Recognizing a unique peri-implant fracture pattern associated with an orthopedic implant with a successful treatment option avoiding the need for conversion to hemiarthroplasty.
Dr. Roy Small, Department of Orthopedic Surgery, Michigan State University, McLaren Macomb Medical Center, Mount Clemens, Michigan, USA. E-mail: roy.small@mclaren.org
Introduction: Peri-implant fractures (PIF) reported after cannulated screw and dynamic hip screw fixation historically occur distal to the implant within the subtrochanteric region secondary to the development of a stress riser. Newer implant designs for femoral neck fractures have attempted to combine the benefits of minimally invasive techniques without forgoing rigid angular stability but bring new potential complications.
Case Report: We present a case of an intertrochanteric PIF in the setting of a non-displaced femoral neck fracture treated with the DePuy Synthes Femoral Neck System (FNS).
Conclusion: We present this case of a unique PIF pattern with the hope of identifying a potential complication associated with the novel FNS. Furthermore, we present a successful treatment option avoiding the need for conversion to hemiarthroplasty.
Keywords: Femoral neck fracture, intertrochanteric fracture, femoral neck system, peri-implant fracture.
Newer implant designs for femoral neck fractures have attempted to combine the benefits of minimally invasive cannulated screw fixation with the rigid angular stability seen with dynamic hip screws (DHS) [1]. The femoral neck system (FNS) (Fig. 1) is one such design (DePuy Synthes, West Chester, Pennsylvania, USA). Fixation of femoral neck fractures is associated with a higher incidence of complications than any other fracture [2]. Complications following the fixation of non-displaced femoral neck fractures include non-union, avascular necrosis, implant cutout, varus collapse, and subtrochanteric peri-implant fracture (PIF) [3]. Subtrochanteric PIFs associated with cannulated screw fixation and DHS constructs lead to additional reoperation risks, particularly in the immunocompromised and osteoporotic elderly patient [4]. In this article, we present a case of an intertrochanteric PIF in the setting of a non-displaced femoral neck fracture treated with the FNS. This case report is the first of its kind highlighting an unexpected fracture pattern associated with a novel implant system utilized in the treatment of femoral neck fracture.
An 82-year-old female presented with right hip/groin pain and an inability to ambulate after a ground-level fall from standing at home. Persistent pain on clinical examination prompted advanced imaging for suspicion of occult femoral neck fracture despite a negative radiographic workup utilizing plain radiographs (Fig. 2a) and a CT scan (Fig. 2b). An MRI was unable to be obtained secondary to the patient’s history of retained metal shrapnel. Therefore, a three-phase bone scan was obtained which demonstrated increased uptake in the subcapital femoral neck region (Fig. 3).
An MRI was unable to be obtained secondary to the patient’s history of retained metal shrapnel. Therefore, a three-phase bone scan was obtained which demonstrated increased uptake in the subcapital femoral neck region (Fig. 3). 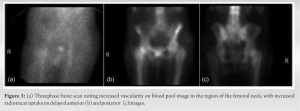 The patient underwent fracture fixation using the FNS 130-degree one-hole plate with an 85 mm barrel and a locking antirotation screw (Fig. 4). She tolerated surgery successfully without immediate post-operative complications. She was allowed to fully weight bear immediately after surgery. Her perioperative stay was otherwise uneventful, and she was discharged on post-operative day six to an inpatient rehabilitation center. Secondary to the fragility fracture, the patient was referred to her primary care physician for evaluation and management of osteoporosis. The patient was seen in the orthopedic trauma clinic at 2 weeks postoperatively for suture removal. At 8 weeks post-operative, the patient presented back to the emergency department following a second ground-level fall from standing at home.
The patient underwent fracture fixation using the FNS 130-degree one-hole plate with an 85 mm barrel and a locking antirotation screw (Fig. 4). She tolerated surgery successfully without immediate post-operative complications. She was allowed to fully weight bear immediately after surgery. Her perioperative stay was otherwise uneventful, and she was discharged on post-operative day six to an inpatient rehabilitation center. Secondary to the fragility fracture, the patient was referred to her primary care physician for evaluation and management of osteoporosis. The patient was seen in the orthopedic trauma clinic at 2 weeks postoperatively for suture removal. At 8 weeks post-operative, the patient presented back to the emergency department following a second ground-level fall from standing at home. 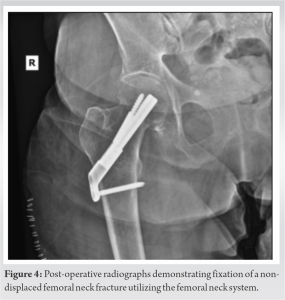 Radiographs and advanced imaging in the emergency department demonstrated a new four-part, peri-implant intertrochanteric fracture about the pre-existing FNS (Fig. 5 and 6). All instrumentation appeared intact without evidence of screw penetration, varus collapse, or other mode of construct failure outside of the PIF.
Radiographs and advanced imaging in the emergency department demonstrated a new four-part, peri-implant intertrochanteric fracture about the pre-existing FNS (Fig. 5 and 6). All instrumentation appeared intact without evidence of screw penetration, varus collapse, or other mode of construct failure outside of the PIF.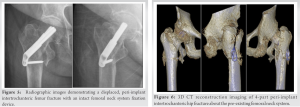 Recommendations were made to the patient and her family regarding the removal of the instrumentation with cephalomedullary nail fixation versus possible hip hemiarthroplasty. The patient elected to proceed with revision surgical fixation versus possible hemiarthroplasty and was medically optimized before returning to the operating room. Intraoperatively, the patient was positioned in the lateral decubitus position utilizing a peg board in anticipation of the possible need for hemiarthroplasty. The original incision was utilized and extended and routine dissection was performed splitting the vastus lateralis down to the level of the pre-existing FNS implant. The previous instrumentation showed no macroscopic evidence of fatigue or failure. The proximal antirotation screw and inner barrel were then easily backed out of position within the femoral neck without complication. The distal transverse screw through the one-hole plate was noted to be cold-welded to the implant, preventing simple removal with a hand screwdriver or a torque-limiting power driver. Multiple techniques for implant removal were attempted, including the use of a diamond-tipped burr and conical extraction screws. Both methods were unsuccessful at the time. Unable to free the distal screw, the side plate was then cut proximally in situ utilizing a metal-cutting diamond disc (Stryker, 2019).
Recommendations were made to the patient and her family regarding the removal of the instrumentation with cephalomedullary nail fixation versus possible hip hemiarthroplasty. The patient elected to proceed with revision surgical fixation versus possible hemiarthroplasty and was medically optimized before returning to the operating room. Intraoperatively, the patient was positioned in the lateral decubitus position utilizing a peg board in anticipation of the possible need for hemiarthroplasty. The original incision was utilized and extended and routine dissection was performed splitting the vastus lateralis down to the level of the pre-existing FNS implant. The previous instrumentation showed no macroscopic evidence of fatigue or failure. The proximal antirotation screw and inner barrel were then easily backed out of position within the femoral neck without complication. The distal transverse screw through the one-hole plate was noted to be cold-welded to the implant, preventing simple removal with a hand screwdriver or a torque-limiting power driver. Multiple techniques for implant removal were attempted, including the use of a diamond-tipped burr and conical extraction screws. Both methods were unsuccessful at the time. Unable to free the distal screw, the side plate was then cut proximally in situ utilizing a metal-cutting diamond disc (Stryker, 2019).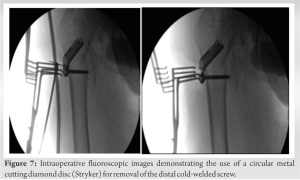 Then using a needle driver, the cold-welded screw and one-hole plate were successfully removed as a unit from the lateral cortex in a counterclockwise fashion (Fig. 7). At this point the fracture was adequately reduced with gentle traction and, secondary to adequate remaining bone stock, a decision was made to proceed with cephalomedullary nail fixation using the TFN-Advanced (TFNA) proximal femoral nailing system (DePuy Synthes, 2020). The previous FNS neck angle matched the 130° TFNA implant, so the same neck path was used with a fenestrated 85 mm lag screw through the nail. Injectable radiopaque cement was then directed through the lag screw, filling defects left from the previously placed antirotation screw (Fig. 8).
Then using a needle driver, the cold-welded screw and one-hole plate were successfully removed as a unit from the lateral cortex in a counterclockwise fashion (Fig. 7). At this point the fracture was adequately reduced with gentle traction and, secondary to adequate remaining bone stock, a decision was made to proceed with cephalomedullary nail fixation using the TFN-Advanced (TFNA) proximal femoral nailing system (DePuy Synthes, 2020). The previous FNS neck angle matched the 130° TFNA implant, so the same neck path was used with a fenestrated 85 mm lag screw through the nail. Injectable radiopaque cement was then directed through the lag screw, filling defects left from the previously placed antirotation screw (Fig. 8).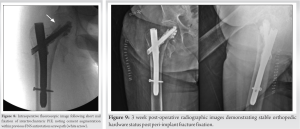 Postoperatively, the patient was restricted to toe-touch weight bearing and was mobilized daily with physical therapy. She was discharged on post-operative day 5 in stable condition to a sub-acute rehabilitation center. Her post-operative period was mostly uneventful minus a brief episode of acute kidney injury which was managed and resolved by nephrology. The patient was seen and evaluated in the orthopedic trauma clinic 3 weeks postoperatively. X-rays were obtained demonstrating stable positioning of the orthopedic implant (Fig. 9). She was allowed to fully weight bear after this visit. The patient had returned to her baseline as a household ambulator with an assistive device.
Postoperatively, the patient was restricted to toe-touch weight bearing and was mobilized daily with physical therapy. She was discharged on post-operative day 5 in stable condition to a sub-acute rehabilitation center. Her post-operative period was mostly uneventful minus a brief episode of acute kidney injury which was managed and resolved by nephrology. The patient was seen and evaluated in the orthopedic trauma clinic 3 weeks postoperatively. X-rays were obtained demonstrating stable positioning of the orthopedic implant (Fig. 9). She was allowed to fully weight bear after this visit. The patient had returned to her baseline as a household ambulator with an assistive device.
Non-displaced and valgus-impacted femoral neck fractures, classified as Garden I or II, are routinely treated with multiple cannulated screws or DHS constructs. Several studies have examined the complications associated with such fixation devices, estimating 3–13% complication rate of implant cut-out, varus collapse, and/or subtrochanteric PIF [5, 6]. PIFs reported with cannulated screw and DHS fixation historically occur distal to the implant within the subtrochanteric region. This is due to the increased stress secondary to the stiff implants used to obtain compression through the femoral neck. With axial loading coupled with abductor muscle distraction, the stiff construct creates a weak point concentrated in the subtrochanteric region, lending to the predictable PIF pattern [7]. Biomechanical evaluation of 2-hole and 4-hole DHS constructs placed under cyclic loading demonstrate similar PIF patterns, with failure occurring either just distal to the plate or at the level of the lag screw hole within the subtrochanteric region [8]. A tip-to-apex distance of <25 mm has been shown to increase the risk of screw cutout but has not been associated with a similar fracture pattern to our case [9]. The same subtrochanteric fracture pattern is also noted in studies evaluating PIFs in the setting of DHS and cephalomedullary implants used to treat intertrochanteric hip fractures [10]. These complications can be devastating, having shown severe complications in elderly osteopenic patients [4]. Rates of reoperation following fixation of stable femoral neck fractures, including conversion to arthroplasty or removal of the instrumentation with cephalomedullary nailing, range from 4 to 12% [11, 12]. Bhandari et al. identified a 21% overall reoperation rate when comparing DHS and cannulated screw fixation of non-displaced femoral neck fracture [13]. This complication profile drives the development of biomechanically superior implants. The FNS, developed by DePuy Synthes, was recently introduced in hopes to reduce such complications and reoperation rates through its reported stronger integrated rotational stability and minimally invasive compact design [5]. Moreso, the lateral locking plate of the FNS serves as a means of preventing lateral bolt prominence and subsequent abductor irritation commonly encountered with cannulated screw fixation and DHS devices. Several case studies and reports have demonstrated good outcomes utilizing the FNS for non-displaced, and even displaced femoral neck fractures in elderly and young patient populations alike [1]. However, to date, there are no reports of PIF in the setting of the novel FNS system. Based on previously published data, one would expect similar subtrochanteric fracture patterns associated with the FNS as seen with cannulated screws, DHS s, and cephalomedullary implants. We hypothesize the derotational screw divergence of the FNS may act as a stress riser within the intertrochanteric region leading to the fracture pattern discussed in this case report. Weaknesses of this article include those inherent to a single patient case report as well as a lack of literature surrounding complications of the FNS. Furthermore, we acknowledge the optimal treatment of minimally displaced femoral neck fractures is debated in the literature. Treatment with hemiarthroplasty has been shown to have lower reoperation rates as well as improved post-operative mobility [14, 15]. This case highlights an unexpected complication seen with the FNS: an intertrochanteric PIF in the setting of a previous non-displaced femoral neck fracture stabilized with the FNS. While our proposed treatment option appeared to be successful in the fixation of the PIF while avoiding conversion to hemiarthroplasty, long-term follow-up is not available at this time as the patient was lost to follow-up.
Newer implant designs such as the FNS combine the advantages of minimally invasive cannulated screw fixation with the higher mechanical stability seen with laterally fixated dynamic compression devices [1]. With higher stability and stiffness, concerns may arise with forces transferred to the surrounding bone. Subtrochanteric fractures encountered in cases of PIFs about cancellous screws and DHS constructs have been reported in the literature. To the best of our knowledge, this case is the first presented in the literature to report an intertrochanteric PIF associated with the newer FNS. A larger powered study is needed to form a proper correlation with our anecdotal findings, however, this report may be the first in potentially identifying unique PIF pattern association.
We present this case of a unique PIF pattern with the hope of identifying a potential complication associated with the novel FNS. Furthermore, we present a successful treatment option avoiding the need for conversion to hemiarthroplasty.
References
- 1.Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, et al. Biomechanical evaluation of the femoral neck system in unstable Pauwels III femoral neck fractures: A comparison with the dynamic hip screw and cannulated screws. J Orthop Trauma 2017;31:131-7. [Google Scholar]
- 2.Estrada LS, Volgas DA, Stannard JP, Alonso JE. Fixation failure in femoral neck fractures, clinical orthopaedics and related research. Clin Orthop Relat Res 2002;399:110-8. [Google Scholar]
- 3.Biz C, Tagliapietra J, Zonta F, Belluzzi E, Bragazzi NL, Ruggieri P. Predictors of early failure of the cannulated screw system in patients, 65 years and older, with non-displaced femoral neck fractures. Aging Clin Exp Res 2020;32:505-13. [Google Scholar]
- 4.Jansen H, Frey SP, Meffert RH. Subtrochanteric fracture: A rare but severe complication after screw fixation of femoral neck fractures in the elderly. Acta Orthop Belg 2010;76:778-84. [Google Scholar]
- 5.Matsumura T. FNS Case Study: Valgus Impacted Non-displaced Subcapital Femoral Neck Fracture in Elderly Patient. JnJ Medical Devices., Synthes USA Products, Monument, CO.; 2020. Available from: ??? [Last accessed on 2021 May 14]. [Google Scholar]
- 6.Zhang LL, Zhang Y, Ma X, Liu Y. Multiple cannulated screws vs. dynamic hip screws for femoral neck fractures: A meta-analysis. Orthopade 2017;46:954-62. [Google Scholar]
- 7.Tsai AG, Reich MS, Bensusan J, Ashworth T, Marcus RE, Akkus O. A fatigue loading model for investigation of iatrogenic subtrochanteric fractures of the femur. Clin Biomech (Bristol, Avon) 2013;28:981-7. [Google Scholar]
- 8.Rog D, Grigsby P, Hill Z, Pinette W, Inceoglu S, Zuckerman L. A biomechanical comparison of the two- and four-hole side-plate dynamic hip screw in an osteoporotic composite femur model. J Orthop Surg (Hong Kong) 2017;25:2309499017717199. [Google Scholar]
- 9.Rubio-Avila J, Madden K, Simunovic N, Bhandari M. Tip to apex distance in femoral intertrochanteric fractures: A systematic review. J Orthop Sci 2013;18:592-8. [Google Scholar]
- 10.Müller F, Galler M, Zellner M, Bäuml C, Marzouk A, Füchtmeier B. Peri-implant femoral fractures: The risk is more than three times higher within PFN compared with DHS. Injury 2016;47:2189-94. [Google Scholar]
- 11.Kain MS, Marcantonio AJ, Iorio R. Revision surgery occurs frequently after percutaneous fixation of stable femoral neck fractures in elderly patients. Clin Orthop Relat Res 2014;472:4010-4. [Google Scholar]
- 12.Bigoni M, Turati M, Leone G, Caminita AD, D’Angelo F, Munegato D, et al. Internal fixation of intracapsular femoral neck fractures in elderly patients: Mortality and reoperation rate. Aging Clin Exp Res 2019;32:1173-8. [Google Scholar]
- 13.Bhandari M, Devereaux PJ, Guyatt G, Thabane L, Walter SD, Heetveld MJ, et al. Fracture fixation in the operative management of hip fractures (FAITH): An international, multicentre, randomised controlled trial. Lancet 2017;389:1519-27. [Google Scholar]
- 14.Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, et al. Screw fixation versus hemiarthroplasty for nondisplaced femoral neck fractures in elderly patients: A multicenter randomized controlled trial. J Bone Joint Surg Am 2019;101:136-44. [Google Scholar]
- 15.Ma HH, Chou TA, Tsai SW, Chen CF, Wu PK, Chen WM. Outcomes of internal fixation versus hemiarthroplasty for elderly patients with an undisplaced femoral neck fracture: A systematic review and meta-analysis. J Orthop Surg Res 2019;14:320. [Google Scholar]











