This report is the first study evaluating the post-surgical outcomes of patients received bio-integrative screws for their tarsometatarsal (TMT) joint fixation to date.
Dr. Alireza Ebrahimi, Foot and Ankle Research and Innovation Lab, Department of Orthopaedic Surgery, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts. E-mail: aebrahimi@mgh.harvard.edu
Introduction: Various methods are used for open reduction and internal fixation of Lisfranc injuries, and each shows different post-treatment outcomes. Other than the common post-surgery problems in these patients, including possible non-anatomical reduction, implant loosening, breakage, and arthritis, most of these patients will undergo a second surgery for implant removal which itself might cause further complications. To reduce the need for re-operation, bio-degradable or bio-integrative implants can be promising; however, the short- and long-term outcomes have been scarcely investigated to date.
Case Report: We followed up 10 adult patients who received bio-integrative screws for Lisfranc injuries. The patients were asked to fill out the patient-reported outcome measures (PROMs) surveys during one of the follow-up visits. We gathered variables including the type of injury, pain score, and PROMs including physical function (PF), pain interference, pain intensity, and depression. We evaluated the patients for wound dehiscence, non-union, and hardware failure. The median (interquartile range [IQR]) follow-up time of the patients in this study was 9 (4–11.5) months. Nine out of 10 patients with Lisfranc injuries who received bio-integrative screws showed improvements in their pain scores and started progressive weight-bearing. Among 3 patients who had sport-related Lisfranc injuries, 2 returned to play in <6 months, and one started side-to-side agility work in <3 months. The median (IQR) scores of PROMs representing PF, depression, physical health, mental health, pain interference, and pain intensity were 49.5 (30.1–61.9), 41 (41–49), 50.8 (39.2–57.7), 59 (48.9–63.7), 51.7 (41.6–72.6), and 43.5 (37.8–55.2), respectively.
Conclusion: Our results demonstrated promising short-term outcomes of using bio-integrative screws in patients with Lisfranc injuries based on PROMs and the rate of complications. Future studies on larger populations and more comprehensive variables with longer follow-up duration should be the next step in evaluating the pros and cons of these new implants.
Keywords: Bio-integrative implant, revision surgery, implant removal, Lisfranc complications.
Lisfranc injuries, caused by low-energy and high-energy traumas, could vary from ligamentous sprains to complex fractures [1, 2]. The incidence of Lisfranc injuries was estimated to be 9.2/100,000 person-year, and men and young individuals in their third decade of life appeared to be more susceptible to the injury [1, 3]. The treatment method for Lisfranc injuries is decided based on the severity of the injuries as well as the patients’ characteristics [4, 5]. The injuries with less than subtle malalignment could be managed nonoperatively while open reduction and internal fixation (ORIF) and arthrodesis might be indicated for more severe cases [5]. Different instruments and implants are used for both ORIF and arthrodesis including plates, screws, K-wires, staples, and flexible fixation [6, 7]. Most of these implants are metallic and impose the need for second removal surgery on the patients aside from other complications such as loosening and breakage that can cause further psychosomatic and economic burden on the patients and the health-care system [8, 9]. Thus, resolving the need for a second operation that is provided by bio-absorbable and bio-integrative implants has become a focus of various research in orthopedic surgery [10]. A preclinical study on rabbit models with cylindrical bone defects in the femur showed that using bio-absorbable screws could lead to higher rates of bone healing by increasing vascularization and bone regeneration [10, 11]. While the application of bio-integrative implants is still limited, this could revolutionize the care of patients with orthopedic injuries if the implants’ built-in properties ensure a functionally stable connection between the bones and the implant surface [11]. The current study is a case series of 10 patients receiving bio-integrative screws for their Lisfranc injuries. Herein, we report the patient-reported outcome measures (PROMs) and the complications in these patients over at least 3 months of follow-up.
This is a retrospective case-series study on 10 adult patients with Lisfranc injury who underwent tarsometatarsal (TMT) fixation using bio-integrative screws (OSSIOfiber™). The inclusion criteria were: (1) patients with Lisfranc injury with documented instability on weight-bearing computed tomography scan when compared to the contralateral side, (2) receiving surgical fixation of TMT joint, (3) using bio-integrative implant, (4) being ≥18 years old, and (5) having at least 2 months of follow-up. The exclusion criteria were (1) patients who received metal implants, (2) concomitant injuries that affect the PROMs reported by the patient during the follow-up visits, and (3) patients who have not filled out PROMs surveys. The study protocol was approved by the institutional review board (IRB no. 2015P000464). Patients’ charts were reviewed to gather information about the treatment method, pain score (Visual Analog Scale), and reported complications in the postoperative follow-up visits.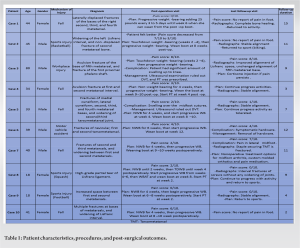
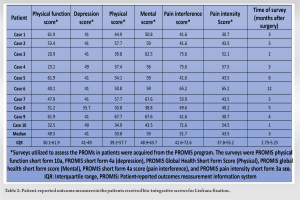
The patients’ demographic data, diagnosis, mechanism of injury, procedure, pain scores, and complications in follow-up visits are presented in Table 1. The median (IQR) age of patients with Lisfranc injury who received bio-integrative screws was 39.5 (29.2–44.2), ranging from 18 years old to 80 years old. Of these 10 patients, five were female (50%), and five were male (50%). The median (IQR) of body mass index of patients was 27.76 (24.9–37.3), with the minimum and maximum being 23.9 and 68.3, respectively. The mechanisms of injury included fall (n = 5), sports injury (n = 3), motor vehicle accident (MVA) (n = 1), and work-related injury (n = 1). All patients had TMT ORIF for Lisfranc injury. The median (IQR) of patients’ follow-up duration was 9 (4–11.5). Among the patients, nine showed promising outcomes as their pain scores evaluated in follow-up visits decreased. These patients began progressive weight-bearing, and two returned to sports (case no. 8 after 5 months and case no. 9 after 4 months). Case no. 8 was a young female squash player who came to the clinic after a twisting injury, leading to a high-grade partial Lisfranc ligament tear with 2nd TMT subluxation (Fig. 1). The procedures done for the patient were Lisfranc ORIF, 1st TMT ORIF, and inter-cuneiform ORIF (Figs. 2 and 3). Another patient (case no. 9) who returned to playing 4 months after the surgical procedure was an 18-year-old girl with increased space between her first and second metatarsal bones who received Lisfranc ORIF, 2nd TMT ORIF, and inter-cuneiform ORIF. The symptoms of one patient (case no. 6) who had MVA did not improve, leading to a second surgical intervention. Case no. 6 was a patient MVA leading to multiple fractures, including metatarsal bones. First and second TMT fusions and inter-cuneiform fixation were done for the patients. However, the patient remained symptomatic and needed a second surgical intervention to remove the hardware. Table 2 represents the PROMs in patients who received Lisfranc fixation using bio-integrative screws. The median (IQR) scores of PROMs representing PF, depression, physical health, mental health, pain interference, and pain intensity were 49.5 (30.1–61.9), 41 (41–49), 50.8 (39.2–57.7), 59 (48.9–63.7), 51.7 (41.6–72.6), and 43.5 (37.8–55.2), respectively. The surveys were done in one of the patients’ post-operation follow-up visits with the median (IQR) of 3 (2.75–5.25) months.
In addition, we reported the PROMs of the Lisfranc patients who received bio-integrative screws and monitored the complications that occurred at least 2 months’ postoperatively. According to the T-score maps and the PROMs, the patients could conduct daily activities and never felt depressed during the study period. In addition, PROMIS global health scores in patients who received bio-integrative screws for Lisfranc injury shows that they were as healthy as the general population, both physically and mentally. Although with a median (IQR) Pain interference score of 51.7 (41.6–72.6), the patients had slight pain during daily and social activities, the pain intensity scores were within the normal range. In conclusion, this report is the first study evaluating the post-surgical outcomes of patients received bio-integrative screws for their TMT joint fixation. We observed that the patients who received the treatment as part of their primary Lisfranc fixation did not require any further intervention. However, as the implants are made of radiolucent materials, we needed to examine anatomical landmarks to assess the joint alignments after the surgery and during the follow-up period. Further studies with a longer-term follow-up are needed to evaluate these results.
The incidence of Lisfranc Injury is estimated to be 9.2/100,000 person-year, and young individuals in their third decade of life appeared to be more susceptible to the injury. Various methods are used for ORIF of Lisfranc injuries, and each shows different post-treatment outcomes. In the current study, 9 out of 10 patients receiving bio-integrative screw showed promising outcomes as their pain scores decreased in follow-up visits. These patients began progressive weight-bearing, and two returned to sports in <6 months. The PROMs representing of PF, depression, physical health, mental health, and pain intensity were within normal ranges during the follow-up period.
Most of the implants used for ORIF are metallic and impose the need for second removal surgery on the patients aside from other complications such as loosening and breakage that can cause further psychosomatic and economic burdens on the patients and the healthcare system. Resolving the need for a second operation that is provided by bio-absorbable and bio-integrative implants has become a focus of various research in orthopedic surgery. The current study reported the treatment outcomes of 10 patients receiving bio-integrative screws for their Lisfranc injuries.
References
- 1.Chen J, Sagoo N, Panchbhavi VK. The Lisfranc injury: A literature review of anatomy, etiology, evaluation, and management. Foot Ankle Spec 2021;14:458-67. [Google Scholar]
- 2.Ponkilainen VT, Mattila VM, Laine HJ, Paakkala A, Mäenpää HM, Haapasalo HH. Nonoperative, open reduction and internal fixation or primary arthrodesis in the treatment of Lisfranc injuries: A prospective, randomized, multicenter trial-study protocol. BMC Musculoskelet Disord 2018;19:301. [Google Scholar]
- 3.Ponkilainen VT, Laine HJ, Mäenpää HM, Mattila VM, Haapasalo HH. Incidence and characteristics of midfoot injuries. Foot Ankle Int 2019;40:105-12. [Google Scholar]
- 4.Coetzee JC. Making sense of lisfranc injuries. Foot Ankle Clin 2008;13:695-704, ix. [Google Scholar]
- 5.Seybold JD, Coetzee JC. Lisfranc injuries: When to observe, fix, or fuse. Clin Sports Med 2015;34:705-23. [Google Scholar]
- 6.Weening B, Bhandari M. Predictors of functional outcome following transsyndesmotic screw fixation of ankle fractures. J Orthop Trauma 2005;19:102-8. [Google Scholar]
- 7.Grewal US, Onubogu K, Southgate C, Dhinsa BS. Lisfranc injury: A review and simplified treatment algorithm. Foot (Edinb) 2020;45:101719. [Google Scholar]
- 8.Lalli TA, Matthews LJ, Hanselman AE, Hubbard DF, Bramer MA, Santrock RD. Economic impact of syndesmosis hardware removal. Foot (Edinb) 2015;25:131-3. [Google Scholar]
- 9.Sripanich Y, Weinberg MW, Krähenbühl N, Rungprai C, Haller J, Saltzman CL, et al. Surgical outcome of chronic Lisfranc injury without secondary degenerative arthritis: A systematic literature review. Injury 2020;51:1258-65. [Google Scholar]
- 10.Baravarian B, Lindner TP, Merchav-Feuermann R. Advancements in bone fixation utilizing novel biointegrative fixation technology. Clin Podiatr Med Surg 2018;35:53-62. [Google Scholar]
- 11.Sharma CP, editor. Biointegration of Medical Implant Materials. 2nd ed. United Kingdom: Woodhead Publishing (An imprint of Elsevier); 2019. (Woodhead Publishing Series in Biomaterials). [Google Scholar]
- 12.Cella D, Choi SW, Condon DM, Schalet B, Hays RD, Rothrock NE, et al. PROMIS® adult health profiles: Efficient short-form measures of seven health domains. Value Health 2019;22:537-44. [Google Scholar]
- 13.O’Hara NN, Richards JT, Overmann A, Slobogean GP, Klazinga NS. Is PROMIS the new standard for patient-reported outcomes measures in orthopaedic trauma research? Injury 2020;51:S43-50. [Google Scholar]
- 14.HealthMeasures. T-score Maps. T-score Maps. Available from: https://staging.healthmeasures.net/score-and-interpret/interpret-scores/promis/t-score-maps [Last accessed on 2023 Apr 18]. [Google Scholar]
- 15.Stone AA, Broderick JE, Junghaenel DU, Schneider S, Schwartz JE. PROMIS fatigue, pain intensity, pain interference, pain behavior, physical function, depression, anxiety, and anger scales demonstrate ecological validity. J Clin Epidemiol 2016;74:194-206. [Google Scholar]
- 16.Wynter S, Grigg C. Lisfranc injuries. Aust Fam Physician 2017;46:116-9. [Google Scholar]
- 17.Philpott A, Epstein DJ, Lau SC, Mnatzaganian G, Pang J. Lisfranc fixation techniques and postoperative functional outcomes: A systematic review. J Foot Ankle Surg 2021;60:102-8. [Google Scholar]
- 18.Levy CJ, Yatsonsky D 2nd, Moral MZ, Liu J, Ebraheim NA. Arthrodesis or open reduction internal fixation for Lisfranc injuries: A meta-analysis. Foot Ankle Spec 2022;15:179-84. [Google Scholar]
- 19.Buda M, Kink S, Stavenuiter R, Hagemeijer CN, Chien B, Hosseini A, et al. Reoperation rate differences between open reduction internal fixation and primary arthrodesis of Lisfranc injuries. Foot Ankle Int 2018;39:1089-96. [Google Scholar]
- 20.Smith N, Stone C, Furey A. Does open reduction and internal fixation versus primary arthrodesis improve patient outcomes for Lisfranc trauma? A systematic review and meta-analysis. Clin Orthop Relat Res 2016;474:1445-52. [Google Scholar]
- 21.Meyerkort DJ, Gurel R, Maor D, Calder JD. Deep peroneal nerve injury following hardware removal for Lisfranc joint injury. Foot Ankle Int 2020;41:320-3. [Google Scholar]
- 22.Reith G, Schmitz-Greven V, Hensel KO, Schneider MM, Tinschmann T, Bouillon B, et al. Metal implant removal: Benefits and drawbacks--a patient survey. BMC Surg 2015;15:96. [Google Scholar]











