Rare case of bizarre parosteal osteochondromatous proliferation showing pathognomonic features of cortico-medullary continuity and bizarre binucleated chondrocytes with cartilaginous cap.
Dr. Adnan Anwer, Department of Orthopaedic Surgery, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh, Uttar Pradesh, India. Email- dr.adnan.amu@gmail.com
Introduction: Nora’s lesion or bizarre parosteal osteochondromatous proliferation (BPOP) is a rare, benign lesion of small bones of hands and feet in adults. It composed of differing amounts of cartilage, bone, and spindle cells and an unusual form of calcified cartilage so-called “blue bone”.
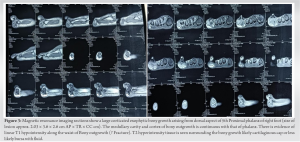
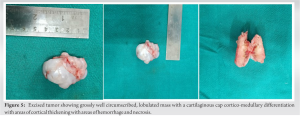
Case Report: A 23-year-old male presented with swelling at the lateral side of the fifth toe of his right foot, which was separated from the adjacent toe. Radiographs showed a mass arising from the proximal phalanx of the little toe, with no medullary and cortical continuity. Excisional biopsy of the mass was performed, and a histologic diagnosis of BPOP of bone (Nora’s lesion) was made.
Conclusion: This case presented with a cartilaginous cap around tumor which is suggestive for benign nature of this tumor with some histological variation from bizarre variant along with no recurrence which is unlikely seen in BPOP.
Keywords: Nora lesion, foot, tumor.
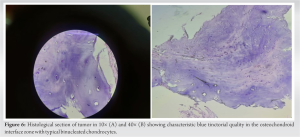
Bizarre parosteal osteochondromatous proliferation (BPOP) is a rare tumor usually seen in small bones (hands less often than feet) of young adults [1]. Classically, it occurs in the second and third decades of life although it was also described in children and long bones of the extremities in later reports. There is no sex predilection [2]. This lesion grows rapidly and has aggressive features on imaging studies as well as confusing findings on histopathologic analysis, leading to many errors in diagnosis and inappropriate treatments. This lesion, which arises from the periosteum, is composed of a cartilaginous cap and bone tissue. Histologically, it exhibits hypercellular cartilage with calcification and ossification, a blue tinctorial quality in osteocartilaginous interfaces, spindle cell stroma with cytologic atypia, and binucleated or bizarre enlarged chondrocytes. The classic radiologic feature of BPOP is a well-marginated mass with a lack of medullary continuity with the bone from which it originates [1]. A thorough clinicopathological correlation is utmost important for the final diagnosis of these heterogeneous lesions as the decision leads to different treatment approaches. Within the spectrum of parosteal osteochondromatous proliferations, “BPOP or Nora’s lesion”, first described by Nora in 1983, is an extremely rare subgroup showing frequent recurrences [2].
A 23-year-old male with pain at the lateral side of the fifth toe of his right foot was seen at an outpatient clinic. He presented with the complaint of a swelling and deformity over the fifth toe of his left foot which was progressively increasing from the past 3 years. It recently advanced in size in the past 7–8 months. It was never associated with pain during course of time. Due to swelling, patient was unable to wear shoes. Physical examination revealed lateralization of the fifth toe with a palpable mass at the lateral aspect of five toe (Fig. 1). On palpating swelling, it was hard in consistency with smooth skin. There was no local rise of temperature or any tenderness. There were no discoloration or secondary changes of skin. However, radiographs showed a bony growth involving proximal, middle and distal phalanx of the fifth toe with cortical breach in proximal phalanx (Fig. 2).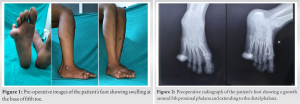

BPOP (Nora’s lesion) was first described by Nora et al. in 1983 [3]. The most frequent locations of BPOP are the proximal and middle phalanges, metacarpals, and metatarsals. It is rarely located at the long tubular bones [1]. The age range is reported as being anywhere between 8 and 74, with the majority in the third or fourth decade of life [4]. It is difficult to diagnose BPOP with respect to histopathological findings and differential diagnosis. It is seen on review of literature that there is considerable overlap in radiological and histological findings of benign and malignant forms of these proliferations [1]. Benign differentials include neoplastic lesions as osteochondroma, subungual exostosis and periosteal chondroma or reactive processes due to trauma as fracture healing, myositis ossificans, florid reactive periostitis (FRP), Turret exostosis (ossifying haematoma or acquired osteochondroma), progressive osseous heteroplasia, and fibrodysplasia ossificans progressive. Yuen and colleagues proposed that this lesion occurs as part of reparative process following an inciting event, often related to trauma [2]. This was supported by Ly et al. who reported the development of this lesion in the upper limb following a traumatic event. Similarly, a history of trauma was elucidated in 30% of the cases described by meneses and colleagues. Hypothesis was proposed by Yuen et al. for proliferative periosteal proliferations and the histological differences among the lesions were explained by their relation to the bone surface, the degree of their breaching of the periosteum and subsequent maturation. Dorfman and Czerniak described the stages, which those lesions pass through while evolving from one entity to another as the lesions mature over time. According to this theory, the first stage is FRP with less cartilaginous elements and evolves to Nora’s lesion characterized with prominent new bone and metaplastic cartilage formation. The stages end with turret exostosis as the ossified and cartilaginous areas are matured. Dhondt et al. conducted study and confirms that the radiological appearances of Nora’s lesion, and demonstrates that these lesions have a spectrum of reactive changes which includes FRP and turret exostosis [5]. Nilsson et al. conducted a cytogenetic study to find the chromosomal abnormality in BPOP and found that t (1;17) (q32;q21), or variant translocations involving 1q32, are recurrent and unique aberrations in BPOP [6]. Surgical resection with wide margins represents the treatment of choice, since BPOP shows a remarked tendency to give local recurrence after therapeutic approach [7]. Time between the first excision and local relapse ranges from 2 months to 2 years, while the time between the second excision and the third or subsequent operations ranges from 3 to 13 years [8-10].
As the BPOP is not possible to diagnose clinically and requires both radiological and histopathological expertise which shows some pathognomonic features such as cortico-medullary continuity and bizarre binucleated chondrocytes with cartilaginous cap. But in this case binucleated chondrocytes are present but the appearance appears to be more homogenous rather than bizarre. This can be both benign and malignant, but the presence of cartilaginous cap is suggestive of its benign character. BPOP often recurs after excision but till the last follow-up of 2 years, no growth is evident either clinically or radiologically.
BPOP is a rare tumor of small bones of hands and feet presenting with rapid growth and aggressive features on radiology. However, histopathological features of corticomedullary continuity and bizarre binucleated chondrocytes with cartilaginous cap are suggestive of benign nature. The contrasting features make it difficult to understand the nature of the tumor. Close follow-up should be done of all patients diagnosed with BPOP.
References
- 1.Saygi B, Karadag-Saygi E, Erzik C, Erkan M, Yildirim Y. Bizarre parosteal osteochondromatous proliferation of the little toe. J Am Podiatr Med Assoc 2006;96:158-61. [Google Scholar]
- 2.Doganavsargil B, Argin M, Sezak M, Kececi B, Pehlivanoglu B, Oztop F. A bizarre parosteal osteochondromatous proliferation (Nora’s lesion) of metatarsus, a histopathological and etiological puzzlement. Joint Bone Spine 2014;81:537-40. [Google Scholar]
- 3.Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol 1983;7:245-50. [Google Scholar]
- 4.Rybak LD, Abramovici L, Kenan S, Posner MA, Bonar F, Steiner GC. Cortico-medullary continuity in bizarre parosteal osteochondromatous proliferation mimicking osteochondroma on imaging. Skeletal Radiol 2007;36:829-34. [Google Scholar]
- 5.Dhondt E, Oudenhoven L, Khan S, Kroon HM, Hogendoorn PC, Nieborg A, et al. Nora’s lesion, a distinct radiological entity? Skeletal Radiol 2006;35:497-502. [Google Scholar]
- 6.Nilsson M, Domanski HA, Mertens F, Mandahl N. Molecular cytogenetic characterization of recurrent translocation breakpoints in bizarre parosteal osteochondromatous proliferation (Nora’s lesion). Hum Pathol 2004;35:1063-9. [Google Scholar]
- 7.Edoardo I, Elisa F, Damiano RA, Silvia F, Rodolfo C, Lorenzo A. Bizarre parosteal osteochondromatous proliferation (Nora Lesion): A narrative review. Acta Med Litu 2022;29:176-93. [Google Scholar]
- 8.Campanacci M. Bone and Soft Tissue Tumors. New York: Springer Verlag; 1990. p. 305. [Google Scholar]
- 9.Meneses MF, Unni KK, Swee RG. Bizarre parosteal osteochondromatous proliferation of the bone (B.P.O.P.). Am J Surg Pathol 1993;17:691-7. [Google Scholar]
- 10.de Lange EE, Pope TL Jr., Fechner RE, Keats TE. Case report 428: Bizarre parosteal osteochondromatous proliferation (BPOP). Skeletal Radiol 1987;16:481-3. [Google Scholar]












