Posterior decompression and fusion effectively treat spondylodiscitis and neurological deficits in the cervical spine following head-and-neck radiotherapy, with separate skin incisions and avoiding anterior approaches to reduce infection spread and complications.
Dr. Satoshi Maki, Department of Orthopaedic Surgery, Graduate School of Medicine, Chiba University, 1-8-1 Inohana, Chuou-Ku, Chiba 260-8670, Japan. E-mail: satoshimaki@gmail.com
Introduction: Cervical spondylodiscitis due to osteoradionecrosis (ORN) after head-and-neck cancer radiotherapy is a severe complication. However, there are few reports on the surgical treatment of this condition.
Case Report: We report two cases of cervical spondylodiscitis due to ORN, which were successfully treated with posterior decompression and fusion. The first case was in a 73-year-old male patient with spondylodiscitis at C3–C5, due to ORN. A posterior fusion of the spine (C2–T1) was performed, and a biopsy was conducted at a site separate from the incision for fusion. The second case was in a 76-year-old female patient with spondylodiscitis due to C4–C7 ORN. Cervical posterior decompression and fusion (C2–Th2) were performed, and decompression (C5–6) was conducted through an incision separate from that for the fusion. An anterior approach was avoided in both cases because of radiation-induced tissue changes. For these two patients with cervical spondylodiscitis due to ORN, surgery resulted in an improvement of infection and neurological deficits by posterior spinal fusion, isolation from decompression or biopsy of the infected area, and antibiotic treatment.
Conclusion: Posterior decompression and fusion are effective for spondylodiscitis in the cervical spine after head-and-neck radiotherapy, treating both infection and neurological deficits. Spinal fusion that avoids the level of the infected vertebral body and decompression from separate skin incision sites may prevent the spread of infection. An anterior approach should be avoided because the risk of esophageal perforation and posterior pharyngeal wall defects is high.
Keywords: Cervical spondylodiscitis, osteoradionecrosis, radiotherapy, posterior fusion surgery.
Cervical spondylodiscitis due to osteoradionecrosis (ORN) after head-and-neck cancer radiotherapy is a severe complication. Mandibular ORN is a well-described complication following radiotherapy of the head and neck [1]. The literature reports that doses exceeding 60 Gy increase the risk of ORN [2]. Radiation has side effects in normal tissue, including homeostatic and metabolic cell defects due to hypocellularity, hypoxia, and hypovascularity [3]. As a result, the risk of secondary infection increases [1]. Secondary infections of cervical ORN occur in approximately 40% of patients [4]. ORN in the cervical spine is considered an uncommon disease [5]. However, King et al. [6] reported that 1% (9/884 cases) of cases were associated with cervical ORN among nasopharyngeal carcinoma treated with radiation therapy and stated that ORN is more common than previously suspected. If cervical ORN and secondary infections occur, this may cause cervical instability or spinal cord compression by an epidural abscess, requiring surgical stabilization of the cervical and spinal cord decompression [3]. However, there are few reports on the surgical treatment of cervical spondylodiscitis due to ORN after head-and-neck cancer radiotherapy [3, 7-11]. We report two cases of cervical spondylodiscitis due to ORN, which were improved by posterior decompression and fusion.
Case 1
The first case was a 73-year-old male patient. He had been treated for hypopharynx (stage T1N2bM0) and esophageal cancer by radiotherapy five years ago, when he was 68 years old. The total radiation therapy dose was 70 Gy, consisting of 50 Gy of radiation to the hypopharynx and esophagus, followed by a 20 Gy boost. The lesion disappeared after treatment completion, and no recurrence has been observed. He began to experience neck pain five years after the radiotherapy, and a neck collar was prescribed. However, within a few days, his neck pain (visual analog scale; VAS was 9/10) and cervical kyphotic alignment progressed, and he developed unilateral upper extremity paresis [3 according to the Manual Muscle Test (MMT), right arm] and paresthesia. In addition, he complained about swallowing difficulties due to a neck kyphotic change. A blood examination showed a leukocyte count of 4400/mg and a C-reactive protein (CRP) level of 8.30 mg/dL; an elevated inflammatory response was observed. Severe kyphotic deformity and distraction of the C4 vertebrae, and expansion of the retropharyngeal space were shown in radiography (Fig. 1a). Computed tomography (CT) revealed destruction of the C4 vertebrae and erosion of the C5 vertebrae (Fig. 1b). 
Case 2
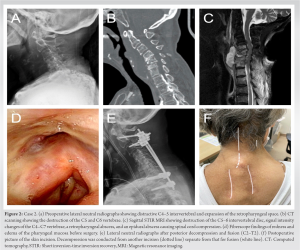
The second case involved a 76-year-old female patient. She had been treated for hypopharynx (stage Ⅳ T2N2bM0) cancer 20 years ago, using radiation and chemotherapy. She had received 60 Gy radiations to the pharynx and 46 Gy to the right supraclavicular fossa, followed by a planned right neck dissection. No recurrence has been observed during the follow-up. However, she began to have neck pain 20 years after the radiotherapy. Within a few days, she developed bilateral upper extremity paresis (3 according to the MMT), paresthesia, and gait disorder. A blood examination showed a leukocyte count of 7700/mg and a CRP level of 9.87 mg/dL; an elevated inflammatory response was observed. Destruction of the C4–5 intervertebral disc and expansion of the retropharyngeal space were shown in radiography (Fig. 2a). CT scanning showed destruction of the C5 and C6 vertebrae (Fig. 2b). Sagittal STIR MRI showed destruction of the C5–6 intervertebral disc, signal intensity changes of the C4–C7 vertebrae, a retropharyngeal abscess, and an epidural abscess causing spinal cord compression (Fig. 2c). A fiberscope showed redness and edema of the pharyngeal mucosa secondary to radiotherapy (Fig. 2d). A puncture of the retropharyngeal abscess was performed through the neck using ultrasound. Streptococcus dysgalactiae was isolated in culture. The patient was diagnosed with spondylodiscitis at levels C4–C7 due to ORN. Cervical posterior decompression and fusion (C2–Th2) were performed on the day of admission. Surgical screw insertion for fixation was performed via three incisions at both the C2-3 and bilateral C7-T1 sites. An ILS was inserted on the left side of C2, and a PS was inserted on the right side of C2, while a PVFS was inserted on the left side of C3, and another PS was inserted on the right side. A PS of C3 was inserted through another 2-cm lateral incision on the left side. For the cervical-thoracic region, PS were bilaterally inserted into T1 and T2, and a rod was then passed under the muscle and connected to the screw heads. As the infected vertebral body at C4–7 was not suitable for direct PS placement, caudal fixation was carried out in T1 and T2. In addition, a C5–6 laminectomy was performed through an incision separate from that for the fusion (Fig. 2f). After surgery, the patient remained intubated and underwent a tracheostomy because of the difficulty of reintubation due to a retropharyngeal abscess and the risk of laryngeal edema after extubation. She was treated with a 6-week course of intravenous antibiotics (SBT/ABPC) and a 19-week course of oral antibiotics (AMPC and CVA). The infection was controlled, and the retropharyngeal abscess improved. The tracheotomy cannula was removed after one month. Postoperatively, bilateral upper extremity paresis, paresthesia, and gait disorder improved. To date, 10 months after surgery, the patient’s neurological condition is stable.
After head-and-neck cancer radiotherapy, posterior decompression and fusion are effective for treating spondylodiscitis in the cervical spine and treating infections and neurological deficits. Spinal fusion that avoids the infected vertebral body level and decompression from separate skin incisions may prevent the spread of infection. An anterior approach should be avoided because the risk of esophageal perforation and posterior pharyngeal wall defects is high. Posterior fusion surgery, which improves infection and neurological deficits, has fewer complications than anterior surgery, especially in cervical spondylodiscitis after head-and-neck cancer radiotherapy. Moreover, posterior decompression and fusion surgery generally lead to favorable clinical outcomes for pyogenic spondylodiscitis [13]. These favorable outcomes are because posterior fusion stabilizes the infected vertebral body and the disc space, enhancing antibiotic penetration and tissue healing [14]. In cervical spondylodiscitis due to ORN following radiotherapy, there are some reports of posterior fusion surgery [8-10]. Eenhuis et al. [8] reported the cases of three patients who were treated for cervical spondylodiscitis due to ORN using posterior fixation surgery and antibiotic treatment without debridement. They stated that even when the tissue structures of the posterior pharyngeal wall are altered by irradiation and an anterior approach is not possible, a combination of lifelong antibiotic treatment and posterior stabilization is a good alternative. West et al. [9] and Cheung et al. [10] reported successful treatment of spondylodiscitis due to ORN of the craniocervical junction using posterior spinal fusion and hyperbaric oxygen therapy. Similarly, in our present cases, patients with cervical spondylodiscitis due to ORN after radiotherapy had reduced neurological deficits and no recurrent infections using posterior spinal fusion and antibiotic treatment. In our two cases, antibiotics were administered for 6 months postoperatively, and long-life antibiotic treatment was unnecessary. This might suggest that posterior decompression and fusion surgery lead to favorable clinical outcomes. The spinal fusion that skips the infected vertebral body level and decompression from separate skin incisions may prevent the spread of infection. Both internal fixation and bone fusion are reported to be performed safely in the presence of infection [15]. Whereas Sanda et al. [16] reported that patients with instrumentation have higher rates of reinfection than those with the surgical treatment but without fixation, indicating there may be an increased risk of reinfection due to bacteria on the instrumentation. In our two patients with cervical spondylodiscitis due to ORN, posterior spinal fusion isolated from decompression or biopsy of the infected area and subsequent antibiotic treatment resulted in improvement of infection and neurological deficits, and no reinfection occurred. An anterior approach should be avoided because the risk of esophageal perforation and posterior pharyngeal wall defects is high. Debridement and structural reconstruction of infected areas is the conventional criterion standard for the surgical management of infections [17]. An anterior approach allows direct access to the infected vertebral body and the disc space and enables sufficient debridement and placement of a bone graft for stabilization. Additionally, it allows adequate tissue biopsy to ensure reliable microbiological diagnosis [18]. However, in hypopharyngeal cancer after irradiation or neck dissection, the condition of the tissues covering the anterior part of the vertebral column is poor, and the risk of esophageal perforation and posterior pharyngeal wall defects is high, sometimes making an anterior approach difficult [8, 19]. Cheung et al. [10] reported a case of a patient who had cervical spondylodiscitis due to ORN. The patient underwent anterior decompression and fusion but, because of a posterior pharyngeal wall defect, did not develop the expected bony union. This patient subsequently required a long posterior fusion and a myocutaneous sternocleidomastoid flap for coverage. In both of our patients, no esophageal perforation or posterior pharyngeal wall defect was present, but the anterior approach was difficult because of radiation-induced tissue changes. Additionally, the poor vascularity and hypoxic tissue environment of necrotic regional bone in patients after irradiation pose challenging treatment problems for successful fusion, and the grafts are at higher risk for failure [20]. Kouyoumdjian et al. [21] reported failure of the anterior approach surgery in ORN patients with kyphosis. They stated that a long, isolated posterior or circumferential stabilization should be considered the primary procedure for this type of patient. There are some reports that an anterior approach using vascularized fibular bone grafts has led to favorable outcomes for cervical spondylodiscitis due to ORN. However, these cases were combined with posterior fusion or long-time halo-vest fixation [3, 7, 11]. Therefore, an anterior approach alone might not be sufficient to restore spinal stability, and an additional posterior instrumentation procedure should be considered. The spine surgeon should be aware of some pitfalls of cervical ORN with infection after radiotherapy and adapt the evaluation and surgery.
Posterior decompression and fusion are effective for spondylodiscitis in the cervical spine after head-and-neck cancer radiotherapy, treating both infection and neurological deficits. Spinal fusion that avoids the infected vertebral body level and decompression using separate skin incisions may prevent the spread of infection. An anterior approach should be avoided because the risk of esophageal perforation and posterior pharyngeal wall defects is high.
Cervical spondylodiscitis due to ORN after head-and-neck cancer radiotherapy is a severe complication. However, there are few reports on the surgical treatment of this condition. Posterior decompression and fusion are effective for this type of patient, treating both infection and neurological deficits. An anterior approach should be avoided because the risk of esophageal perforation and posterior pharyngeal wall defects is high.
References
- 1.Lim AA, Karakla DW, Watkins DV. Osteoradionecrosis of the cervical vertebrae and occipital bone: A case report and brief review of the literature. Am J Otolaryngol 1999;20:408-11. [Google Scholar]
- 2.Chung SJ, Wan-Teck L, Tham SC, Tan IB, Wang ML, Khoo JB. Osteoradionecrosis of the cervical spine complicated by pneumocephalus and meningitis in a nasopharyngeal cancer patient radically treated with radiotherapy 11 years ago. BMJ Case Rep 2009;2009:bcr11.2008.1179. [Google Scholar]
- 3.Donovan DJ, Huynh TV, Purdom EB, Johnson RE, Sniezek JC. Osteoradionecrosis of the cervical spine resulting from radiotherapy for primary head and neck malignancies: Operative and nonoperative management. Case report. J Neurosurg Spine 2005;3:159-64. [Google Scholar]
- 4.Smith VA, Lentsch EJ. Life-threatening cervical spine collapse as a result of postradiation osteonecrosis-case report and review of the literature. Head Neck 2013;35:E142-6. [Google Scholar]
- 5.Mut M, Schiff D, Miller B, Shaffrey M, Larner J, Shaffrey C. Osteoradionecrosis mimicking metastatic epidural spinal cord compression. Neurology 2005;64:396-7. [Google Scholar]
- 6.King AD, Griffith JF, Abrigo JM, Leung SF, Yau FK, Tse GM, et al. Osteoradionecrosis of the upper cervical spine: MR imaging following radiotherapy for nasopharyngeal carcinoma. Eur J Radiol 2010;73:629-35. [Google Scholar]
- 7.Powell DK, Jacobson AS, Kuflik PL, Persky MS, Silberzweig JE, Khorsandi AS. Fibular flap reconstruction of the cervical spine for repair of osteoradionecrosis. Spine J 2013;13:e17-21. [Google Scholar]
- 8.Eenhuis LL, Bijl HP, Kuijlen JM, Wedman J. Cervical stabilization in patients with instability resulting from osteoradionecrosis with subsequent spondylodiscitis after radiotherapeutic treatment for head-and neck carcinoma. Indian J Otolaryngol Head Neck Surg 2019;71:784-9. [Google Scholar]
- 9.West JL, Frenkel MB, Renfrow JJ, Wilson JA. Craniocervical osteoradionecrosis treated with neoadjuvant and adjuvant hyperbaric oxygen in combination with posterior spinal fusion. World Neurosurg 2019;126:107-12. [Google Scholar]
- 10.Cheung JP, Wei WI, Luk KD. Cervical spine complications after treatment of nasopharyngeal carcinoma. Eur Spine J 2013;22:584-92. [Google Scholar]
- 11.Ng RL, Beahm E, Clayman GL, Hassenbusch SJ, Miller MJ. Simultaneous reconstruction of the posterior pharyngeal wall and cervical spine with a free vascularized fibula osteocutaneous flap. Plast Reconstr Surg 2002;109:1361-5. [Google Scholar]
- 12.Maki S, Aramomi M, Matsuura Y, Furuya T, Ota M, Iijima Y, et al. Paravertebral foramen screw fixation for posterior cervical spine fusion: Biomechanical study and description of a novel technique. J Neurosurg Spine 2017;27:415-20. [Google Scholar]
- 13.Lin CP, Ma HL, Wang ST, Liu CL, Yu WK, Chang MC. Surgical results of long posterior fixation with short fusion in the treatment of pyogenic spondylodiscitis of the thoracic and lumbar spine: A retrospective study. Spine (Phila Pa 1976) 2012;37:E1572-9. [Google Scholar]
- 14.Mohamed AS, Yoo J, Hart R, Ragel BT, Hiratzka J, Hamilton DK, et al. Posterior fixation without debridement for vertebral body osteomyelitis and discitis. Neurosurg Focus 2014;37:E6. [Google Scholar]
- 15.Lee JS, Suh KT. Posterior lumbar interbody fusion with an autogenous iliac crest bone graft in the treatment of pyogenic spondylodiscitis. J Bone Joint Surg Br 2006;88:765-70. [Google Scholar]
- 16.Sanda M, Singleton A, Yim J, Rahmani R, Sheffels E, Andreshak T. The effect of instrumentation staging on patient outcomes in pyogenic vertebral osteomyelitis: A systematic review. N Am Spine Soc J 2021;8:100083. [Google Scholar]
- 17.Eismont FJ, Bohlman HH, Soni PL, Goldberg VM, Freehafer AA. Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg Am 1983;65:19-29. [Google Scholar]
- 18.Fang D, Cheung KM, Dos Remedios ID, Lee YK, Leong JC. Pyogenic vertebral osteomyelitis: Treatment by anterior spinal debridement and fusion. J Spinal Disord 1994;7:173-80. [Google Scholar]
- 19.Matsuo M, Rikimaru F, Higaki Y, Masuda M. A case of hypopharyngeal cancer with stenosis, perforation, and pyogenic spondylitis development after chemoradiotherapy. Int J Surg Case Rep 2016;20:104-8. [Google Scholar]
- 20.Ariyan S. The survival of free nonvascularized bone grafts in irradiated areas by wrapping in muscle flaps. Plast Reconstr Surg 1984;74:787-8. [Google Scholar]
- 21.Kouyoumdjian P, Gille O, Aurouer N, Soderlund C, Vital JM. Cervical vertebral osteoradionecrosis: Surgical management, complications and flap coverage--a case report and brief review of the literature. Eur Spine J 2009;18 Suppl 2:258-64. [Google Scholar]