Percutaneous extensor tenotomy is a minimally invasive surgical technique and provides pain relief and elbow function improvement in chronic tennis elbow patients.
Dr. Vipin Sharma, Prof and Head , Department of Orthopaedic Surgery, Dr. Rajendra Prasad Government Medical College, Himachal Pradesh, India. E-mail: docvipinsharma@gmail.com
Background: Tennis elbow (lateral epicondylitis elbow) is a self-limiting disease of indeterminate pathogenesis. Conservative therapy is the treatment of choice. In chronic tennis elbow with failure of conservative therapy; surgical treatment is a method of choice. Percutaneous tenotomy of extensor origin for patients with chronic tennis elbow is a minimally invasive technique with better long-term outcomes.
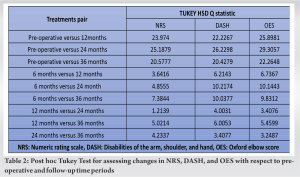
Case Report: Ten patients (six males, four females) presented with chronic tennis elbow, who did not respond to conservative treatment/non-surgical intervention for more than 6 months underwent percutaneous tenotomy in an outpatient setting. Two patients were lost to follow-up at 2 months’ post-operative. The remaining eight patients were evaluated at a mean follow-up of 3 years and assessed using the numerical rating scale, disabilities of the arm, shoulder and hand questionnaire ,and Oxford elbow score. These scores had a statistically significant difference in baseline to 3-year follow-up values (P < 0.05). No adverse outcomes, recurrence of symptoms, and signs of lateral epicondylitis elbow were noted and none required open surgical release.
Conclusion: Percutaneous tenotomy, a minimally invasive technique is an effective and well-tolerated treatment for chronic tennis elbow and gives good pain relief and functional recovery.
Keywords: Extensor carpi radialis brevis, lateral epicondylitis, percutaneous tenotomy, tennis elbow.
Tennis elbow (lateral epicondylitis) is a prevalent and well-recognized disease that induces discomfort in the lateral region of the elbow. As an upper extremity musculoskeletal disorder that is frequently encountered, it impacts approximately 1–3% of the global adult population annually [1]. Middle-aged individuals are most commonly affected, with symptoms typically persisting for 6 months–2 years [2]. Macroscopic or microscopic tears in the common extensor origin are a universally accepted pathology [3]. In 75% of cases, dominant side is involved indicating it to be a work-related injury [4]. Localized tenderness over the lateral epicondyle and pain in the extensor muscles triggered by gripping or engaging in resisted extension movements of the wrist is the chief presentation. Conservative therapy as non-steroidal anti-inflammatory drugs (NSAIDs), physical therapy, and bracing is a popular option in tennis elbow management but management of chronic lateral epicondylitis is unclear. Surgical treatment is required in 4–11% of patients when symptoms persist [4]. Various surgical techniques, for example, open common extensor origin release, partial excision of extensor origin with repair, Z lengthening of the extensor carpi radialis brevis, excision of the proximal part of the annular ligament, excision of the synovial fringe of the radiohumeral joint, bursectomy, percutaneous release of the common extensor origin, arthroscopic release or a combination of the aforementioned procedures are mentioned in literature [4-6]. Percutaneous technique is a time saving outpatient department (OPD) based minimally invasive procedure which functions by engendering an inflammatory state triggered by the activation of the clotting cascade and the subsequent release of growth factors, thereby transforming the chronic injury into an acute healing state leading to healing and remodeling of tendons. Hence, the present study was undertaken to evaluate the outcomes of minimally invasive percutaneous tenotomy in cases of chronic tennis elbow at our institute.
This case series study was conducted at a tertiary care institute after due approval by the Institutional Research Ethics Committee. Patients who fulfilled inclusion criteria, for example, 30–60 years of age, symptoms >6 months, failed non-surgical management including a previous history of a single dose of corticosteroid injection, and consenting to participate in the study were enrolled. While patients with acute pain or calcification of lateral epicondyle on X-ray findings were excluded from the study. Ten patients (six males, four females) with tennis elbow, who did not respond to conservative treatment/non-surgical intervention for more than 6 months, with a mean age of 46.08 years (Year 2021–2022) were evaluated by history, clinical examination and by preprocedural Numeric Rating Scale (NRS) score, disabilities of the arm, shoulder, and hand (DASH) score and Oxford elbow score (OES). Subsequently, patients were operated by percutaneous tenotomy in outpatient settings under local anesthesia. Pain and functional evaluation was done before surgery and post-operative at 3, 6, 1 year, and 3-year follow-up. Due to early loss to follow-up of two patients, eight patients were available for evaluation at 3-year follow-up using NRS, DASH, and Oxford scores. No adverse outcomes, recurrence of symptoms, and signs of lateral epicondylitis elbow were noted and none required open surgical release.
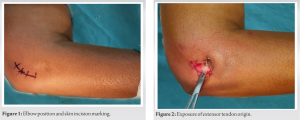
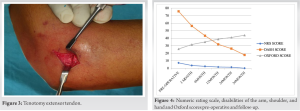
All procedures were performed by the senior surgeon in a tertiary care hospital outpatient environment under local anesthesia at a single institution. A 1 cm incision was made on the lateral epicondyle to expose the extensor origin. After incising deep fascia, the extensor origin was identified. The radial nerve was protected by keeping the elbow in flexion and Forearm in pronation. Entry into the elbow joint, and damage to the annular ligament, capsule, and articular cartilage was avoided. After tenotomy near the origin of extensor tendons, the wrist was flexed to create a 1 cm gap which was palpated to confirm completion of the procedure. Subsequently, the wound was closed and pressure was applied for hemostasis (Fig. 1, 2, 3).
Post-operative rehabilitation
Postoperatively, arm was placed in a sling and patients were advised to mobilize the wrist and elbow multiple times a day including maintaining full pronation of the forearm, fully extending the elbow, and flexing the wrist. Although the patient could carry out day-to-day activities as soon as pain permitted, heavy manual work was allowed after 6 weeks.
Statistical data analysis
The data were analyzed in the SPSS software version 20.0 using descriptive statistics by calculating frequencies and percentages for each parameter in each study group. Mean and standard deviation was computed. Post hoc Tukey test was done to assess changes in various scores. P < 0.05 was considered statistically significant.
Our case series included 10 patients (six males and four females) with an average age of 46.08 years (range 30–60 years) who underwent percutaneous tenotomy for chronic lateral epicondylitis elbow (Table 1).
Conservative therapy is mainstay of treatment in tennis elbow but in a chronic presentation following the failure of conservative treatment, surgical treatment has a role to play. Surgery leads to an early return to daily life activities. Various methods of surgical release of extensor tendons are described in Table 3. In a study comparing percutaneous technique (n = 23) with open technique (n = 22) more satisfactory results were noted for the percutaneous group, with a better DASH score and better patient satisfaction and early return to work in percutaneous group [7]. In our setting, percutaneous tenotomy has been used in patients with chronic tennis elbow having failure of conservative therapy. It is an OPD-based procedure, 10–15 min duration performed under local anesthesia with no requirement of post-operative hospital stay. Extensor tendon is not sutured and no decortication of the lateral epicondyle is done. Only a few studies reporting the long-term outcomes for such minimally invasive procedures are available. Of 10 cases examined in the present study, the majority (37.78%) were 41–50 years, with an average age of 46.09 years. This aligns with numerous studies mentioning its manifestation in the 4th and 5th decades [8]. This age preponderance in the 4th and 5th decades could be due to a decrease in the extensibility of soft tissue and muscle mass bringing them at heightened risk of sustaining injury. 
Percutaneous tenotomy for chronic tennis elbow has a promising potential as a conclusive treatment of chronic elbow tendinopathy. It provides satisfactory pain relief and restoration of functional abilities. This technique is a secure, efficient, and well-accepted alternative for individuals seeking a less invasive treatment option for common extensor tendinopathy, without the associated heightened risks related to general anesthesia and open or arthroscopic surgical procedures.
Chronic tennis elbow is a debilitating condition with limited treatment options available. Percutaneous tenotomy of extensor tendons is a useful and minimally invasive technique to provide pain relief and functional improvement in such conditions.
References
- 1.Mattie R, Wong J, McCormick Z, Yu S, Saltychev M, Laimi K. Percutaneous needle tenotomy for the treatment of lateral epicondylitis: A systematic review of the literature. PM R 2017;9:603-11. [Google Scholar]
- 2.Battista CT, Dorweiler MA, Fisher ML, Morrey BF, Noyes MP. Ultrasonic percutaneous tenotomy of common extensor tendons for recalcitrant lateral epicondylitis. Tech Hand Up Extrem Surg 2018;22:15-8. [Google Scholar]
- 3.Coonrad RW, Hooper WR. Tennis elbow: Its course, natural history, conservative and surgical management. J Bone Joint Surg Am 1973;55:1177-82. [Google Scholar]
- 4.Amroodi MN, Mahmuudi A, Salariyeh M, Amiri A. Surgical treatment of tennis elbow; minimal incision technique. Arch Bone Jt Surg 2016;4:366-70. [Google Scholar]
- 5.Smidt N, Van der Windt DA, Assendelft WJ, Devillé WL, Korthals-de Bos IB, Bouter LM. Corticosteroid injections, physiotherapy, or a wait-and-see policy for lateral epicondylitis: A randomised controlled trial. Lancet 2002;359:657-62. [Google Scholar]
- 6.Terra BB, Rodrigues LM, Filho AN, de Almeida GD, Cavatte JM, De Nadai A. Arthroscopic treatment for chronic lateral epicondylitis. Rev Bras Ortop 2015;50:395-402. [Google Scholar]
- 7.Leppilahti J, Raatikainen T, Pienimäki T, Hänninen A, Jalovaara P. Surgical treatment of resistant tennis elbow. A prospective, randomised study comparing decompression of the posterior interosseous nerve and lengthening of the tendon of the extensor carpi radialis brevis muscle. Arch Orthop Trauma Surg 2001;121:329-32. [Google Scholar]
- 8.Boyer MI, Hastings H 2nd. Lateral tennis elbow: “Is there any science out there?” J Shoulder Elbow Surg 1999;8:481-91. [Google Scholar]
- 9.Samagh P, Sudhakar K, Jindal R. Lateral epicondylitis: Impact on demographic variables. J Ergonomics 2016;6:169. [Google Scholar]
- 10.Solheim E, Hegna J, Øyen J. Extensor tendon release in tennis elbow: Results and prognostic factors in 80 elbows. Knee Surg Sports Traumatol Arthrosc 2011;19:1023-7. [Google Scholar]
- 11.Afzal S, Devgun A, Dhar D. Open release technique in the surgical treatment of tennis elbow. J Orthop 2006;3:e22. [Google Scholar]
- 12.Kayatha N, Joshi A, Chand P, Thapa B, Rana S, Singh B, et al. Treatment outcome of tennis elbow by percutaneous needle tenotomy. MJSBH 2013;11:32-5. [Google Scholar]
- 13.Nazar M, Lipscombe S, Morapudi S, Tuvo G, Kebrle R, Marlow W, et al. Percutaneous tennis elbow release under local anaesthesia. Open Orthop J 2012;6:129-32. [Google Scholar]
- 14.Ang BF, Mohan PC, Png MA, Allen JC Jr., Howe TS, Koh JS, et al. Ultrasonic percutaneous tenotomy for recalcitrant lateral elbow tendinopathy: Clinical and sonographic results at 90 months. Am J Sports Med 2021;49:1854-60. [Google Scholar]