The combination of intra- and extra-articular SC is possible but extremely rare. The primary treatment for optimal management entails undergoing a synovectomy and removing loose bodies.
Dr. John Christian Parsaoran Butarbutar, Department of Orthopedics and Traumatology, Siloam Hospitals Lippo Village, Tangerang, Indonesia. E-mail: john.butarbutar@lecturer.uph.edu
Introduction: Synovial chondromatosis (SC) is a relatively rare benign disorder characterized by developing many nodules composed of cartilage within the synovial cavities of joints. It impacts several joints, with the knee joint being the most often affected. Extra-articular involvement, such as bursae or tendon sheaths, is rare. Furthermore, the coexistence of intra- and extra-articular SC is an infrequent condition. Hence, we present a rare case of SC with intra- and extra-articular involvement.
Case Presentation: The patient, a 38-year-old woman, reported experiencing progressive right knee discomfort for 2 months. In addition, a growing mass was observed on the medial aspect of the right knee that was noticeable for the past 2 months. MRI examination revealed the presence of both intra-articular and extra-articular lesions. A two-step surgical procedure, including arthroscopy synovectomy involving the debridement of the lesions and removal of the extra-articular mass through an open incision, was performed. Histopathological analysis confirmed SC. At the 1-year follow-up, the patient reported complete relief of discomfort in the right knee.
Conclusion: The coexistence of extra-articular and intra-articular SC is an exceedingly rare condition. Surgical removal of the loose bodies and a synovectomy performed as thoroughly as possible constitute the mainstay of treatment in managing SC.
Keywords: Synovial chondromatosis, extra-articular, intra-articular, joint loose bodies, knee
Synovial chondromatosis (SC) is an uncommon, benign disorder induced by metaplasia of the synovium into chondrocytes and characterized by multiple cartilaginous nodules or loose bodies within the synovium joints [1]. The disease is typically monoarticular and predominantly affects the knee [1]. The etiology of the disease is uncertain. The incidence rate is one per 100,000, and males are twice as likely to be diagnosed as women, typically between the third and fifth decades of life [2]. Patients with SC may either be asymptomatic or present with pain, swelling, and restriction of movement. The disease is usually intra-articular but can also, in rare instances, be extra-articular and involve bursae, tendinous sheaths, or surrounding soft tissues [1]. The combined intra- and extra-articular form is rare, as in our case [3-5]. In this case report, we describe a patient with both intra- and extra-articular SC of the knee with a distinct feature of form from other cases that have been reported.
The patient, a 38-year-old woman, was granted written authorization to disseminate the data included in this report. The patient exhibited 2-month duration of gradually worsening pain in her right knee. The patient experienced increased pain when she engaged in activities such as climbing stairs and exercising, which limited her ability to walk long distances. The patient’s medical history did not reveal any notable findings. There was no history of injury to the knee before the patient’s symptoms. The patient also complained of a growing mass over the medial aspect of the right knee, which has been noticeable for the past 2 months. The mass formed spontaneously without any prior injury.
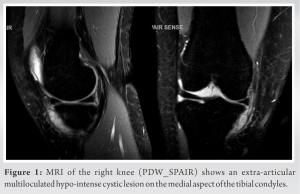
Upon examination, an initial inspection of the right knee revealed no deformity in both knees. On palpation, there was a palpable mass on the anteromedial tibial condyle of the right knee, where moderate intra-articular swelling was also present. The mass was roughly 2 by 2 cm in dimension and had a dense and firm consistency. The border was distinct, uniform, and smooth. While palpating the mass, it was immobile and mildly tender. The patient could fully extend her knee, but discomfort prevented her from flexing it deeply. There was no ligamentous instability found. On the magnetic resonance imaging (MRI) examination, an extra-articular multiloculated hypo-intense cystic lesion (1.8 × 1.2 × 1.4 cm) was identified on the medial aspect of the right anteromedial condyle tibia. In addition, multiple intra-articular lesions were also observed on the tibiofemoral joint space, along with the effusion on the suprapatellar bursa (Fig. 1 and 2).
The patient was planned for elective surgery and underwent a two-stage surgical procedure. The initial phase involved performing a right knee arthroscopy, which was able to note multiple loose bodies in the medial gutter and articular surface of the patella (Fig. 3). The meniscus appears intact with no tears, and no communication between the intra- and extra-articular regions was found. Thus, a synovectomy involving the debridement of these bodies was carried out. The second stage involved a medial open incision on the anteromedial of the knee, which identified a cartilage-like mass measuring approximately 3.5 × 3 cm (Fig. 4). The cartilage-like mass was removed, and the wound was subsequently closed. Both the intra-articular loose bodies and the extra-articular mass were sent for histopathological examination.
The results of the post-operative histopathologic analysis were identical in both samples, confirming our diagnosis of SC. The section showed synovial connective tissue containing multiple hyaline cartilaginous nodules with clustered chondrocyte cells. At 1-year follow-up, the patient reported a total absence of discomfort and the absence of any further swelling in the right knee.
SC is associated with synovial metaplasia with an uncertain etiology [1]. The development of cartilaginous foci in synovial membranes characterizes it [2]. The foci of SC initially develop as immobile cartilaginous bodies. Once the synovial attachment becomes peduncular, it can extend from the synovium and change into loose bodies within the joint space or expand into the soft tissues outside the joint [1]. SC is categorized into primary and secondary SC [1, 2]. The cause of the primary SC has yet to be established. In primary SC, also referred to as idiopathic SC, there are no clear associations with trauma, infection, or genetics. Secondary SC is more frequently encountered. It arises within a joint due to disease and an intra-articular process, resulting in joint destruction and synovitis. Secondary SC is believed to develop because of structural alterations in a joint caused by arthropathy [2]. Milgram et al. [6] reported three phases of the disease based on its histological and radiographic characteristics. During the first phase, active synovitis and the creation of nodules are present. However, the identification of calcifications needs to be seen. During the second phase, the examination reveals the presence of nodular synovitis and loose bodies in the joint. The majority of the loose bodies are remains composed of cartilage. Phase III is distinguished by the resolution of synovitis and the propensity for loose bodies to amalgamate and undergo calcification. The combination of intra- and extra-articular SC is an exceedingly uncommon condition. Several studies have reported a combination form of SC involving the Baker cyst or the popliteal cyst [3-5]. Pathologically, this disease can be distended through an acquired communication between the intra-articular knee joint and a bursa between the gastrocnemius muscle and semitendinosus tendon in this combination. A distinct feature in our case is the extension of the disease into the extra-articular region without substantial communication with the intra-articular space. During knee arthroscopy, the meniscus appeared intact with no tears, and we excluded communication between the intra-articular and extra-articular regions. Based on the arthroscopic findings, a diagnosis of a parameniscal cyst can be ruled out due to the absence of any pathological evidence in the meniscus. A parameniscal cyst is consistently correlated with a structural alteration of the internal meniscus [7]. The phenomenon under consideration involves the extrusion of intra-articular loose bodies through a very narrow aperture into the extra-articular region over an extended period of time, which then closes spontaneously, gradually forming an extra-articular mass. To the extent of our current understanding, there is no prior research or report on this particular illness pattern seen in the knee. The diagnosis of SC is based on the patient’s medical history, physical examination, and radiographic findings. Advanced imaging modalities, such as computed tomography and MRI, play a crucial role in identifying and localizing lesions and differentiating them from other diagnostic possibilities. MRI scans are advantageous in diagnosing and characterizing synovial lesions because they provide high-resolution imaging of soft tissue and non-calcified cartilage nodules [8]. The use of MRI during the first phases of SC has undeniably contributed to enhanced diagnostic capabilities and expedited the early identification and management of SC disorders. SC can be a self-limiting disease [1, 9]. For certain patients, it may be beneficial to consider conservative treatment involving the use of non-steroidal anti-inflammatory drugs (NSAIDs) and activity modification [1, 9]. However, the definite management of SC is the surgical removal of loose bodies with or without synovectomy [1, 9], which is recommended for patients experiencing restricted range of motion and mechanical symptoms such as locking. In the early phases of the disease, synovectomy is sufficient when there are no loose bodies; however, in the intermediate phase, a combination of loose body removal and synovectomy is favored. In most cases, however, the most significant results are obtained by combining synovectomy with removing loose bodies [1-3]. If present, underlying joint pathology should also be treated. A total surgical excision is typically conducted to treat extra-articular SC [1,3-5]. Our case was approached through arthroscopic debridement and synovectomy, combined with an open incision on the knee’s anteromedial to remove intra-articular and extra-articular lesions. Articular degeneration can occur as a consequence of SC. Hence, prompt assessment and management will aid in preventing subsequent complications. Primary SC seldom reoccurs after surgical therapy involving the removal of loose bodies and synovectomy [10]. The occurrence of malignant transition to chondrosarcoma is a recognized consequence, but fortunately, it is an uncommon phenomenon with an incidence ranging between 1% and 6%. [11].
This case report presents a unique instance of SC with a novel characteristic that has not been previously documented. A combination of extra-articular and intra-articular SC is uncommon, but it is possible. The mainstay of treatment is surgery to remove the loose bodies and synovectomy as altogether as possible.
Advanced imaging techniques are essential for improving diagnostic capabilities and accelerating the early detection and treatment of SC diseases. Surgical intervention is the primary and most effective method for treating SC.
References
- 1.Habusta SF, Mabrouk A, Tuck JA. Synovial chondromatosis. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 2.Ko E, Mortimer E, Fraire AE. Extraarticular synovial chondromatosis: Review of epidemiology, imaging studies, microscopy and pathogenesis, with a report of an additional case in a child. Int J Surg Pathol 2004;12:273-80. [Google Scholar]
- 3.Sarangi PK, Kumar TS. Primary synovial chondromatosis of knee with both intra-articular and extra-articular involment: A case report with delayed diagnosis. Oncol J India 2017;1:46-8. [Google Scholar]
- 4.Bassir RA, Ismael F, Elbardouni A, Mahfoud M, Berrada MS, Elyaacoubi M. Bilateral synovial chondromatosis in the knee joint with both intra and extra-articular diseases. Pan Afr Med J 2014;19:57. [Google Scholar]
- 5.Mackenzie H, Gulati V, Tross S. A rare case of a swollen knee due to disseminated synovial chondromatosis: A case report. J Med Case Rep 2010;4:113. [Google Scholar]
- 6.Milgram JW. Synovial osteochondromatosis: A histopathological study of thirty cases. J Bone Joint Surg Am 1977;59:792-801. [Google Scholar]
- 7.Saraiva L, Saraiva AP, Coutinho M, Pereira da Silva JA. Parameniscal cyst: An important differential diagnosis in slow growing masses of the knee. ARP Rheumatol 2023;2:83-4. [Google Scholar]
- 8.Frick MA, Wenger DE, Adkins M. MR imaging of synovial disorders of the knee: An update. Radiol Clin North Am 2007;45:1017-31, vii. [Google Scholar]
- 9.Neumann JA, Garrigues GE, Brigman BE, Eward WC. Synovial chondromatosis. JBJS Rev 2016;4:e2. [Google Scholar]
- 10.Murphey MD, Vidal JA, Fanburg-Smith JC, Gajewski DA. Imaging of synovial chondromatosis with radiologic-pathologic correlation. Radiographics 2007;27:1465-88. [Google Scholar]
- 11.Evans S, Boffano M, Chaudhry S, Jeys L, Grimer R. Synovial chondrosarcoma arising in synovial chondromatosis. Sarcoma 2014;2014:e647939. [Google Scholar]