Spontaneous resolution of an ankle deformity is possible after a physeal bar resection.
Dr. Neil Jain, Department of Orthopedic Surgery, Texas Tech University Health Sciences Center, Lubbock, Texas. E-mail: Neil.Jain@ttuhsc.edu
Introduction: Distal tibia fractures are a common cause of physeal injuries that can subsequently cause deformity in pediatric populations. Limited literature exists supporting treatment strategies for varus deformities. In this study, we illustrate a unique case of premature physeal closure complicated by development of a varus ankle deformity treated with navigation guided physeal bar resection that spontaneously resolved without the requirement for guided growth.
Case Report: A 6-year-old female presented to our clinic after development of a right ankle varus deformity measuring 14°. She had sustained a right Salter Harris type 3 distal tibia fracture 10 months prior and underwent fixation at an external facility. After undergoing navigation guided physeal bar resection, resolution of her deformity occurred without the use of guided growth.
Conclusion: Spontaneous resolution of an ankle deformity is possible after a physeal bar resection. However, in these technically demanding procedures, it is important to optimize accuracy and results using preoperative bar mapping and intraoperative three-dimensional navigation.
Keywords: Varus ankle, spontaneous resolution, bar resection, guided growth, case report.
Fractures in skeletally immature individuals involve the physis approximately 18–30% of the time [1, 2]. Physeal injuries are typically seen in children aged 11–14 years old and predominantly occur in males [1]. Due to their weak cartilaginous makeup, growth plates are highly susceptible to shearing and tensile forces [1]. Thus physeal injury in this population can lead to premature physeal closure (PPC) [3]. Common etiologies of PPC include physeal fractures, infection, congenital conditions (e.g. Blount’s disease), neoplasms, metabolic/hematologic disorders, frostbite, electrical injury, radiation exposure, and repetitive stress injuries [1, 3, 4]. Damage to this area can cause replacement with bony or fibrous tissue to form a bar that extends from the metaphysis to the epiphysis [1]. Removal of this unwanted bony bar is important as it can cause further complications such as angular deformities or growth arrest [1]. Current consensus for the indications of a physeal bar resection include: a documented history of existing or developing deformity, at least 2 years or 2 cm of growth remaining in the affected physis, and arrest affecting less than 50% of the growth plate; 50% being arbitrary [2, 3, 4, 5]. However, arrest greater than 25% of the physis has been associated with a decreased chance for growth resumption [3]. Many surgical techniques have been described in the literature for physeal bar resection, including the use of fluoroscopy, arthroscopy, or computer navigation for guidance [2, 3, 6]. Following excision of the bony bar, it has become standard to fill the cavity made with an interpositional material to prevent physeal bridge reformation and reduce scar formation [4, 7, 8, 9]. Options for grafted materials include fat, bone wax, or even cement [4]. After bar resection, it has been found that performing guided growth – also known as hemiepiphysiodesis – to correct angular deformities for these skeletally immature populations is more effective than bar excision alone [2]. Tension band plating (TBP) has gained traction as a favorable treatment option for guided growth as first described by Stevens et al. in 2007 [3, 10, 11]. Other management strategies for premature growth arrest include chondrodiastasis, limb lengthening and deformity correction, or a combination of the aforementioned techniques [4]. Third only to injuries of the distal radius and phalanges, distal tibia fractures are a common cause of physeal injuries that can subsequently cause deformity in pediatric populations [4, 9, 12]. Currently, limited literature exists supporting treatment strategies for varus deformities [10]. In this study, we illustrate a unique case of PPC complicated by development of a varus ankle deformity treated with navigation guided physeal bar resection that spontaneously resolved without the requirement for guided growth.
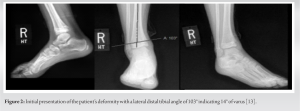
A 6-year-old girl with no relevant past medical history presented to our clinic after development of a right ankle varus deformity. She had sustained a right Salter Harris type 3 distal tibia fracture 10 months prior while jumping on a trampoline and underwent closed reduction percutaneous pinning at an external facility 3 weeks after the initial injury (Fig. 1).
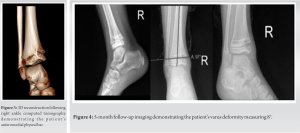
To better characterize the physeal bar, the patient followed up at a second visit 2 weeks later having obtained a computed tomography (CT) scan with 3D reconstruction. The physeal bar was measured at approximately 5 mm, involved less than 25% of the surface area of the physis, and localized to the anteromedial aspect of the right ankle (Fig. 3). Through shared decision-making, informed consent was obtained for distal tibia physeal bar resection with bone wax interposition, and the choice for lateral hemiepiphysiodesis was deferred unless indicated by insufficient resumption of growth or angular correction.
An anteromedial approach to the ankle was utilized and the physeal bar was localized on fluoroscopy with a Kirschner wire (K-wire). The K-wire was overdrilled with a drill bit size of 5 mm to a depth of 6 mm as determined by her preoperative CT imaging. A curette was used to further clear the borders of the physeal bar until normal appearing cartilage was visualized at the margins. There appeared to be some residual bone within the depth of the wound, and O-arm navigation was used intraoperatively to revise and verify that no remaining bone was crossing the physis. The bony edges were then covered with bone wax. Postoperatively, the patient was immobilized in a CAM boot and restricted in her daily activities.
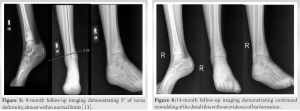
She was immobilized for 6 weeks before advancing to a normal shoe and resuming activities. At a 5-month follow-up, imaging revealed no obvious bar recurrence and a varus deformity of 8°, indicating a slight correction compared to preoperative films (Fig. 4). At a 9-month follow-up visit, approximately 21 months from the initial fracture, the patient’s gross alignment appeared near symmetric with symmetric ankle dorsiflexion and plantarflexion to 20° and 30° respectively. The patient had returned to gymnastics and normal activities without pain or soreness. Radiographic imaging from this visit showed nearly completely corrected varus deformity (Fig. 5). At a 14-month follow-up, imaging demonstrated continued remodeling of the distal tibia without evidence of bar formation (Fig. 6).
This patient demonstrated a Salter Harris type 3 right distal tibia fracture after jumping on a trampoline, a common mechanism for these types of injuries [12]. Interestingly, the patient’s varus deformity that resulted after fixation is uncommon, usually occurring in 2–25% of distal tibia cases, as noted by Blumetti et al. and Masquijo et al. [10, 12]. A good body of evidence has shown that ankle valgus deformities have been successfully treated with guided growth and TBP; however, limited literature exists supporting treatment strategies for varus deformities [10]. In 2019, Fu et al. demonstrated that bar resection with TBP was an effective treatment for these particular deformities with no difference in using fluoroscopy or intraoperative three-dimensional navigation [8]. In their study, they reported 31 out of 45 cases of effective treatment with median angle correction ranging from 10° to 15° [8, 10]. In our report, we were able to achieve these findings via a correction from 14° to 5° using only bar resection without TBP. Fu et al. further noted that it is critical to visualize the exact location of the physeal bar prior to resection either using plain radiography, CT, or magnetic resonance imaging [8]. However, they recommended intraoperative three dimensional navigation, similar to what was used in our presented case, to perform precise excision and allow for more accurate surgery [8]. Given the results of this report, we agree with their recommendation and support steps to ensure more accuracy in this already technically demanding procedure. Further literature on treatment of varus deformities can be found in the work done by Tunçez and Kazımoğlu and Blumetti et al. [9, 12]. Tunçez and Kazımoğlu effectively treated an 11-year-old patient with 30° of varus deformity using distal tibial opening wedge and fibular osteotomies, bar resection, and fat interposition techniques [9]. In the report done by Blumetti et al., initial bar resection in a 9-year-old patient with 18° of varus deformity failed, and satisfactory alignment was achieved only after distal tibial opening wedge and fibular osteotomies [12]. In either case, these treatments align with prior recommendations made by Williamson and Staheli for corrective osteotomy to be done at the time of bar resection for any deformity over 10° [5, 14]. In our report, we were able to avoid these invasive techniques and demonstrate that spontaneous resolution using only a bar resection is possible. However, it is important not to overlook that our early successful results were achieved in a young patient with a decent amount of remaining growth in comparison to previously cited cohorts. Continued long-term follow-up for these successful cases is crucial to assess for bar recurrence, PPC, or other discrepancies.
Spontaneous resolution of ankle deformity is possible after a physeal bar resection. However, in these technically demanding procedures, it is important to optimize accuracy and results using preoperative bar mapping and intraoperative three-dimensional navigation.
Spontaneous resolution of ankle deformity can be observed after a physeal bar resection; however, factors such as remaining growth can influence results. Continued long-term follow-up for these successful cases is crucial to assess for bar recurrence, PPC, or other discrepancies.
References
- 1.Yamamura MK, Carry PM, Gibly RF, Holmes K, Ogilvie B, Phillips A, et al. Epidemiology of physeal fractures and clinically significant growth disturbances affecting the distal tibia, proximal tibia, and distal femur: A Retrospective cohort study. J Am Acad Orthop Surg 2023;31:e507-15. [Google Scholar]
- 2.Xiao H, Li M, Zhu G, Tan Q, Ye W, Wu J, et al. The effectiveness of physeal bar resection with or without Hemi-Epiphysiodesis to treat partial growth arrest. BMC Musculoskelet Disord 2023;24:77. [Google Scholar]
- 3.Masquijo JJ, Allende V, Ferreyra A, Hernández Bueno JC. Distal femoral physeal bar resection combined with guided growth for the treatment of angular limb deformity associated with growth arrest: A preliminary report. J Pediatr Orthop 2020;40:e958-62. [Google Scholar]
- 4.Dabash S, Prabhakar G, Potter E, Thabet AM, Abdelgawad A, Heinrich S. Management of growth arrest: Current practice and future directions. J Clin Orthop Trauma 2018;9:S58-66. [Google Scholar]
- 5.Lalonde KA, Letts M. Traumatic growth arrest of the distal tibia: A clinical and radiographic review. Can J Surg 2005;48:143-7. [Google Scholar]
- 6.Kang HG, Yoon SJ, Kim JR. Resection of a physeal bar under computer-assisted guidance. J Bone Joint Surg Br 2010;92:1452-5. [Google Scholar]
- 7.Foster BK, John B, Hasler C. Free fat interpositional graft in acute physeal injuries: The anticipatory Langenskiöld procedure. J Pediatr Orthop 2000;20:282-5. [Google Scholar]
- 8.Fu G, Wang W, Dong YF, Lv XM, Yang Z. Treatment of post-traumatic pediatric ankle varus deformity with physeal bar resection and hemi-epiphysiodesis. Curr Med Sci 2019;39:604-8. [Google Scholar]
- 9.Tunçez M, Kazımoğlu C. Treatment of ankle varus deformity due to physeal bar formation: A case report. Ulus Travma Acil Cerrahi Derg 2022;28:1359-62. [Google Scholar]
- 10.Masquijo JJ, Artigas C, de Pablos J. Growth modulation with tension-band plates for the correction of paediatric lower limb angular deformity: Current concepts and indications for a rational use. EFORT Open Rev 2021;6:658-68. [Google Scholar]
- 11.Stevens PM. Guided growth for angular correction: A preliminary series using a tension band plate. J Pediatr Orthop 2007;27:253-9. [Google Scholar]
- 12.Blumetti FC, Gauthier L, Moroz PJ. The “trampoline ankle”: Severe medial malleolar physeal injuries in children and adolescents secondary to multioccupant use of trampolines. J Pediatr Orthop B 2016;25:133-7. [Google Scholar]
- 13.Çakmak M, Cıvan M. Ankle deformities. In: Şen C, Eralp L, Balci HI, Civan M, editors. Basic Techniques for Extremity Reconstruction: External Fixator Applications According to Ilizarov Principles. Berlin, Cham: Springer International Publishing; 2018. p. 413-39. [Google Scholar]
- 14.Williamson RV, Staheli LT. Partial physeal growth arrest: Treatment by bridge resection and fat interposition. J Pediatr Orthop 1990;10:769-76. [Google Scholar]