The triangular osteosynthesis construct is a stable and safe option for spinopelvic fixation and provides an anchor to early weight-bearing.
Dr. Mohit Kumar Verma, Department of Orthopaedic Surgery, Apex Trauma Centre, Sanjay Gandhi Postgraduate Institute, Lucknow, Uttar Pradesh, India. E-mail: mohitmamc120.2013@gmail.com
Introduction: Sacral fractures, which can occur in young individuals following road traffic accidents or falls from a height, as well as in elderly individuals with osteoporosis after minor trauma, are considered a diverse type of fracture. The incidence of non-osteoporotic sacral fractures is estimated to be 2.1/100,000 people, whereas osteoporotic fractures are estimated to affect 1–5% of elderly individuals at risk. Triangular osteosynthesis is a relatively new fixation technique used as a surgical treatment for unstable sacral fractures. It combines transverse fixation with lumbo-pelvis distraction osteosynthesis, providing stability in different planes. The subcategory of triangular osteosynthesis encompasses spinopelvic fixation, which involves the fusion of transverse sacral alar fracture fixation (such as iliosacral screw/s and sacral plate) and unilateral lumbopelvic fixation from the pedicle of L5 to the ipsilateral posterior ilium. The utilization of this technique provides a mechanically advanced approach for stabilizing unstable sacral alar fractures with vertical shear. Once the pelvic ring injury has been reduced, lumbopelvic fixation can assist in preventing the recurrence of vertical displacement in the unstable hemipelvis.
Case Report: The patient, a 29-year-old male, experienced a road traffic accident resulting from a collision involving a motorcycle. As a result of the incident, he suffered from an unstable lateral compression type 1 pelvic ring injury, accompanied by an ipsilateral sacroiliac dislocation and a vertical sacral fracture on the opposite side. Computed tomography imaging revealed a right sacroiliac dissociation, a left sacral fracture classified as AO type B1, as well as fractures in both the superior and inferior pubic rami. The pelvic ring of the patient was subjected to closed reduction and percutaneous fixation, accompanied by minimally invasive spinopelvic fixation. The surgical procedure was performed in a single session, involving the reduction and fixation of the right sacroiliac dissociation, followed by lumbopelvic fixation while in the prone position. After a 1-month follow-up, the patient demonstrated the ability to walk without experiencing pain, and the X-ray revealed a stable spinopelvic and sacroiliac fixation.
Conclusion: The utilization of triangular osteosynthesis fixation provides a reliable form of fixation that enables the patient to bear complete weight at an early stage of 6 weeks while also preventing any reduction loss in vertical shear transforaminal sacral fractures.
Keywords: Sacrum fracture, spinopelvic fixation, triangular osteosynthesis, iliosacral fixation.
Unstable sacral fractures are commonly observed in individuals who have undergone pelvic trauma, particularly those who have experienced high-energy trauma and are prevalent in a significant proportion (17–30%) of cases [1]. Non-osteoporotic sacral fractures have been reported to have an estimated incidence rate of 2.1/100,000 individuals, whereas osteoporotic fractures are estimated to occur in 1–5% of elderly individuals who are at risk [2]. Different modalities of internal fixation have been used in the past to reconstruct the pelvic ring including transiliac bars [3], sacral rods, and iliosacral screws inserted percutaneously. However, none of the above modalities were found to resist vertical shear force and provide early weight-bearing [4]. Spinopelvic fixation includes the subcategory of triangular osteosynthesis. The surgical approach involves the utilization of transverse sacral alar fracture fixation techniques such as iliosacral screws and sacral plates, among others, in combination with lumbopelvic fixation, usually unilateral, extending from the pedicle of L5 to the ipsilateral posterior ilium [5]. For unstable, vertical shear sacral alar fractures, this approach provides mechanically superior fixation. Triangular osteosynthesis is a relatively new fixation technique used as a surgical treatment for unstable sacral fractures. Triangular fixation provides transverse fixation with lumbopelvis distraction osteosynthesis providing stability in different planes. This technique offers numerous advantages in comparison to alternative treatment options. These include the facilitation of function recovery, the provision of rigid fixation, decompression of nerves, and early full weight-bearing ability [6]. Despite its benefits, there is still much debate about the technique and implant options for triangular osteosynthesis. Crushed nerve injuries have shown potential for restoration through early surgical intervention, exemplified by nerve decompression and early surgical measures employed in triangular osteosynthesis fixation for sacral fractures accompanied by nerve injuries. Triangular osteosynthesis has been established as a dependable method of stabilization for comminated vertical shear transforaminal sacral fractures [6].
A 29-year-old man sustained an unstable lateral compression type 1 pelvic ring injury, an ipsilateral sacroiliac dislocation, and an opposite vertical sacral fracture (Fig. 1) in a road traffic accident involving a motorcycle. There were no neurological deficits. Radiographs and computed tomography imaging were done, which revealed that the patient had right sacroiliac dissociation with left sacral fracture AO type B1, as well as bilateral superior and inferior pubic rami fractures (Fig. 2), resulting in spinopelvic instability. Upon arrival at the hospital, the patient was hemodynamically unstable and required immediate stabilization in the intensive care unit (ICU). Unfortunately, the patient developed a nosocomial MRSA infection during his stay in the ICU, which further complicated his recovery. After 22 days of injury, the patient underwent a comprehensive treatment approach that included closed reduction and percutaneous fixation of the pelvic ring, as well as minimally invasive spinopelvic fixation in a single setting. With the patient in the prone position, the first reduction and fixation of the right sacroiliac dissociation were followed by lumbopelvic fixation of the left side which involved the insertion of L5 pedicle screw and an iliac screw.
Radiographs and computed tomography imaging were done, which revealed that the patient had right sacroiliac dissociation with left sacral fracture AO type B1, as well as bilateral superior and inferior pubic rami fractures (Fig. 2), resulting in spinopelvic instability. Upon arrival at the hospital, the patient was hemodynamically unstable and required immediate stabilization in the intensive care unit (ICU). Unfortunately, the patient developed a nosocomial MRSA infection during his stay in the ICU, which further complicated his recovery. After 22 days of injury, the patient underwent a comprehensive treatment approach that included closed reduction and percutaneous fixation of the pelvic ring, as well as minimally invasive spinopelvic fixation in a single setting. With the patient in the prone position, the first reduction and fixation of the right sacroiliac dissociation were followed by lumbopelvic fixation of the left side which involved the insertion of L5 pedicle screw and an iliac screw.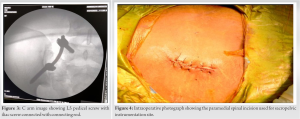
The patient was positioned in a prone manner on the imaging table, with the pelvis and chest adequately supported by silicone pads. Subsequently, right sacroiliac fixation was done using percutaneous cannulated cancellous (CC) screws. The fluoroscopic machine was set up in a lateral position, and traction was applied to the lower limb. A free guide wire was superimposed upon the iliac cortical density and anterior sacral slope, which were marked on the skin. The superior border of S1, along with the posterior sacral slope, was marked, and subsequently, a guide wire was carefully inserted within the zone of safety to facilitate the appropriate positioning of the screw. The operation proceeded in the standard fashion using inlet, outlet, and lateral radiographs, and an 80 mm CC screw was inserted over the guide wire.
A 4-cm paramedial incision was made over the lumbosacral region between L5 and S1 on the left side. Using the fluoroscopic technique, the lateral borders of the pedicle of L5 vertebrae were marked. The thoracolumbar fascia was dissected carefully, and the pedicle was exposed. Using an awl, entry was made through the lateral border of the pedicle, and a track within the pedicle was created by probing with a Lenke-style freehand probe. A 6.5 mm ×40 pedicle screw was placed after tapping the track. The fluoroscope is positioned on the left side of the iliac crest, with an angulation in the sagittal and coronal planes in the obturator outlet view. This ensures that the X-ray beams are aligned parallel to both the inner and outer tables of the ilium. Next, an incision of 1.5 cm is made over the posterior superior iliac spine (PSIS). The iliac screw direction was guided by the teardrop which is formed by the cortical layer of the iliac bone. The accurate placement of the screw in the middle of the teardrop was done. The burr channel was meticulously established toward the medial aspect of the PSIS using a bone awl, followed by a thorough evaluation using a probe. For the screw head to enter the burr hole, the medial PSIS was opened using a chisel. An 8.5 × 80 mm screw was put in. To find the ideal screw length and diameter, we employed intraoperative probing as well as pre-operative imaging (Fig. 3). The rod was bent accordingly in two planes to accommodate the more dorsal and lateral positions of the iliac screw compared to the pedicle screws. It was then passed through the screw heads from distal to proximal and firmly secured using set screws. Radiographs were employed to verify the alignment in the anteroposterior, lateral, and teardrop perspectives. Early mobilization with weight-bearing was implemented. Fig. 4 illustrates the paramedial incision on the left side utilized for spino-pelvis instrumentation. During the 1-month follow-up, the patient successfully walked without experiencing any discomfort, and the X-ray exhibited a secure spinopelvic and sacroiliac fixation (Fig. 5).
Schildhauer et al. [7] investigated cadaveric specimens with unilateral unstable sacral fractures under cyclic loading, and it was found that triangular osteosynthesis provided greater stability than a single iliosacral fixation. Combining horizontal (iliosacral) and vertical (lumbopelvic) fixation, triangle osteosynthesis provides extra protection against cranial migration of the fractured part of the pelvic ring by transferring vertical forces from the lower lumbar spine to the ilium [7]. With at least three distal pelvic fixation locations in our triangle osteosynthesis system, patients can begin bearing weight early. Because of this, the sacral fracture is only partially exposed to these loads, and by resisting the force of internal rotation, the horizontal component of the triangle fixation can more effectively stabilize the fracture in the horizontal plane. An additional benefit is that, unlike an iliosacral screw, which penetrates three cortices but predominantly trabecular bone at the bone-implant interface, the long ilium screw, which is positioned between the outer and inner iliac tables, has a greater degree of bicortical purchase. Because of their cortical purchase within the pedicle, the pedicle screw and other lumbopelvic fixation screws have a higher ratio of screw-bone interface and greater pull-out strength. El Dafrawy et al. [8] reported percutaneous S2 alar-iliac and iliosacral screw fixation to be a safe fixation technique that circumvents the soft-tissue compromise associated with open procedures in cases of unstable H-type sacral fractures. Sufficient pelvic anchor points in the triangle osteosynthesis construct enable quick weight-bearing operations. Gryphon et al. [9] have shown that addressing vertically unstable sacral fractures with percutaneous iliosacral screw fixation may be a helpful strategy. However, there are important anatomical restrictions, and extended bed rest is frequently needed to prevent fixation failure. Due to the patient’s young age, we opted not to fuse the lumbosacral junction to preserve motion across the L5-S1 joint. Mouhsine et al. [10] conducted a study on seven individuals with unstable sacral fractures, revealing that the fixation was stable enough to allow for immediate weight-bearing. Nevertheless, the researchers noted a concern regarding the visibility of the distal screw head. This problem was addressed using a bone chisel to remove the bone and sink the screw head. To maintain mobility across the L5-S1 joint, we chose not to fuse the lumbosacral junction due to the patient’s young age. This alternative method of treatment permits strong spinopelvic fixation, enabling the patient to bear weight soon after surgery and necessitating minimal soft-tissue dissection in the affected area. The current study provides a preliminary understanding of the potential benefits of triangular osteosynthesis in the treatment of fractures. However, to confirm the validity of these findings, further research involving larger case series and long-term investigations is necessary. This will help establish the effectiveness of triangular osteosynthesis in a wider range of patients and fracture types. In addition, future studies should also investigate the potential risks and complications associated with triangular osteosynthesis. This will help to ensure that the benefits of this technique outweigh any potential risks or adverse effects. Despite the need for further research, the current study offers valuable insights into clinical practice. This information can be used by clinicians to make informed decisions about the most appropriate treatment options for their patients.
The stable fixation technique of triangular osteosynthesis allows for early weight-bearing in patients with transforaminal sacral fractures while still maintaining proper reduction in vertical shear. In this particular case, the patient’s young age played a significant role in the decision-making process. Given their young age, it was important to prioritize maintaining mobility in the L5-S1 joint. Therefore, the decision was made against fusing the lumbosacral junction, as fusion would restrict movement in this joint. By opting for a non-fusion approach, the patient’s mobility in the L5-S1 joint is preserved. This allows for a greater range of motion and flexibility in the lower back, which can be particularly beneficial for a young individual. In addition, this approach facilitates strong spinopelvic fixation, meaning that the stability of the spine and pelvis is maintained.
Vertical shear fractures of the sacrum are highly unstable fractures and typically require a stable type of fixation. The combination of vertical (lumbopelvic) and horizontal (iliosacral) fixation, known as triangle osteosynthesis, ensures stability in multiple planes. This technique effectively transfers vertical stresses from the lower lumbar spine to the ilium, allowing for early weight-bearing.
References
- 1.Gibbons KJ, Soloniuk DS, Razack N. Neurological injury and patterns of sacral fractures. J Neurosurg 1990;72:889-93. [Google Scholar]
- 2.Santolini E, Kanakaris NK, Giannoudis PV. Sacral fractures: Issues, challenges, solutions. EFORT Open Rev 2020;5:299-311. [Google Scholar]
- 3.Ebraheim NA, Coombs R, Hoeflinger MJ, Zeman C, Jackson WT. Anatomical and radiological considerations in compressive bar technique for posterior pelvic disruptions. J Orthop Trauma 1991;5:434-8. [Google Scholar]
- 4.Kanezaki S, Miyazaki M, Notani N, Ishihara T, Sakamoto T, Sone T, et al. Minimally invasive triangular osteosynthesis for highly unstable sacral fractures: Technical notes and preliminary clinical outcomes. Medicine (Baltimore) 2019;98:e16004. [Google Scholar]
- 5.ORIF-Triangular Osteosynthesis for Sacral Fractures. Available from: https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/pelvic-ring/sacrum/orif-triangular-osteosynthesis [Last accessed on 2023 Jul 08]. [Google Scholar]
- 6.Hu X, Pei F, Wang G, He J, Kong Q, Tu C. Application triangular osteosynthesis for vertical unstable sacral fractures. Eur Spine J 2013;22:503-9. [Google Scholar]
- 7.Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt ML Jr. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: A cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma 2003;17:22-31. [Google Scholar]
- 8.El Dafrawy MH, Shafiq B, Vaswani R, Osgood GM, Hasenboehler EA, Kebaish KM. Minimally invasive fixation for spinopelvic dissociation: Percutaneous triangular osteosynthesis with S2 alar-iliac and iliosacral screws: A case report. JBJS Case Connect 2019;9:e0119. [Google Scholar]
- 9.Griffin DR, Starr AJ, Reinert CM, Jones AL, Whitlock S. Vertically unstable pelvic fractures fixed with percutaneous iliosacral screws: Does posterior injury pattern predict fixation failure? J Orthop Trauma 2006;20:S30-36, discussion S36. [Google Scholar]
- 10.Mouhsine E, Wettstein M, Schizas C, Borens O, Blanc CH, Leyvraz PF, et al. Modified triangular posterior osteosynthesis of unstable sacrum fracture. Eur Spine J 2006;15:857-63. [Google Scholar]








