The long-term results of total joint arthroplasty in ochronotic arthropathy are good. Robotic system helps in better soft tissue balancing and less soft tissue injury in already stiff and friable soft tissues.
Dr. Atul Jaspal, Department of Orthopaedics, Amandeep Hospital, Amritsar, Punjab, India. E-mail: atuljaspal@gmail.com
Introduction: Alkaptonuria is a rare autosomal recessive disorder caused by the defective metabolism of homogentisic acid, with a rare course and remained undetected even until adulthood. Ochronotic arthropathy is one of the manifestations of alkaptonuria, predominantly affecting weight bearing joints such as spine, hip, and knee. Total joint arthroplasty is treatment of choice in end-stage arthritis of hip and knee. Owing to the rarity of the disease, limited data is available in literature regarding surgical challenges and long-term functional outcomes.
Case Report: Herein, we present a case of 43-year-old male with ochronotic arthropathy of bilateral hip, right knee, and bilateral elbow joints with involvement of spine, who was incidentally diagnosed with ochronotic arthropathy intraoperatively and underwent sequential arthroplasty for right hip followed by right knee and left hip over a period of 10 years. At 11 years’ follow-up, the patient has full mobility with no loosening of implants.
Conclusion: The long-term results of total joint arthroplasty in ochronotic arthropathy are good. Surgeon should be aware of the difficulty in soft tissue balancing and possible complications in the ochronotic arthropathy and require a conscientious approach to avoid complications.
Keywords: Alkaptonuria, ochronosis, ochronotic arthropathy, total knee arthroplasty, total hip arthroplasty.
Alkaptonuria is a rare autosomal recessive metabolic disorder affecting 1 in 1 million people, first described by Sir Archibald Garrod in 1908. It is caused by mutation of homogentisic acid (HGA) oxidase (HGO) gene on chromosome 3q resulting in defective HGO [1]. This presents with classical clinical triad of homogentisic aciduria (black discoloration of the urine after standing when oxidized or alkalinized); eumelanin-like pigmentation of the skin, sclera, ear cartilages, and other organs; and degenerative ochronotic arthropathies commonly appearing in the fourth decade of life. Less common manifestations include renal, urethral, and prostate calculi, cutaneous nodules and deposition in cardiovascular system, especially the valves [2, 3]. Ochronotic arthropathy is caused due to alteration of the mechanical properties due to deposition of bluish black pigmented remnants of the metabolite in connective tissues (particularly in hyaline articular cartilage). This chemically irritates the joint leading to inflammation, brittle/fragile connective tissue, and degeneration of the joint [4]. It usually involves spine first followed by large joints such as hip and knee affecting the quality of life and may cause disability in young individuals [5, 6]. There is no specific and effective medical treatment for ochronotic arthropathy [7]. Total joint arthroplasty has been suggested as an effective treatment option for end-stage ochronotic arthropathy. However, with only few reported cases, there is a paucity of data available in medical literature regarding the bone quality for survivorship of total joint arthroplasty, intraoperative challenges, complications, and long-term functional outcomes. Herein, we present a case of a 43-year-old male with ochronotic arthropathy managed by staged bilateral total hip arthroplasty and robotic-assisted right total knee arthroplasty with a long-term follow-up of 10 years and a discussion regarding the challenges and surgical management in such patients.
A 43-year-old male presented to us with complaint of pain in right hip for the past 2 years and restriction of movement for the past 1 year. Pain was insidious in onset, used to relieve on taking medications initially and aggravates on walking. However, when patient presented to us, the pain was of such severity that it was interfering with his daily activities and it was not responding to any conservative treatment. On physical examination, the patient had antalgic gait, there was flexion deformity of 15°, adduction and abduction possible up to 15° and there was hardly any rotation in right hip. There was true shortening of about 1.5 cm of right limb compared to left. Examination of spine, contralateral hip, and both knee joints revealed no abnormality. On radiographs, there was concentric loss of joint space and subchondral sclerosis (Fig. 1). The patient was planned for right total hip replacement after routine pre-operative preparations. Positioned in lateral decubitus position, on exposing the hip joint using posterior approach, we noticed black pigmentation of subcutaneous tissues, joint capsule, bones, and articular surfaces. The consistency of joint capsule was not normal, and it was very hard and contracted. We faced difficulty in dislocating the hip joint due to stiff and contracted joint capsule. During acetabular reaming, we realized that the bone was osteopenic so reaming of acetabulum and femoral canal preparation were done gently. We also faced difficulty in reducing the joint due to contracted joint capsule so we had to excise some part of anterior hip joint capsule for reduction of components. Retrospectively patient gave history of darkening of urine and cloths on exposure to air and sunlight. On physical examination, the patient also had yellowish dark pigmentation of sclera and ear lobules (Fig. 2). His high urine HGA levels confirmed the diagnosis. There was no family history of ochronosis. ost-operative rehabilitation was smooth, the patient was mobilized with full weight bearing next day after surgery, drain removed 48 h after surgery, and the patient discharged on 4th day postoperatively.
The patient was planned for right total hip replacement after routine pre-operative preparations. Positioned in lateral decubitus position, on exposing the hip joint using posterior approach, we noticed black pigmentation of subcutaneous tissues, joint capsule, bones, and articular surfaces. The consistency of joint capsule was not normal, and it was very hard and contracted. We faced difficulty in dislocating the hip joint due to stiff and contracted joint capsule. During acetabular reaming, we realized that the bone was osteopenic so reaming of acetabulum and femoral canal preparation were done gently. We also faced difficulty in reducing the joint due to contracted joint capsule so we had to excise some part of anterior hip joint capsule for reduction of components. Retrospectively patient gave history of darkening of urine and cloths on exposure to air and sunlight. On physical examination, the patient also had yellowish dark pigmentation of sclera and ear lobules (Fig. 2). His high urine HGA levels confirmed the diagnosis. There was no family history of ochronosis. ost-operative rehabilitation was smooth, the patient was mobilized with full weight bearing next day after surgery, drain removed 48 h after surgery, and the patient discharged on 4th day postoperatively.
After 6 years, the patient developed pain and stiffness in right knee and lower back. He had right knee range of motion of around 10–90°, and medial and lateral joint line tenderness was present. Radiographic examination of spine revealed multilevel fused intervertebral disc spaces, syndesmophytes formation, and osteoporosis (Fig. 3) whereas loss of joint space and widespread osteophytes were seen on knee X-ray. The patient was advised conservative treatment for his back pain and robotic-assisted posterior stabilized total knee replacement was done on right knee. This time surgery underwent under general anesthesia as it was difficult to give spinal anesthesia to patient. Intraoperatively, we noted black subcutaneous nodules (Fig. 4), dark stiff menisci, and black pigmentation of articular surface of patella, femur, and tibia. There was difficulty in retracting the patella so we excised patellar osteophytes in initially steps of surgery to avoid tension on patellar tendon attachment at tibial tuberosity. As most of the soft tissue structures were stiff, robotic system allowed us better soft tissue balancing, precise bone cuts and appropriate implant planning. Robotic system also helped us in avoiding use of intramedullary jig as bones were osteopenic. Further steps of surgery completed without any complication. The patient was allowed full weight bearing next day after surgery and gained painless range of motion of 0–100° within 2 weeks.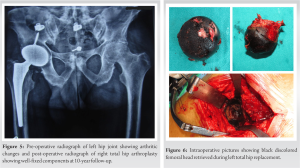
4 years after his right knee replacement, the patient developed painful arthritis of left hip (Fig. 5), for which uncemented total hip replacement was done. Similar findings suggestive of ochronosis were noted intraoperatively (Fig. 6). The patient also had stiffness of bilateral elbow with decreased range of motion. Radiographs of bilateral elbow revealed arthritic changes (Fig. 7), for which patient demanded only conservative treatment. At 11-year follow-up of right total hip replacement, 5-year follow-up of right total knee replacement and 1-year follow-up of left total hip replacement patient is doing well with well fixed all components, there are no radiolucent lines on X-rays, no osteolysis, and the patient has good range of motion in all the replaced joints (Fig. 8).

Alkaptonuria being a metabolic disorder affects connective tissues particularly cartilage and bone leading to fragile bone and degenerative arthritis. The wide spectrum of clinical variability may delay the diagnosis of alkaptonuria and usually an incidental finding of blackened joint during surgery is what leads to its suspicion [8]. History of dark color urine or black cola colored discoloration after prolonged standing is the only early manifestations seen during childhood. Other manifestations present only after the fourth decade of life when renal clearance of HGA decreases with aging. Ochronotic arthropathy occurs due to deposition of polymerized HGA in connective tissue and cartilage, chronic inflammation, and microruptures. It is usually seen after fourth decade affecting large weight bearing joints mainly knee, hip, and spine. Ochronotic arthropathy is usually managed conservatively as there is no definitive medical treatment available currently. Nitisinone, an inhibitor of 4-hydroxyphenylpyruvate dioxygenase, has been shown to decrease urinary excretion of HGA, however, its efficacy in ochronotic arthropathy is not proven yet [9]. Dietary restriction of ascorbic acid and amino acids particularly phenylalanine and tyrosine is advised. End-stage degenerative arthritis involving multiple large joints such as spine, knee, and hip is common in ochronotic arthropathy. Total joint arthroplasty in ochronotic arthropathy leads to significant improvement in functional outcome postoperatively. Ligaments and tendons are stiffened due to heavy pigment deposition with high collagen content, leading to inflammation, calcification, and are at risk for rupture. Previous reports describe increased risk of patellar and Achilles tendon rupture during surgery. Hence, we advise gentle handling and caution during retraction and dislocation of patella. The surgeon should be familiar to tackle such complications and ensure the availability of necessary implants/instruments in the inventory [10-12]. Furthermore, we also recommend the use of posterior stabilized prosthesis in knee arthroplasty because of suspected compromised state of ligaments. The post-operative rehabilitation is no different from a standard protocol for a patient undergoing arthroplasty except that the active quadriceps exercises should be done with caution due to stiff and friable tendon [13, 14]. Increased intraoperative and post-operative blood loss, delayed drain removal has been reported previously which was attributed to surgeon’s extensive synovectomy owing to inflammatory nature of the disease [9]. In our reported case report, blood loss was average and no transfusion of any blood products was needed after the surgery. Most of the previously published case reports describe short to midterm follow-up for total joint arthroplasty in ochronotic arthropathy, with only few reporting long-term follow-up. Moreover, to our knowledge, there is no case report till date describing clinical and functional outcomes after robotic total knee arthroplasty using full burr technique in ochronotic arthroplasty. Our case report describes the promising clinicoradiological outcomes after robotic-assisted total knee arthroplasty in patients with ochronotic arthropathy.
The diagnosis of alkaptonuria and ochronotic arthropathy is often delayed due to its unusual presentation and rarity of the disease. It requires a high index of suspicion preoperatively and often is an incidental diagnosis intraoperatively. Careful handling of soft tissue structures during surgery and post-operative rehabilitation is needed to prevent tendon or ligament injury.
Involvement of bilateral elbow joint, bilateral hip joint, spine, and knee joint in a single patient is rare in ochronotic arthropathy. Long-term results of total joint arthroplasty are good in ochronotic arthropathy. However, surgeon should be aware of possible complications in such patients.
References
- 1.Phornphutkul C, Introne WJ, Perry MB, Bernardini I, Murphey MD, Fitzpatrick DL, et al. Natural history of alkaptonuria. N Engl J Med 2002;347:2111-21. [Google Scholar]
- 2.Aliberti G, Pulignano I, Schiappoli A, Minisola S, Romagnoli E, Proietta M. Bone metabolism in ochronotic patients. J Intern Med 2003;254:296-300. [Google Scholar]
- 3.Wu K, Bauer E, Myung G, Fang MA. Musculoskeletal manifestations of alkaptonuria: A case report and literature review. Eur J Rheumatol 2018;6:98-101. [Google Scholar]
- 4.Taylor AM, Boyde A, Wilson PJ, Jarvis JC, Davidson JS, Hunt JA, et al. The role of calcified cartilage and subchondral bone in the initiation and progression of ochronotic arthropathy in alkaptonuria. Arthritis Rheum 2011;63:3887-96. [Google Scholar]
- 5.Mistry JB, Bukhari M, Taylor AM. Alkaptonuria. Rare Dis 2013;1:e27475. [Google Scholar]
- 6.Gil JA, Wawrzynski J, Waryasz GR. Orthopedic manifestations of ochronosis: Pathophysiology, presentation, diagnosis, and management. Am J Med 2016;129:536.e1-6. [Google Scholar]
- 7.Ranganath LR, Cox TF. Natural history of alkaptonuria revisited: Analyses based on scoring systems. J Inherit Metab Dis 2011;34:1141-51. [Google Scholar]
- 8.Fisher AA, Davis MW. Alkaptonuric ochronosis with aortic valve and joint replacements and femoral fracture: A case report and literature review. Clin Med Res 2004;2:209-15. [Google Scholar]
- 9.Patel VG. Total knee arthroplasty in ochronosis. Arthroplasty Today 2015;1:77-80. [Google Scholar]
- 10.Sahoo MM, Mahapatra SK, Sethi GC, Dash SK. Patellar ligament rupture during total knee arthroplasty in an ochronotic patient. Acta Orthop Traumatol Turc 2014;48:367-70. [Google Scholar]
- 11.Spencer JM, Gibbons CL, Sharp RJ, Carr AJ, Athanasou NA. Arthroplasty for ochronotic arthritis: No failure of 11 replacements in 3 patients followed 6-12 years. Acta Orthop Scand 2004;75:355-8. [Google Scholar]
- 12.Manoj Kumar RV, Rajasekaran S. Spontaneous tendon ruptures in alkaptonuria. J Bone Joint Surg Br 2003;85:883-6. [Google Scholar]
- 13.Lee WC, Tan TL, Chan YH. Total knee arthroplasty in ochronosis arthropathy: A case report and systematic review. Case Rep Orthop 2019;2019:1871856. [Google Scholar]
- 14.Syam G, John JT, Nair DS, Yadav S, Varghese J, Jamsheed T. Ochronotic surprise during total knee replacement! A case report. J Orthop Case Rep 2021;11:49-52. [Google Scholar]








