We demonstrate the benefits of 3D-printed models in spine surgery, illustrating their role in pre- and post-operative planning, enhancing intraoperative efficiency, and increasing patient satisfaction, particularly in cases of Bertolotti syndrome.
Dr. James P Caruso, Department of Neurosurgery, The University of Texas Southwestern, 5151 Harry Hines Blvd, Dallas, Texas. E-mail: james.caruso@phhs.org
Background: Three-dimensional (3D) printing has enabled numerous advances in spine surgery execution and education. However, few examples exist to outline how this technology can aid the performance of complex spine surgery using minimally invasive surgery (MIS) techniques. Therefore, we present a case that illustrates the benefits of 3D-printed spine model production before and after correction of a case with Bertolotti Syndrome using a MIS approach.
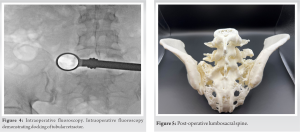
Case Presentation: A 40-year-old woman with Bertolotti syndrome underwent staged bilateral L6 MIS transverse process resection for the treatment of severe and progressive axial back pain which had repeatedly failed conservative management. 3D-printed spine models were used for pre- and post-operative surgical planning and patient counseling.
Conclusion: 3D-printed spine models can aid in the planning of complex spine cases suited for a MIS approach.
Keywords: 3D printing, anatomy, Bertolotti syndrome, minimally invasive, spine model.
In recent years, minimally invasive spine surgery (MISS) approaches have become increasingly versatile and can be applied safely and successfully in a variety of complex spine pathologies [1]. The number of instrumented MISS procedures performed in the United States continues to increase [2], and cost savings can range from $8,731 to $9,295 for MIS compared to open spine surgeries [3]. In addition, MISS can minimize complications and aid in post-operative quality of life improvement [1, 4-6] since many patients who undergo MISS experience reduced risk of intraoperative and perioperative adverse outcomes, shorter operative times, and earlier returns to work [6, 7]. However, while MISS approaches may benefit patient recovery, smaller incisions and operative working windows can increase the complexity of cases with aberrant anatomy or congenital deformities. To address these challenges, three-dimensional (3D) printing can serve as a helpful adjunct for surgical preparation and patient education [8], and many surgical subspecialties have adopted 3D-printing practices to improve pre- and intraoperative workflows [9-12]. However, the widespread use of 3D-printing applications in MISS can be limited by material cost, time, and a specialized market associated with the procedures [13]. To demonstrate the utility of 3D-printing in MISS, we present a rare case of Bertolotti syndrome requiring bilateral staged L6 transverse process (TP) resection, in which a 3D-printed models of the patient’s lumbosacral spine were used for pre-, intra-, and post-operative surgical planning and patient education.
A 40-year-old woman presented with over 10 years of axial back pain. Her pain significantly worsened with her last pregnancy a year prior, was refractory to maximal pharmacologic therapy and to repeated corticosteroid injections, which only provided her with a few days of relief, and limited her ability to ambulate and perform activities of daily living. On physical examination, paraspinal palpation at the level of the lumbosacral junction elicited severe pain, worse on the left compared to the right. Her bilateral lower extremity strength and sensation were preserved. Computed tomography (CT) of her lumbar spine revealed six lumbar vertebrae, bilateral L6 TP hypertrophy with aberrant degenerative changes at sites of articulation with the posterior superior iliac spine (Fig. 1).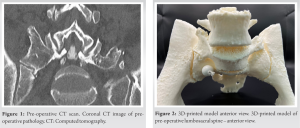
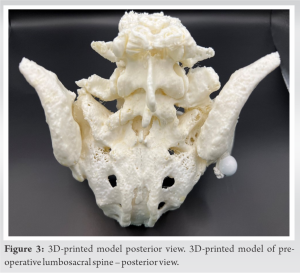
Bertolotti syndrome often presents with chronic axial back pain [14]. Enlarged TPs at the caudal lumbar vertebral level develop anomalous articulations with the sacrum or ilium, leading to accelerated lumbosacral degeneration and associated disk degeneration and discogenic pain and superior lumbar vertebral levels [14]. The underlying pathophysiology driving this process is unclear, but it often results in restricted range of motion and functional limitations. Surgical management consists of either lumbosacral fusion or resection of the hypertrophic TP, which can carry substantial complexity due to the associated aberrant congenital anatomy.
In this case, a 3D-printed full-scale model of the patient’s lumbosacral spine allowed the surgeons to better visualize the patient’s anatomy to achieve an adequate degree of TP resection, which depended on precise docking of the tubular retractor along the TP during the approach adjacent to the iliac crest. During the procedure, we frequently referenced the model to ensure that we were docked adequately on the aberrant Bertolotti TP-pelvic articulation, rather than incorrectly on the sacroiliac joint. In addition, the minimal financial cost and time required to produce the models render them useful training tools when preparing for cases with unique anatomy. For specific cranial neurosurgery applications, augmented reality can provide a similar benefit [15], but a palpable intraoperative reference object provides superior tactile feedback. In addition, in the post-operative setting, the patient expressed gratitude for being able to directly visualize her anatomy using the model. While this feedback is anecdotal and informal, patient satisfaction is an essential component of successful spine surgery, and introducing 3D-printed models in pre- and post-operative evaluations may promote this. 3D-printing applications in spine surgery continue to evolve, and further, progress is necessary to develop anatomically faithful individualized 3D models that account for bone quality to better predict the likelihood of biomechanical success after spine surgery.
Low-cost 3D-printed models can assist with anatomic visualization and patient counseling for MISS cases with complex or aberrant anatomy, and they are a useful tool to improve intraoperative workflow and patient satisfaction.
In an effort to demonstrate the advantages of using three-dimensional (3D)-printed models in spine surgery, we present a case where 3D-printed spine models were used for pre- and post-operative surgical planning and patient counseling in a patient with Bertolotti syndrome. We show how 3D-printed models assist with visualizing complex anatomical features even when restricted by the smaller incisions and operative working windows of MIS spine surgery. These models are a useful tool to improve intraoperative workflow and patient satisfaction.
References
- 1.Spetzger U, Von Schilling A, Winkler G, Wahrburg J, König A. The past, present and future of minimally invasive spine surgery: A review and speculative outlook. Minim Invasive Ther Allied Technol 2013;22:227-41. [Google Scholar]
- 2.Phillips FM, Cheng I, Rampersaud YR, Akbarnia BA, Pimenta L, Rodgers WB, et al. Breaking through the “glass ceiling” of minimally invasive spine surgery. Spine (Phila Pa 1976) 2016;41:S39-43. [Google Scholar]
- 3.Hopkins B, Mazmudar A, Kesavabhotla K, Patel AA. Economic value in minimally invasive spine surgery. Curr Rev Musculoskelet Med 2019;12:300-4. [Google Scholar]
- 4.Bae J, Lee SH. Minimally invasive spinal surgery for adult spinal deformity. Neurospine 2018;15:18-24. [Google Scholar]
- 5.Vaishnav AS, Othman YA, Virk SS, Gang CH, Qureshi SA. Current state of minimally invasive spine surgery. J Spine Surg 2019;5:S2-10. [Google Scholar]
- 6.Yoon JW, Wang MY. The evolution of minimally invasive spine surgery: JNSPG 75th anniversary invited review article. J Neurosurg Spine 2019;30:149-58. [Google Scholar]
- 7.Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR. Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: Meta-analysis and systematic review. J Neurosurg Spine 2016;24:416-27. [Google Scholar]
- 8.Yamaguchi JT, Hsu WK. Three-dimensional printing in minimally invasive spine surgery. Curr Rev Musculoskelet Med 2019;12:425-35. [Google Scholar]
- 9.Yamada T, Osaka M, Uchimuro T, Yoon R, Morikawa T, Sugimoto M, et al. Three-dimensional printing of life-like models for simulation and training of minimally invasive cardiac surgery. Innovations (Phila) 2017;12:459-65. [Google Scholar]
- 10.Barber SR, Kozin ED, Dedmon M, Lin BM, Lee K, Sinha S, et al. 3D-printed pediatric endoscopic ear surgery simulator for surgical training. Int J Pediatr Otorhinolaryngol 2016;90:113-8. [Google Scholar]
- 11.Weinstock P, Rehder R, Prabhu SP, Forbes PW, Roussin CJ, Cohen AR. Creation of a novel simulator for minimally invasive neurosurgery: Fusion of 3D printing and special effects. J Neurosurg Pediatr 2017;20:1-9. [Google Scholar]
- 12.Izatt MT, Thorpe PL, Thompson RG, D’Urso PS, Adam CJ, Earwaker JW, et al. The use of physical biomodelling in complex spinal surgery. Eur Spine J 2007;16:1507-18. [Google Scholar]
- 13.Hsu MR, Haleem MS, Hsu W. 3D printing applications in minimally invasive spine surgery. Minim Invasive Surg 2018;2018:4760769. [Google Scholar]
- 14.Crane J, Cragon R, O’Neill J, Berger AA, Kassem H, Sherman WF, et al. A comprehensive update of the treatment and management of Bertolotti’s syndrome: A best practices review. Orthop Rev (Pavia) 2021;13:24980. [Google Scholar]
- 15.Sheth SA, Bijanki KR, Metzger B, Allawala A, Pirtle V, Adkinson JA, et al. Deep brain stimulation for depression informed by intracranial recordings. Biol Psychiatry 2022;92:246-51. [Google Scholar]