The “balloon dip” is a post-operative rehabilitation trend that is exhibited by a small yet substantial proportion of balloon patients and is characterized by a transient deterioration in pain and function around 3–6 months mark following balloon implantation
Dr. Joseph A Abboud, Division of Shoulder and Elbow Surgery, Rothman Orthopedic Institute, Philadelphia, Pennsylvania, USA. E-mail: abboudj@gmail.com
Introduction: The subacromial balloon is a novel therapeutic device that is used in patients with massive irreparable rotator cuff tears (MIRCTs). The novelty of this device implies that there is still a lot to be known about its mechanism of action and rehabilitation trends. One rehabilitation trend that has been noticed is the “balloon dip”, where a patient exhibits exacerbations in pain and function around 3 months following balloon implantation and after having experienced earlier symptomatic relief post-operative. We discuss the clinical, diagnostic, and therapeutic aspects of the patient’s management while providing additional insight into this prognostic trend.
Case Report: In this report, we present the case of a 65-year-old male patient who underwent a subacromial balloon procedure for a MIRCT. During his recovery, the patient exhibited a classic “balloon dip” evident by an exacerbation of pain and function around the 3-month mark. After a notable deterioration in pain and function, the patient was examined, reassured, and educated on the importance of adhering to physical therapy. He was able to successfully recover and showed gradual improvement in pain and function along the course of the year.
Conclusion: The “balloon dip” is a rehabilitation pattern that occurs 3–6 months following subacromial balloon spacer implantation. In the majority of cases, careful clinical assessment, watchful monitoring, and education on the importance of following up with physical therapy are sufficient to overcome the dip.
Keywords: Subacromial balloon, balloon dip, deflation, shoulder, balloon resorption.
The subacromial balloon spacer is an interpositional device that inserts between the humeral head and acromion in patients with massive irreparable rotator cuff tears (MIRCTs) [1]. The balloon, which was Food and Drug Administration (FDA)-approved for indicated use in the US in 2021, helps decrease pain in MIRCT patients by relieving acromiohumeral impingement and improves joint function by redistributing forces toward adjacent musculature [2]. This device constituted a new treatment option for shoulder surgeons and has demonstrated efficacy in MIRCT patients with appropriate indications, i.e., those with minimal osteoarthritis, intact subscapularis, and the ability to forward elevate their shoulder to 90°, among other indications [2]. Studies exploring the clinical outcomes of the balloon in its indicated population have generally shown good results [1,3-5]. A pivotal randomized controlled trial by Verma et al. compared partial cuff repair to subacromial balloon placement in patients with MIRCTs and noted non-inferior outcomes in the balloon group while highlighting a speedier recovery and a shorter surgical time in the balloon group [3]. The findings of that study were echoed by several other studies in the literature that confirm the utility and clinical efficacy of the subacromial balloon in improving patient-reported outcomes postoperatively [1,3-5]. Being a relatively novel device, there is still a lot to learn about the subacromial balloon spacer in the setting of MIRCT patients. Exploring outcomes and reporting on post-operative trends and patterns are important for the education of shoulder surgeons and patients alike. In our practice, it has been noticed that in a small subset of balloon patients, a post-operative pattern of recovery can be appreciated: An initial improvement in pain and function, followed by an exacerbation of performance that starts around the 3–6-month mark, is to be followed by a subsequent rise in performance and recovery, given that the right management is advised. There have been no studies or reports to date that describe this exacerbation in performance, termed the “balloon dip”. In this report, we describe the case of a 57-year-old male balloon patient who exhibited a well-documented “balloon dip,” while appropriately discussing management options and recovery.
A 65-year-old right-hand dominant male chef presented to our clinic with right shoulder pain and dysfunction. The patient was previously healthy, had no previous surgeries in his affected joint, and had normal shoulder function until he pushed on a heavy door and felt a snap in his shoulder 2 months before his presentation. He attempted physical therapy before his clinical presentation and noted mild improvement in his range of motion but persistence of pain and dysfunction. He was using non-steroidal anti-inflammatory medications for pain control. He has no pertinent medical history, and his surgical history includes a previous hernia repair. On physical assessment, he exhibited full passive range of motion and was able to reach 170° in active forward elevation, 80° in active abduction, 30° in active external rotation, and his upper lumbar spine in active internal rotation. The patient had positive Jobe’s and Hawkin’s tests and had a negative belly press test. He had no apprehension or signs of instability, and he had no bruising or swelling in his affected upper extremity. He was neurovascularly intact. His American shoulder and elbow surgeons (ASES) score was 39.5; his visual analog scale (VAS) pain score was 5/10; and his single assessment numeric evaluation (SANE) score was 25%. X-ray imaging revealed mild arthritic changes with no significant lesions or fractures (Fig. 1).
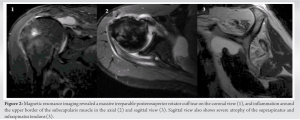
The patient had the clinical vignette of a rotator cuff tear in the setting of his recent injury, and a magnetic resonance imaging (MRI) study was ordered to fully assess his presentation. The MRI study showed a massive posterosuperior rotator cuff tear involving the supraspinatus and infraspinatus tendons with retraction medial to the level of the glenoid margin (Fig. 2).
There was an effusion evident in the subacromial space and around the subscapularis tendon, but no significant tear in the subscapularis tendon was appreciated (Fig. 2). On sagittal view, the supraspinatus and infraspinatus muscle bellies showed grade 4 Goutailler fatty infiltrations, while the subscapularis and teres minor muscle bellies showed no atrophy (Fig. 2). There was minimal osteoarthritis present. Given the patient’s clinical presentation and imaging findings, he was diagnosed with a MIRCT–acute on chronic presentation–of both his supraspinatus and infraspinatus tendons. The patient was informed about his diagnosis and possible management options. Given his preserved range of motion, his minimal osteoarthritis, and the good condition of his subscapularis muscle, the treatment plan was decided on the placement of a subacromial balloon spacer in his right shoulder. During the procedure, the subacromial space was assessed, and the subscapularis tendon was deemed in good condition and did not necessitate repair. A medium-sized balloon was chosen in accordance with device indications, and 15 mL of saline were used to inflate the balloon inside the patient’s joint. The procedure was well tolerated, and the patient was placed in a sling for 10 days up until his first post-operative visit, after which the sling was removed and the patient was instructed to start physical therapy. The patient was doing well with his post-operative recovery. At around the 2-month mark, the patient had 130° of active forward elevation, and his VAS pain score decreased to 3.5 (Fig. 3).
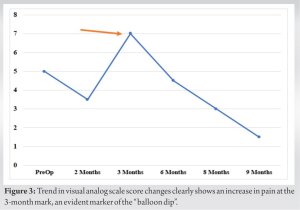
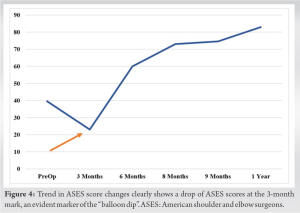
Our case describes a distinct pattern of recovery that is witnessed in a small yet significant subset of subacromial balloon spacer patients. This “balloon dip” can be discouraging to patients and shoulder surgeons who are unfamiliar with the intricacies and details of the balloon procedure, and hence, reporting on similar experiences can be very beneficial for overall management and treatment. The subacromial balloon is a relatively novel device that got FDA approval in 2021 [6, 7]. This novelty entails much to be known and discovered about its outcomes and rehabilitation patterns [6, 7]. While the balloon dip has been suggested by different surgeons, there are no published studies that confirm or report an accurate incidence. In our practice, the “balloon dip” is estimated to affect around 5–10% of balloon patients post-operatively; nevertheless, holistic clinical studies should be conducted to appropriately quantify the prevalence and incidence of this phenomenon. Several factors can explain the etiology of the “balloon dip.” One major factor is balloon resorption. The subacromial balloon spacer is made out of a biodegradable polymer material that is expected to be completely absorbed in the joint by 12 months [1, 2, 6, 8, 9]. However, it has been suggested that the balloon begins to resorb by 3 months, and this deflation may lead to the increase in pain seen in dipping patients [1, 2, 6, 8, 9]. Upon deflation, the balloon may lose some of its spacer properties, and hence, some patients may re-experience some of the symptoms felt before their procedure. In this regard, it is important to educate patients on the initial role of the subacromial balloon and the importance of early rehabilitation. The subacromial balloon should be considered a “rehabilitation accelerator” [6, 7]. It should alleviate pain and improve function in MIRCT patients to allow them to conduct physical therapy in a more efficient way [6, 7]. This accelerated physical therapy can then help procure benefits that can outlast the duration of the balloon’s existence in the joint [7, 10-12]. Other patient-related factors can contribute to the “balloon dip” as well. The initial improvement in pain and function exhibited following balloon implantation can sometimes provide patients with a false sense of assurance and security. As such, many patients may skip physical therapy sessions and/or clinical visits due to the improvement exhibited early on post-operatively. This leads to early deterioration in strength and symptomatic exacerbations. Other patients may obtain a false sense of security due to the initial symptomatic improvement and conduct excessively strenuous activities that are not advised post-operatively, leading to exacerbation of injury and worsening of symptoms. “Balloon dip” cases can be prevented by administering proper education on the subacromial balloon spacer’s role and recovery to the patient before the procedure. Understanding the goals and rationale behind this device is pivotal to both the surgeon and the patient and helps set appropriate expectations and treatment goals. When a dipping patient presents to the clinic, usually around 3–6-month postoperatively, it is important to conduct a holistic clinical investigation to assess for any novel injuries. In cases where the clinical assessment does not provide any remarkable impressions, watchful monitoring, providing reassurance, and continuing physical therapy are the appropriate steps to take toward overcoming the balloon dip. The dipping patient, similar to our case, is often expected to make gradual improvements up until symptomatic relief and full recovery. In the rare cases where the dip persists beyond 3 months without improvement, ordering imaging studies like MRIs can provide additional insight into the mode of symptomatic exacerbation and whether any remarkable injuries or lesions require to be addressed. At that stage, discussing more invasive options such as shoulder replacement procedures may be necessary.
The subacromial balloon is a novel device that is used to treat patients with MIRCTs. Having been recently approved by the FDA in the US, details about its mechanism and intricacies about its recovery process are yet to be uncovered. One unreported yet notable pattern of recovery is the “balloon dip,” where the patients exhibit a deterioration in pain and function around 3–6 months post-balloon procedure, after having noted significant improvements early on in the recovery. One major factor that may contribute to the “balloon dip” is balloon resorption, which may start as soon as 3 months following implantation. Other factors include the false sense of security provided by early pain relief, which may allow patients to skip physical therapy or engage in excessively strenuous activities, thereby causing an exacerbation of injury. When a dipping patient presents, a careful clinical assessment should be conducted, and in the majority of cases, watchful monitoring, providing reassurance, and insisting on the importance of following through with physical therapy are sufficient to allow the patient to overcome the dip. Educating patients on the role of the balloon and the importance of rehabilitation is essential for setting appropriate expectations and treatment goals.
- The “balloon dip” is a rehabilitation pattern seen in the post-operative course of MIRCT patients who underwent subacromial balloon implantation.
- The “balloon dip” is characterized by a deterioration in pain and function following at around 3–6-month post-operative, following an initial improvement.
- Reassurance and adherence to physical therapy are often sufficient to help the patient overcome the “balloon dip”.
References
- 1.Savarese E, Romeo R. New solution for massive, irreparable rotator cuff tears: The subacromial “biodegradable spacer”. Arthrosc Tech 2012;1:e69-74. [Google Scholar]
- 2.Wright MA, Abboud JA, Murthi AM. Subacromial balloon spacer implantation. Curr Rev Musculoskelet Med 2020;13:584-91. [Google Scholar]
- 3.Verma N, Srikumaran U, Roden CM, Rogusky EJ, Lapner P, Neill H, et al. Inspace implant compared with partial repair for the treatment of full-thickness massive rotator cuff tears: A multicenter, single-blinded, randomized controlled trial. J Bone Joint Surg Am 2022;104:10:1250-62. [Google Scholar]
- 4.Holschen M, Brand F, Agneskirchner JD. Subacromial spacer implantation for massive rotator cuff tears: Clinical outcome of arthroscopically treated patients. Obere Extrem 2017;12:38-45. [Google Scholar]
- 5.Johns WL, Ailaney N, Lacy K, Golladay GJ, Vanderbeck J, Kalore NV. Implantable subacromial balloon spacers in patients with massive irreparable rotator cuff tears: A systematic review of clinical, biomechanical, and financial implications. Arthrosc Sports Med Rehabil 2020;2:e855-72. [Google Scholar]
- 6.Fares MY, Khan AZ, Abboud JA. Interpositional balloon: A new frontier. Oper Tech Sports Med 2023;31:150983. [Google Scholar]
- 7.Stewart RK, Kaplin L, Parada SA, Graves BR, Verma NN, Waterman BR, et al. Outcomes of subacromial balloon spacer implantation for massive and irreparable rotator cuff tears: A systematic review. Orthop J Sports Med 2019;7:2325967119875717. [Google Scholar]
- 8.Srikumaran U, Russo R, Familiari F. Subacromial balloon spacer for massive irreparable rotator cuff tears. Arthroscopy 2023;39:576-7. [Google Scholar]
- 9.Dey Hazra RO, Dey Hazra ME, Hanson JA, Millett PJ. The InSpace balloon: Useful augmentation or first-line therapy?: Commentary on an article by Nikhil Verma, MD, et al.: InSpace implant compared with partial repair for the treatment of full-thickness massive rotator cuff tears. A multicenter, single-blinded, randomized controlled trial”. J Bone J Surg Am 2022;104:e65. [Google Scholar]
- 10.Fares MY, Abboud JA. Effective management of bilateral massive irreparable rotator cuff tears through implantation of subacromial balloon spacers. J Orthop Case Rep 2023;13:52-6. [Google Scholar]
- 11.Daher M, Pearl A, Zalaquett Z, Elhassan BT, Abboud JA, Fares MY, et al. InSpace balloon for the management of massive irreparable rotator cuff tears: A systematic review and meta-analysis. Clin Orthop Surg 2023;15:834-42. [Google Scholar]
- 12.Luthringer TA, Fares MY, Rondon AJ, Vaughan AK, Khan AZ, Abboud JA, et al. Subacromial balloon spacer versus partial rotator cuff repair in the treatment of massive irreparable rotator cuff tears: Facility personnel allocation and procedural cost analysis. Cureus 2023;15:e41538. [Google Scholar]