Radiographs of the forearm are inadequate to assess for elbow dislocations even if the elbow region is covered in the radiograph.
Dr. Madhan Jeyaraman, Department of Orthopaedics, ACS Medical College and Hospital, Dr MGR Educational and Research Institute, Chennai, Tamil Nadu, India. E-mail: madhanjeyaraman@gmail.com
Introduction: Neglected elbow dislocation is defined as a dislocation that is present for 3 weeks or longer. There is no available literature on neglected elbow dislocations, leading to ankylosis of the elbow joint.
Case Report: A 17-year-old female sustained a road traffic accident. Anteroposterior and lateral view radiographs of the forearm were done and deemed to be normal at another hospital. Six months after the injury, she presented to us with complaints of absent elbow movements. Examination revealed the elbow to be fixed in 30° of flexion. Radiographs of the elbow revealed an ankylosis of the ulnohumeral articulation in an abnormal position.
Conclusion: This case demonstrates that neglected elbow dislocations can lead to ankylosis of the joint. It also shows how radiographs of the forearm are inadequate to assess for elbow dislocations even if the elbow region is covered in the radiograph.
Keywords: Elbow, dislocation, ankylosis, ulnohumeral.
An elbow dislocation signifies the complete dislodgment of the ulna from its normal articulation with the humerus, usually occurring due to traumatic injury. To diagnose an acute elbow dislocation comprehensively, a meticulous assessment is imperative. This involves obtaining a detailed patient history to understand the mechanism of injury, conducting a thorough physical examination to assess joint stability and neurovascular status, and employing imaging modalities. Radiographs aid in confirming the dislocation, evaluating joint congruity, and identifying potential associated fractures [1]. Magnetic resonance imaging can be used to identify soft-tissue injuries [2]. The early identification and prompt management of an elbow dislocation hold paramount importance. Timely recognition is critical to prevent a range of complications, including neurovascular injury, recurrent instability, or the development of chronic pain and stiffness [3]. An immediate reduction of the dislocation, often achieved through closed reduction under anesthesia, serves as a pivotal intervention. This maneuver not only restores joint alignment but also mitigates the risk of long-term articular damage, ultimately optimizing the patient’s functional recovery and prognosis [4]. We present a case of a missed elbow dislocation despite examination by an orthopedician and radiographs being performed.
A 17-year-old female had a history of fall from a two-wheeler and sustained injury to her right elbow. She consulted at another hospital, where anteroposterior and lateral view radiographs of the forearm were done (Fig. 1). She was told there was no significant injury and was given analgesics. She continued to have pain in her elbow and was unable to bend her elbow freely. She then consulted another orthopedician 2 weeks later, who reviewed the same radiographs, and reassured the patient that were so no bony problem and that there could be a ligament injury around the elbow. He advised her to use an arm pouch for 2 months to aid in ligament healing.6 months after the injury, she presented to us with complaints of absent elbow movements. Examination revealed the elbow to be fixed in 30° of flexion, with no active or passive movements possible. 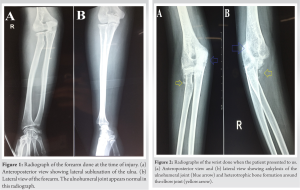
This case demonstrates the importance of separate anteroposterior and lateral radiographs of the elbow to detect subluxations/dislocations. The radiographs done for the patient at the time of injury were anteroposterior and lateral radiographs of the forearm. Despite covering the elbow joint and distal end of the humerus, they gave a false impression of the absence of any dislocation. While the anteroposterior view did show a subluxation of the elbow, the lateral view made the elbow joint appears normal. These subtle features were missed, leading to the missed diagnosis. Despite the patient being examined by two orthopedicians, the elbow in all likelihood continued to remain in a dislocated position for 6 months. While the restriction in movements immediately after the injury could have been due to edema, the absence of movements even 2 weeks after surgery should have raised the surgeon’s suspicion. The forearm radiograph, however, ended up giving the surgeon and patient false reassurance about the status of the elbow. Separate radiographs of the anteroposterior and lateral view of the elbow joint make the diagnosis of subluxations and dislocations much more obvious [5]. A lateral radiograph of the forearm, even if the elbow joint is covered in it cannot substitute a lateral radiograph of the elbow done in 90° flexion [6]. It is also recommended to repeat the elbow radiographs 1 week after the injury or initiate treatment to confirm the status of the elbow and identify the failure of the treatment [7]. Neglected elbow dislocation is defined as a dislocation that is present for 3 weeks or longer [8]. Such neglected elbows can increase the likelihood of complications of dislocation such as elbow instability and neurovascular injury [9]. While loss of movements following dislocation is common, it is usually due to flexion contracture of the anterior capsule, contracture of collateral ligaments, contracture of surrounding musculature, articular incongruity, or fracture fragments causing a mechanical block. Peri-articular heterotrophic bone formation is also common but seldom causes a block in motion. Ankylosis of the elbow following a dislocation is extremely rare [10]. There is scarce literature available on this rare complication of neglected elbow dislocations. Neglected elbow dislocations pose a complex challenge to manage and necessitate a multifaceted approach. Initially, a thorough evaluation, including radiographic assessment, aids in determining joint congruity, the presence of osteochondral lesions, and soft-tissue integrity [11]. Conservative measures may be attempted for stable but neglected cases, focusing on rehabilitation to regain range of motion and strength. Surgical options, such as open reduction, ligament reconstruction, or osteochondral grafting, are often required for unstable or chronic cases [12, 13]. Addressing associated deformities and complications is vital, including radial head excision for irreparable injuries [14]. The duration from initial dislocation is also important in determining the appropriate treatment. Attempting closed reduction for an elbow dislocation beyond 21 days post-injury is generally unsuccessful. Open reduction within 3 months typically yields satisfactory outcomes, but after 6 months, results become less favorable, prompting consideration of arthroplasty as an alternative [15]. A tailored approach, considering joint status, patient factors, and functional goals, is essential to achieve the best possible outcome. In this patient, two fundamental mistakes lead to an adverse outcome for the patient. First, a separate radiograph of the elbow was not performed. Second, when the patient was reviewed 1 week after the injury, the same forearm radiograph was relied upon rather than a new radiograph of the elbow. This misled the surgeon, leading him to immobilize the limb, which worsened the problem [16].
This case demonstrates that neglected elbow dislocations can lead to ankylosis of the joint. It also shows how radiographs of the forearm are inadequate to assess for elbow dislocations even if the elbow region is covered in the radiograph.
- Neglected elbow dislocations can lead to ankylosis of the joint
- Radiographs of the forearm are inadequate to assess for elbow dislocations even if the elbow region is covered in the radiograph
- Separate radiographs of the elbow are essential. If there is doubt, a 3D CT of the elbow should be done.
References
- 1.Cohen MS, Hastings H. Acute elbow dislocation: Evaluation and management. J Am Acad Orthop Surg 1998;6:15-23. [Google Scholar]
- 2.Graf DN, Fritz B, Bouaicha S, Sutter R. Elbow instability. Semin Musculoskelet Radiol 2021;25:574-9. [Google Scholar]
- 3.Martin BD, Johansen JA, Edwards SG. Complications related to simple dislocations of the elbow. Hand Clin 2008;24:9-25. [Google Scholar]
- 4.Layson J, Best BJ. Elbow dislocation. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. Available from: http://www.ncbi.nlm.nih.gov/books/NBK549817 [Last accessed on 2022 Jul 23]. [Google Scholar]
- 5.Tan DJ, Tan TW, Tay GM, Lee NK, Chew EM, Mahadev A, et al. Using the radiocoronoid line for diagnosis of elbow dislocation. J Pediatr Orthop B 2022;31:442-8. [Google Scholar]
- 6.Kim HH, Gauguet JM. Pediatric elbow injuries. Semin Ultrasound CT MR 2018;39:384-96. [Google Scholar]
- 7.Duparc F, Merlet MC. Prevention and management of early treatment failures in elbow injuries. Orthop Traumatol Surg Res 2019;105:S75-87. [Google Scholar]
- 8.Pal CP, Mittal V, Dinkar KS, Kapoor R, Gupta M. Neglected posterior dislocation of elbow: A review. J Clin Orthop Trauma 2021;18:100-4. [Google Scholar]
- 9.Donohue KW, Mehlhoff TL. Chronic elbow dislocation: Evaluation and management. J Am Acad Orthop Surg 2016;24:413-23. [Google Scholar]
- 10.Khanna V, Gupta A, Kumar S. Outcome of long standing ulno-humeral dislocation managed by open reduction and stabilization with V-Y plasty; Our experience. Bull Emerg Trauma 2017;5:259-65. [Google Scholar]
- 11.Islam S, Jahangir J, Manzur RM, Chowdury AA, Tripura N, Das A. Management of neglected elbow dislocations in a setting with low clinical resources. Orthop Surg 2012;4:177-81. [Google Scholar]
- 12.Elzohairy MM. Neglected posterior dislocation of the elbow. Injury 2009;40:197-200. [Google Scholar]
- 13.Anderson DR, Haller JM, Anderson LA, Hailu S, Chala A, OʼDriscoll SW. Surgical treatment of chronic elbow dislocation allowing for early range of motion: Operative technique and clinical results. J Orthop Trauma 2018;32:196-203. [Google Scholar]
- 14.Atkinson CT, Pappas ND, Lee DH. Irreducible posterolateral elbow dislocation. Am J Orthop (Belle Mead NJ) 2014;43:E34-6. [Google Scholar]
- 15.Bruce C, Laing P, Dorgan J, Klenerman L. Unreduced dislocation of the elbow: Case report and review of the literature. J Trauma 1993;35:962-5. [Google Scholar]
- 16.Reiter AJ, Schott HR, Castile RM, Cannon PC, Havlioglu N, Chamberlain AM, et al. Early joint use following elbow dislocation limits range-of-motion loss and tissue pathology in posttraumatic joint contracture. J Bone Joint Surg Am 2023;105:223-30. [Google Scholar]









