts have the potential to transmit infection and may exhibit resorption over time [5]. These issues in conjunction with the unavailability of allografts at our institution prevented the use of this method. The third technique is to restore the bone defect with a modular augment. The use of an augment necessitates use of a revision femoral component and with an intramedullary stem, thus increasing the cost and complexity of the procedure [6]. In addition, the use of a revision femoral component with intramedullary stems in a young patient can complicate future revision procedures. We have used a novel autogenous bone grafting method in which the distal medial femoral condylar resection was used to restore the LFC defect. The sclerotic medial femoral bone served as a good substitute for the LFC defect and solid fixation was obtained with the placement of two overdrilled countersunk screws. This along with accurate alignment and balance achieved with computer navigation helped in a prompt union of the bone graft using the primary femoral implant. In this study, we describe two cases of LFC fracture nonunion treated by medial femoral bone graft and screw fixation with the primary femoral component. Both cases were performed with the assistance of computer navigation and did not require the use of augments or intramedullary stems.
Case 1
A 42-year-old male presented with nonunion of the distal LFC (Fig. 1).  The fracture was managed conservatively elsewhere and the patient presented with progressive valgus deformity and inability to bear weight. On examination, the pre-operative range of motion was 25–100°. His knee society score (KSS) was 49 and Western Ontario and Macmaster Universities Osteoarthritis Index (WOMAC) was 31. TKA was performed with image-free Ci navigation system (Brain Lab, Munich, Germany) using a cemented, posterior cruciate substituting design (Legion®, Smith and Nephew, USA). Pins were inserted inside the incision, through a standard medial parapatellar approach (Fig. 2).
The fracture was managed conservatively elsewhere and the patient presented with progressive valgus deformity and inability to bear weight. On examination, the pre-operative range of motion was 25–100°. His knee society score (KSS) was 49 and Western Ontario and Macmaster Universities Osteoarthritis Index (WOMAC) was 31. TKA was performed with image-free Ci navigation system (Brain Lab, Munich, Germany) using a cemented, posterior cruciate substituting design (Legion®, Smith and Nephew, USA). Pins were inserted inside the incision, through a standard medial parapatellar approach (Fig. 2).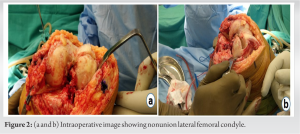 The pre-operative kinematics navigation graph demonstrated a fixed flexion deformity of 21° with 4.5° of valgus deformity (Fig. 3).
The pre-operative kinematics navigation graph demonstrated a fixed flexion deformity of 21° with 4.5° of valgus deformity (Fig. 3). Valgus deformity was gradually corrected with progressive knee flexion. An additional 2 mm of distal femur cut was planned to correct severe fixed flexion deformity. Then femur was prepared with size 7 and rotation was checked with the help of navigation. 8 mm of tibia was cut with 3° of posterior slope. Lateral tibial osteophytes were removed and mediolateral gaps were analyzed. The residual deformity was corrected with the release of the iliotibial band in extension. The primary femur was trialed on the prepared bone cuts and the bone defect of the LFC was measured with a scale. It was 7 mm in case 1 and 10 mm in case 2. The distal femur cut from the medial femoral condyle was shaped in the form of an augment and used to bone graft the defect of the LFC. Cartilage was removed from the graft and shaped according to the defect with the help of saw (triangular in case 1 and rectangular in case 2). Drill holes were made in the bed of the LFC and the bone graft was fixed with 2 cortical screws (Fig. 4).
Valgus deformity was gradually corrected with progressive knee flexion. An additional 2 mm of distal femur cut was planned to correct severe fixed flexion deformity. Then femur was prepared with size 7 and rotation was checked with the help of navigation. 8 mm of tibia was cut with 3° of posterior slope. Lateral tibial osteophytes were removed and mediolateral gaps were analyzed. The residual deformity was corrected with the release of the iliotibial band in extension. The primary femur was trialed on the prepared bone cuts and the bone defect of the LFC was measured with a scale. It was 7 mm in case 1 and 10 mm in case 2. The distal femur cut from the medial femoral condyle was shaped in the form of an augment and used to bone graft the defect of the LFC. Cartilage was removed from the graft and shaped according to the defect with the help of saw (triangular in case 1 and rectangular in case 2). Drill holes were made in the bed of the LFC and the bone graft was fixed with 2 cortical screws (Fig. 4).  The distal part of the screw heads was over-drilled and countersunk to achieve compression at the bone grafting site. The bone graft was well fixed and had no motion after screw fixation. The primary femur trial did not have any movement and was very stable after the bone graft. It was ensured that cement did not percolate between the bone graft and host bone at the time of cementing the final implant. There was a complete correction of the biplanar deformity as demonstrated by post-operative kinematics graph. Post-operative anteroposterior and lateral radiographs showed well-placed femoral and tibial prosthesis components with correct limb alignment and bone graft fixed with two cortical screws. The KSS improved from 49 to 98 and the WOMAC score improved from 31 to 90. At 2 years follow up X-ray showed a union of the bone graft with no evidence of loosening of the femoral prosthesis (Fig. 5). The patient had ROM of 0º–110º. His post-operative KSS improved to 98 and WOMAC score to 90 at 2 years’ follow-up.
The distal part of the screw heads was over-drilled and countersunk to achieve compression at the bone grafting site. The bone graft was well fixed and had no motion after screw fixation. The primary femur trial did not have any movement and was very stable after the bone graft. It was ensured that cement did not percolate between the bone graft and host bone at the time of cementing the final implant. There was a complete correction of the biplanar deformity as demonstrated by post-operative kinematics graph. Post-operative anteroposterior and lateral radiographs showed well-placed femoral and tibial prosthesis components with correct limb alignment and bone graft fixed with two cortical screws. The KSS improved from 49 to 98 and the WOMAC score improved from 31 to 90. At 2 years follow up X-ray showed a union of the bone graft with no evidence of loosening of the femoral prosthesis (Fig. 5). The patient had ROM of 0º–110º. His post-operative KSS improved to 98 and WOMAC score to 90 at 2 years’ follow-up.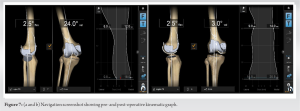
Case 2
A 43-years-old male presented with a history of right lateral femoral condylar fracture operated elsewhere in March 1999. He had progressive valgus deformity with the inability to ambulate. The right knee had ROM from 2° to 90°. The pre-operative anteroposterior and lateral radiograph show nonunion of the LFC along with valgus deformity (Fig. 6). Navigation showed pre-operative deformity of 24° valgus with 2.5° of fixed flexion deformity. Kinematic graph (right side of screen) showed tight lateral gap in extension and flexion (Fig. 7). Cemented, posterior cruciate substituting design (Legion®, Smith and Nephew, USA) was planned. The femur was prepared first with a 9.5 mm distal femur resection. The extension gap was assessed and femur was prepared with size 6 anterior-posterior chamfer cutting jig. Tibia was prepared using an extramedullary jig under navigation control. After tibial preparation lateral osteophytes were removed. Flexion and extension gaps were again reassessed and residual deformity was analyzed. There was 3° of residual valgus deformity, which was corrected with release of iliotibial band in extension and popliteus tendon in flexion. The advantage of using computer navigation in this case was obliteration of intramedullary cavity by the screw inserted 20 years back. It was not possible to remove the screw as it was deeply embedded in the bone. A lateral condyle bone defect was visualized, for which bone graft was harvested from distal cut of medial femoral condyle and was shaped in the form of an augment. The bone graft was fixed with the help of two cortical screws (Fig. 8). After fixation of the bone graft, the primary femur had good stability and hence there was no need to add metal augment with revision femur and a rod. The purpose in this case was to restore bone in a young patient and avoid the need for revision femur and intramedullary rod. Patellar resurfacing was done and appropriate patellar tracking was achieved. The post-operative radiographs show well-placed femoral and tibial prosthesis components with correct limb alignment. At 2 years’ follow–up, the x-ray showed a union of the bone graft with no radiolucent lines in any of the zones around femur and tibia (Fig. 9). We observed increase in KSS from 49 to 100 and WOMAC scores from 30 to 92. The final range of motion achieved was 0°–120° flexion. Post-operative rehabilitation and follow-up: Static quadriceps strengthening exercises with gentle ROM were started for both patients from the immediate post-operative day. Patients were made to walk full weight bearing from the next post-operative day. Both the patients were followed up with radiographs at 2 months, 6 months, and 1-year interval.
Cemented, posterior cruciate substituting design (Legion®, Smith and Nephew, USA) was planned. The femur was prepared first with a 9.5 mm distal femur resection. The extension gap was assessed and femur was prepared with size 6 anterior-posterior chamfer cutting jig. Tibia was prepared using an extramedullary jig under navigation control. After tibial preparation lateral osteophytes were removed. Flexion and extension gaps were again reassessed and residual deformity was analyzed. There was 3° of residual valgus deformity, which was corrected with release of iliotibial band in extension and popliteus tendon in flexion. The advantage of using computer navigation in this case was obliteration of intramedullary cavity by the screw inserted 20 years back. It was not possible to remove the screw as it was deeply embedded in the bone. A lateral condyle bone defect was visualized, for which bone graft was harvested from distal cut of medial femoral condyle and was shaped in the form of an augment. The bone graft was fixed with the help of two cortical screws (Fig. 8). After fixation of the bone graft, the primary femur had good stability and hence there was no need to add metal augment with revision femur and a rod. The purpose in this case was to restore bone in a young patient and avoid the need for revision femur and intramedullary rod. Patellar resurfacing was done and appropriate patellar tracking was achieved. The post-operative radiographs show well-placed femoral and tibial prosthesis components with correct limb alignment. At 2 years’ follow–up, the x-ray showed a union of the bone graft with no radiolucent lines in any of the zones around femur and tibia (Fig. 9). We observed increase in KSS from 49 to 100 and WOMAC scores from 30 to 92. The final range of motion achieved was 0°–120° flexion. Post-operative rehabilitation and follow-up: Static quadriceps strengthening exercises with gentle ROM were started for both patients from the immediate post-operative day. Patients were made to walk full weight bearing from the next post-operative day. Both the patients were followed up with radiographs at 2 months, 6 months, and 1-year interval.
The main aim of this case report is to share the technique of using autogenous bone graft for uncontained defect of the LFC in computer-assisted TKA. Neglected lateral condyle femur fractures as shown in the two cases present with significant bone defect of the LFC leading to valgus deformity and lateral compartment arthritis. One method to reduce the bone defect as often practiced in tibia is to resect 2–3 mm more bone and use a thicker poly but this method cannot be used in the femur as it would increase the extension gap selectively. While the bone grafting technique is well described in literature for uncontained defects on the tibial side, there are no studies suggesting bone grafting on the femoral side in primary TKA [7]. We have used bone grafting on the femoral side as it is cost-effective method when compared to using an augment, revision femur, and an intramedullary rod. The cost of using bone grafting with a primary femur is almost half when compared to the revision set. The bone grafting technique restores bone stock in young patients and will facilitate revision whenever required. A common way to handle such a situation is to build the bone defect with a metal augment. However, whenever a metal augment is used a revision femur along with an intramedullary stem has to be used to prevent component failure [8, 9]. We have taken a contrarian approach and used autograft shaped in the form a distal augment and fixed with two cortical screws. We have used a primary femur thus eliminating the use of an intramedullary stem. The graft was completely incorporated at 2-year follow-up and there were no signs of loosening of the femoral component. This along with the use of computer navigation in both cases ensured complete correction of deformity in both coronal and sagittal planes, thus leading to accurate alignment and ligament balance [10]. This could also be a factor in early incorporation of the bone graft as the weight-bearing axis passing through the center of the knee joint would lead to compression forces prompting the union of the bone graft. Current controversies and future considerations: Our technique of using autograft for uncontained defect of the LFC in neglected lateral condyle femur fractures is unique and leads to restoration of bone stock along with use of primary femur in young patients. We continue to follow-up on these patients with the objective of detecting any loosening of the femoral component in the mid-term.
Neglected LFC fracture results in lateral compartment arthritis, valgus deformity, and instability. The main challenge is the bone defect which can be dealt with the use of a metal augment, which however necessitates the use of a revision femur with an intramedullary stem to prevent component failure. On the contrary, we used autograft shaped in the form of a distal augment and fixed with cortical screws thus leading to the restoration of bone stock along with the use of the primary femur. Computer navigation helped in accurate restoration of alignment thus aiding in compression forces perpendicular to the mechanical axis facilitating union of the bone graft.
Defects resulting from femoral condyle non-union can be managed by autogenous graft and use of a primary femur thus restoring bone stock in young patients.
References
- 1.Mortazavi SJ, Khan F, Ramezanpour A, Firoozabadi M. Post-traumatic total knee arthroplasty: A case of Hoffa fracture nonunion and review of literature. J Orthop Spine Trauma 2020;4:59-61. [Google Scholar]
- 2.Weiss NG, Parvizi J, Hanssen AD, Trousdale RT, Lewallen DG. Total knee arthroplasty in post-traumatic arthrosis of the knee. J Arthroplasty 2003;18(3 Suppl 1):23-6. [Google Scholar]
- 3.Saleh H, Yu S, Vigdorchik J, Schwarzkopf R. Total knee arthroplasty for treatment of post-traumatic arthritis: Systematic review. World J Orthop 2016;7:584-91. [Google Scholar]
- 4.Singh AP, Dhammi IK, Vaishya R, Jain AK, Singh AP, Modi P. Nonunion of coronal shear fracture of femoral condyle. Chin J Traumatol 2011;14:143-6. [Google Scholar]
- 5.Bostrom MP, Seigerman DA. The clinical use of allografts, demineralized bone matrices, synthetic bone graft substitutes and osteoinductive growth factors: A survey study. HSS J 2005;1:9-18. [Google Scholar]
- 6.Mabry TM, Hanssen AD. The role of stems and augments for bone loss in revision knee arthroplasty. J Arthroplasty 2007;22(4 Suppl 1):56-60. [Google Scholar]
- 7.Kharbanda Y, Sharma M. Autograft reconstructions for bone defects in primary total knee replacement in severe varus knees. Indian J Orthop 2014;48:313-8. [Google Scholar]
- 8.Reddy VG, Mootha AK, Chiranjeevi T, Kantesaria P. Total knee arthroplasty as salvage for non-union in bicondylar Hoffa fracture: A report of two cases. J Orthop Case Rep 2011;1:26-8. [Google Scholar]
- 9.Haidukewich GJ, Springer BD, Jacofsky DJ, Berry DJ. Total knee arthroplasty for failed internal fixation or nonunion of the distal femur. J Arthroplasty 2005;20:344-49. [Google Scholar]
- 10.Jones CW, Jerabek SA. Current role of computer navigation in total knee arthroplasty. J Arthroplasty 2018;33:1989-93. [Google Scholar]









