The combined effect of factors such as bone fragility, posterior pelvic tilt, and high activity level likely caused bilateral subchondral insufficiency fractures, and we should be careful as we expect to see an increase in such cases in the future.
Dr. Nobuhiro Kaku, Department of Orthopedic Surgery, Faculty of Medicine, Oita University, Yufu, Oita, Japan. E-mail: nobuhiro@oita-u.ac.jp
Introduction: Unilateral subchondral insufficiency fractures (SIF) of the femoral head have been reported in many cases; however, bilateral cases occurring simultaneously are very rare.
Case Presentation: We report two cases of relatively active elderly females (aged 73 and 67 years), in which bilateral hip pain appeared simultaneously without any specific triggers. There were no notable lifestyle or medication histories. Imaging and histopathology of the bone excised surgically supported the diagnosis. In Case 1, there was a decrease in bone mineral density and poor congruency between the femoral head and acetabulum. In Case 2, the posterior tilt of the pelvis with aging decreased coverage of the femoral head, and the poor congruency between the femoral head and acetabulum was thought to have contributed to uneven distribution and increased stress in the loading zone.
Conclusion: We encountered two unusual cases with contemporaneous bilateral SIF in the elderly. In recent years, the number of highly active elderly people has increased with the increase in healthy life expectancy. The combined effect of factors such as bone fragility, posterior pelvic tilt, and high activity level likely caused bilateral SIFs, and we should be careful as we expect to see an increase in such cases in the future.
Keywords: Aged, femoral head, osteoporosis, subchondral insufficiency, fracture.
Subchondral insufficiency fracture (SIF) of the femoral head was first reported by Bangil et al. in 1996 [1]. This fracture must be differentiated from osteonecrosis of the femoral head, requiring significant patient background, and characteristic Magnetic resonance imaging (MRI) and histopathological findings. Simultaneous bilateral cases of SIF of the femoral head are extremely rare, although many unilateral cases have been reported. In the present study, we report two cases of bilateral SIF in elderly females with no special history.
Case 1
A 73-year-old female with 150.6 cm height, 46.1 kg weight, and 20.3 body mass index (BMI) presented to the clinic with simultaneous bilateral hip pain without any specific triggers. There was no notable lifestyle or medication history. The patient-led an independent life and walked approximately 2 km every morning. Blood biochemistry tests showed the following: Calcium (Ca), 8.10 mg/dL; inorganic phosphorus (IP), 2.48 mg/dL; tartrate-resistant acid phosphatase-5b (TRACP-5b), 346 mU/dL; and total type 1 amino-terminal propeptide (P1NP), 92.7 mg/mL. X-ray images showed that the right femoral head was crushed, while the left side showed no abnormal findings (Fig. 1).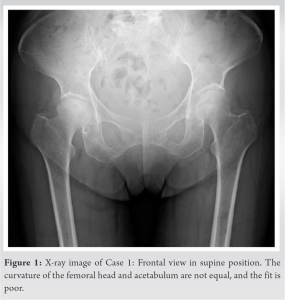
Case 2
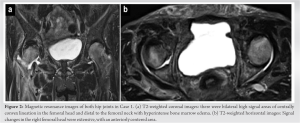
A 67-year-old female with 144.0 cm height, 54.2 kg weight, and 26.1 BMI lived an independent life and jogged 1 km 3 times a week. Without any specific trigger, she developed bilateral hip pain and presented to our department. Blood biochemistry tests showed the following: Ca, 9.48 mg/dL; IP, 3.70 mg/dL; TRACP-5b, 615 mU/dL; and total P1NP, 68.7 mg/mL. X-ray imaging showed a crushed right femoral head and a linear sclerotic image on the central side of the left femoral head (Fig. 4). X-ray images also showed a 34.6°/31.4° CE angle, 77/76% AHI, a 32.9°/43.4° Sharp angle, and 5.2°/17.7° ARO, which corresponds to an ARO of 24.2°/21.8° if we consider that the acetabular sourcil is not parallel to the round femoral head, and the loading surface is up to the top of the “mountain.” The conformity was equivalent to “Fair” according to the classification of Yasunaga et al. [2]. MRI showed a centrally convex linear signal area in the femoral head at T1 and T2 and a hyperintense area extending to the femoral neck at T2. The right femoral head showed extensive signal changes centered anteriorly and centrally, while the left femoral head showed signal changes anteriorly and centrally (Fig. 5).
This case report was approved by the Institutional Review Board of our university (Number 1414). Written and verbal informed consent was approved by the study participants.
SIFs of the femoral head must be differentiated from necrosis of the femoral head. In the case of necrosis, a history of alcohol abuse and a single dose of steroid medication are important. On imaging of a necrotic femoral head, there is a relatively wide band image and a broad, inferiorly convex necrotic zone, while on histopathology, there is a three-layered structure consisting of a necrotic zone with unstructured necrotic material, a repair zone infiltrated by granulation tissue, and a healthy zone with hyperplastic bone formation on the outer side [3]. On the other hand, MRI findings of SIFs of the femoral head are characterized by the presence of horizontal or upward convex thin linear hypointense areas, fractures of the bony trabeculae, and callus [4]. Both cases in this report showed the characteristic clinical course, imaging, and histopathological SIF findings. Bilateral SIF is extremely rare. Previous reports included five cases (Table 1), three of which were reported after kidney transplantation [5, 6], including a 32-year-old man with oncogenic osteochondrosis and a 14-year-old girl with acetabular dysplasia and Vitamin D deficiency [7, 8]. Ohtsuru et al. [5] reported two cases of 53 and 57-year-old men with two points in common: Renal transplantation in middle-aged men and involvement of multiple factors such as age, weight, degree of pelvic retroversion, bone density, and initial treatment. Ikemura et al. [6] also considered the possibility that the use of high-dose steroids and immunosuppressive drugs after renal transplantation in a 47-year-old man may have caused bone fragility that could not be detected by decreased bone density. We examined the common features of the bilateral cases reported thus far and found that the common feature among the three cases was that they were diagnosed after renal transplantation in middle age. Other common features include decreased bone mineral density or bone fragility that does not show up in bone mineral density, and younger age, rather than the older patients usually reported with unilateral SIF. In the two cases of elderly onset we reported, Case 1 had reduced bone density, while Case 2 had no loss of bone density. Both cases were relatively active for their advanced age. We found no similarities between these cases and previous reports. Pentecost et al. [9] defined an insufficiency fracture as that which occurs in a bone with less than normal elastic resistance due to stretching and compression. Although reports of bilateral insufficiency fractures are rare, there have been cases reported in other bones [10]. The mechanism of occurrence is not completely the same as that of SIF; however, both our cases were active and had bone fragility, which may have been a contributing factor to the bilateral onset. Iwasaki et al. [11] reported two mechanisms of pathogenesis, one that occurs based on insufficient acetabular coverage, including developmental dysplasia of the hip, and one unrelated to acetabular coverage. However, not limited to acetabular coverage, mechanical loading on the femoral head may involve soft-tissue elements such as the femoral head and acetabular incompatibility and inversion of the labrum of the hip joint [12, 13, 14]. In addition, poor joint congruency and inadequate coverage lead to increased and unevenly distributed stresses at the loading joint [15]. Increased localized stress at the loading surface for inadequate coverage and fit, coupled with factors such as bone fragility, may lead to fractures of the femoral head. In both present cases, fractures occurred anterior to the center of the loading area of the femoral head. Although the two cases did not have anatomic acetabular dysplasia, posterior torsion of the acetabulum, or femoral head-and-neck junction head elevation, there was a loss of bone density and poor fit between the femoral head and acetabulum in Case 1, and the pelvis was tilted backward in Case 2, which reduced the anterior coverage of the femoral head and resulted in an uneven and increased stress on the load area. The poor fit between the femoral head and acetabulum and the posterior tilt of the pelvis in Case 2 resulted in uneven and increased stress on the loading area, causing the femoral head to fracture anteriorly in the center.
We encountered two unusual cases with contemporaneous bilateral SIF in the elderly. In recent years, we have become an aging society, and the number of highly active elderly people has also increased with the increase in healthy life expectancy. The combined effect of factors such as bone fragility, posterior pelvic tilt, and high activity level likely caused bilateral SIF, and we should be careful as we expect to see an increase in such cases in the future.
Older patients with a high level of activity are more likely to develop bilateral SIF due to a combination of factors, including bone fragility and posterior pelvic tilt, and it is important to note that the number of such cases is expected to increase in the future.
References
- 1.Bangil M, Soubrier M, Dubost JJ, Rami S, Carcanagues Y, Ristori JM, et al. Subchondral insufficiency fracture of the femoral head. Rev Rhum Engl Ed 1996;63:859-61. [Google Scholar]
- 2.Yasunaga Y, Takahashi K, Ochi M, Ikuta Y, Hisatome T, Nakashiro J, et al. Rotational acetabular osteotomy in patients forty-six years of age or older: Comparison with younger patients. J Bone Joint Surg Am 2003;85:266-72. [Google Scholar]
- 3.Sugano N, Kubo T, Takaoka K, Ohzono K, Hotokebuchi T, Matsumoto T, et al. Diagnostic criteria for non-traumatic osteonecrosis of the femoral head. A multicentre study. J Bone Joint Surg Br 1999;81:590-5. [Google Scholar]
- 4.Yamamoto T, Schneider R, Bullough PG. Insufficiency subchondral fracture of the femoral head. Am J Surg Pathol 2000;24:464-8. [Google Scholar]
- 5.Ohtsuru T, Yamamoto T, Murata Y, Morita Y, Munakata Y, Kato Y. Bilateral subchondral insufficiency fractures of the femoral head in patients with living renal transplantation: A report of two cases. J Orthop Sci 2017;22:972-5. [Google Scholar]
- 6.Ikemura S, Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Iwamoto Y. Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: A case report. Arthritis Rheum 2005;52:1293-6. [Google Scholar]
- 7.Ishizu H, Shimizu T, Kaibara T, Asano T, Terkawi MA, Takahashi D, et al. Bilateral subchondral insufficiency fractures of the femoral head in a normally active adolescent patient: A case report. J Orthop Sci 2022;27:492-4. [Google Scholar]
- 8.Chouhan V, Agrawal K, Vinothkumar TK, Mathesul A. Bilateral insufficiency fracture of the femoral head and neck in a case of oncogenic osteomalacia. J Bone Joint Surg Br 2010;92:1028-31. [Google Scholar]
- 9.Pentecost RL, Murray RA, Brindley HH. Fatigue, insufficiency, and pathologic fractures. JAMA 1964;187:1001-4. [Google Scholar]
- 10.Moretti B, Speciale D, Garofalo R, Moretti L, Patella S, Patella V. Spontaneous bilateral fracture of patella. Geriatr Gerontol Int 2008;8:55-8. [Google Scholar]
- 11.Iwasaki K, Yamamoto T, Motomura G, Karasuyama K, Sonoda K, Kubo Y, et al. Common site of subchondral insufficiency fractures of the femoral head based on three-dimensional magnetic resonance imaging. Skeletal Radiol 2016;45:105-13. [Google Scholar]
- 12.Kubo Y, Motomura G, Utsunomiya T, Fujii M, Ikemura S, Sonoda K, et al. Distribution of femoral head subchondral fracture site relates to contact pressures, age, and acetabular structure. AJR Am J Roentgenol 2020;215:448-57. [Google Scholar]
- 13.Wang X, Fukui K, Kaneuji A, Hirosaki K, Miyakawa H, Kawahara N. Inversion of the acetabular labrum causes increased localized contact pressure on the femoral head: A biomechanical study. Int Orthop 2019;43:1329-36. [Google Scholar]
- 14.Jo WL, Lee WS, Chae DS, Yang IH, Lee KM, Koo KH. Decreased lumbar lordosis and deficient acetabular coverage are risk factors for subchondral insufficiency fracture. J Korean Med Sci 2016;31:1650-5. [Google Scholar]
- 15.Stone JJ, Yu H. Computational contact analysis of joint congruency. Biomed Sci Instrum 1997;34:368-73. [Google Scholar]











