Severity of deformity is not a contraindication for cruciate retaining knee replacement.
Dr. James C George, Department of Orthopaedic Surgery, Believers Church Medical College Hospital, Thiruvalla, Pathanamthitta, Kerala - 689 103, India. Email: drjamescgeorge@gmail.com
Introduction: There has been debate regarding the advantages of cruciate-retaining over posterior stabilized (PS) knee arthroplasty and vice versa. Many authors consider any coronal plane deformity >15° as a contraindication for cruciate-retaining total knee arthroplasty. We aimed to compare whether functional outcome, deformity correction, and survivorship of cruciate retaining knee arthroplasty (CR) for severe varus deformity are equivalent to that of posterior cruciate ligament substituting (PS) for 6 years.
Materials and Methods: We conducted a retrospective comparative study among patients who underwent Total Knee Replacement in the Orthopedics Department of a tertiary care hospital between 2016 and 2018 August who had a varus deformity of more than 15°. The first author exclusively performed CR operation (Group A) for all complex knees. In contrast, the second author performed PS surgery (Group B) for any coronal plane deformity over 15°. Clinical evaluation included completing a Knee Society Score (KSS) Evaluation Form. Pre-operative scoring was collected from the hospital database. All clinical examinations and radiographs at the final follow-up were done by the third author, who was unbiased and not involved with the initial patient care.
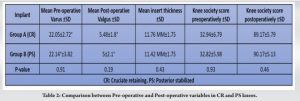
Results: There were 39 patients in Group A (CR) and 28 patients in Group B (PS). In Group A, the mean pre-operative varus was 22.05 ± 2.72° and the pre-operative KSS was 32.94 ± 6.79. Postoperatively, the deformity corrected to a mean valgus of 5.48 ± 1.8° and mean KSS of 89.17 ± 5.79. In Group B, the mean pre-operative varus was 22.14±3.82° and pre-operative KSS was 32.82 ± 5.98. Postoperatively, the deformity corrected to a mean valgus of 4.85 ± 2.1° and mean KSS of 90.17 ± 5.13. The mean insert thickness was 11.76 ± 1.75 mm and 11.42 ± 1.75mm among the CR and PS groups, respectively. Concerning deformity correction (P = 0.19) and functional outcome (P = 0.46), both groups showed equal improvement with a 100% survival rate for 6 years.
Conclusion: We concluded that CR knee replacements are possible with excellent functional and radiological outcomes in severe varus arthritic knees with a 100 % survival rate.
Keywords: Arthritis, total knee arthroplasty, cruciate retaining, posterior stabilizing, varus deformity.
There have been advocates for cruciate-retaining and cruciate substituting knee arthroplasty debating regarding the superiority of one over the other. Many authors consider any coronal plane deformity >15° as severe enough to require intraoperative conversion to posterior stabilized (PS) design [1-3]. They argue that retaining the posterior cruciate ligament (PCL) in such cases can make soft-tissue balancing more difficult, and the PCL may contribute to the deformity. The first author exclusively performed cruciate retaining (CR) arthroplasty for all complex knees, while the second author performed PS surgery for any coronal plane deformity over 15°. The study aimed to compare CR and PS arthroplasty done for severe knee deformities and the objective was to compare the functional outcome, radiological outcome, and survivorship of these two groups.
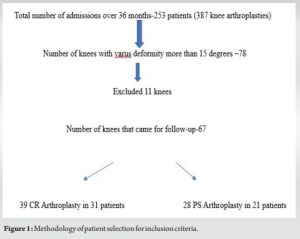
From 2016 to 2018 August the total knee arthroplasties done by both authors were collected from the hospital database after getting institutional review board approval. All patients with 15° or more varus deformity in the standing antero-posterior X-ray were included in the study. Inclusion criteria were exclusively radiological irrespective of age, sex, weight, and other medical conditions. Any deformity <15° or any valgus deformity was excluded from the study (Fig. 1).
The first author exclusively performed CR operation (Group A) for all complex knees. In contrast, the second author performed PS surgery (Group B) for any coronal plane deformity over 15°. The varus angle measurement was done using Medsynapse Picture Archiving and Communication system version 5.3.0.0. Both authors used Genesis II Smith and Nephew through the medial parapatellar approach for all the knee arthroplasties. The first author preferred a gap resection technique and PCL balancing with a cruciate-retaining design. He kept the tibial resection to a minimum, with the maximum thickness being 6 mm from the lateral tibial plateau. The tibial slope was kept to between 7 and 10°. While the second author preferred a measured resection technique with the tibial cut being the same as the first author but keeping the slope to 3–5° and a PS design. Both surgeons kept the distal femoral cut to 5° of valgus and a posterior referencing system for anterior and posterior cuts. Once the cuts were made and the trials were placed, soft tissue releases were performed to obtain, as best possible, rectangular flexion and extension spaces. Clinical evaluation, pre and postoperatively, included physical examination radiological evaluation, and completing a Knee Society Score (KSS) evaluation form. Pre-operative scoring was collected from the hospital database. All clinical evaluations at the final follow-up were done by the third author after obtaining informed consent from the patient. Weight-bearing anteroposterior and non-weight-bearing lateral radiographs of the operative knees were taken at all follow-up visits. Radiographs were reviewed for alignment of the implants as well as for evidence of polyethylene wear, osteolysis, or radiolucencies. Statistical analysis was performed using Student’s t-test.
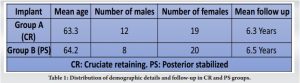
During the study period, 387 knee arthroplasties (253 patients) operated by both authors in 36 months from 2016 to 2018. Among them, 78 knees had a varus deformity of more than 15°. All patients with severe deformity operated by both authors were followed up. Seven patients in Group A and four patients in Group B did not come for follow-up. Finally, Group A had 39 CR arthroplasties in 31 patients and Group B had 28 knees in 21 patients (Table 1).
The mean age at the time of surgery was 63.3 years (range, 48–82 years). Seventeen patients underwent bilateral knee replacement, but only those knees with more than 15° varus were included. The mean follow-up was 6.3 years (5–7 years). Except for three patients who had rheumatoid arthritis, all remaining patients had primary osteoarthritis. In five patients, 3.5 mm screws were used to build up the tibial defect. Postoperatively, two patients developed deep vein thrombosis, one patellar dislocation, and two superficial surgical site infections. In Group A, the mean pre-operative varus was 22.05 ± 2.72° (range 15–30). The mean pre-operative poly insert thickness was 11.76 mm ± 1.75 (range 9–15). The mean post-operative correction achieved was 5.48° ± 1.8 valgus (range, 2–9°) (Fig. 2).
The KSS improved from a mean of 32.94 ± 6.79 (range, 20–45) preoperatively to a mean of 89.17 ± 5.79 (range, 80–95) at latest follow-up. The mean pre-operative range of motion was from 20° (range, 0–40) of flexion contracture to 100° (range, 70–120) of flexion. At the most recent follow-up, this improved to a mean 5° (range, 0–10) of flexion contracture to 120° (range 90–130) of flexion. None of the knees had posterior translation as assessed manually at 90° of flexion and or laxity to valgus-varus manual stress in full extension and mid-flexion. There were not any revision surgeries till the last follow-up. There was no radiological evidence of loosening of progressive posterior cruciate ligament insufficiency. Considering revision as an endpoint, the survivorship for CR knee in severe deformity in our study was 100%. In Group B, there were seven bilateral knee replacements. There were 20 females and eight males with a mean age of 64.2 (range 58–80). The mean follow-up was 6.5 years. All patients had primary osteoarthritis and none of them developed any post-operative complications. The mean pre-operative varus was 22.14 ± 3.82° (range 15–30). The mean poly size was 11.42 ± 1.75 mm, with 15 mm poly used in patients with 30° deformity. A mean post-operative correction was valgus to 5° (range 2–8°) (Fig. 3).
The KSS improved from 32.82 ± 5.98 (range 20–45) preoperatively to a post-operative score of 90.17 ± 5.13 (range 75–95). The mean pre-operative flexion deformity was 18° (range 0–35) and postoperatively, the flexion deformity was a mean of 5° (range 0–10) at the final follow-up. Pre-operative flexion was 95° (range 45–110°) and post-operative flexion was 110° (range 90–120°) at the final follow-up. Mediolateral and anteroposterior instability were not present in any of the patients. None of them developed osteolysis or underwent any revision for loosening. Both groups showed improvement concerning deformity correction and functional outcome. There was no significant difference between the two groups regarding the correction of deformity (P = 0.19), functional improvement (P = 0.46), insert size (P = 0.43) age, and revision rates (Table 2). The post-operative complication was more common among the CR group but was not statistically significant.
Severe coronal plane deformity is considered a contraindication for CR knee arthroplasty by many authors. We reviewed the 6-year results of cruciate-retaining arthroplasty exclusively to that of PS surgery for any coronal plane deformity more than 15°. Severe valgus coronal plane deformity was not included since the number of patients was very few. Our results in 67 patients showed equal results on comparing both the groups with a 100% survival rate for both at 6-year follow-up. Our study was similar to that done by Laskin [2], but the number of patients was less in both groups. His study at 10 years follow-up showed loosening and decreased survivorship in patients with 15° fixed varus deformity who underwent cruciate-retaining total knee arthroplasty. Kubiak et al., [4] in their study on 64 patients, showed 93% 10-year follow-up in similar severe deformity with two revisions done for infection rather than aseptic or mechanical loosening. Our study on 38 CR knees supported the findings of Kubiak et al. While he used 61-lipped poly as inserts in our study, only 5-lipped inserts were used. All the five were used with 15 mm inserts. Our study was on more severe varus deformity with a mean of 22° in both groups and without using a stemmed design. Scott and Volatile [5] used a PS design for deformity >30° in the coronal plane in their 12-year follow-up on 800 cruciate-retaining knees. Adrian et al. [6] suggested the use of a modular tibial stem to reduce the revision rate due to mechanical loosening. Emerging evidence has suggested that both obesity and stemless or short native stem design may be associated with early aseptic loosening in total knee arthroplasty [7]. Hegde et al. suggested using a prophylactic stem during arthroplasty with deformity of more than 8 degrees to prevent aseptic loosening [8]. Our study uses a Genesis II design with a native stem of 50 mm compared to other designs like Nexgen, where the modular stem starts with 30 mm extensions. There is some controversy that the PCL recession essentially renders the PCL incompetent and should be addressed as such. Our clinical results show no evidence of late PCL insufficiency in the short-term follow-up of these knees requiring recession. The lipped insert was used whenever in doubt regarding PCL incompetency after balancing. Worland et al. [9] have also shown that patients who underwent simultaneous bilateral CR TKA with PCL recession on only one side had no increased laxity in the recessed knee on KT-1000 testing at a mean of 4-year follow-up. Backside wear can develop in highly constrained implants and also if the polyethylene thickness is considerably greater than usual [10]. The strength of our study is the severity of deformity we have corrected using a CR knee which is not seen in any other studies. The study has limitations regarding patient numbers and short follow up but the early results are promising for CR knees in severe deformities.
CR knee replacements are possible with excellent functional and radiological outcomes in severe varus arthritic knees with a 100% survival rate.
Cruciate retaining knee arthroplasty, when done for severe deformities, the BMI of the patient, and the length of the native tibial stem are also important along with PCL balancing and surgical technique.
References
- 1.Teeny SM, Krackow KA, Hungerford DS, Jones M. Primary total knee arthroplasty in patients with severe varus deformity. A comparative study. Clin Orthop Relat Res 1991;273:19-31. [Google Scholar]
- 2.Laskin RS. The insall award. Total knee replacement with posterior cruciate ligament retention in patients with a fixed varus deformity. Clin Orthop Relat Res 1996;331:29-34. [Google Scholar]
- 3.Elkus M, Ranawat CS, Rasquinha VJ, Babhulkar S, Rossi R, Ranawat AS, et al. Total knee arthroplasty for severe valgus deformity. Five to fourteen-year follow-up. J Bone Joint Surg Am 2004;8:2671-6. [Google Scholar]
- 4.Kubiak P, Archibeck MJ, White RE Jr. Cruciate-retaining total knee arthroplasty in patients with at least fifteen degrees of coronal plane deformity. J Arthroplasty 2008;23:366-70. [Google Scholar]
- 5.Scott RD, Volatile TB. Twelve years’ experience with posterior cruciate-retaining total knee arthroplasty. Clin Orthop Relat Res 1986;205:100-7. [Google Scholar]
- 6.Hinman AD, Prentice HA, Paxton EW, Kelly MP. Modular tibial stem use and risk of revision for aseptic loosening in cemented primary total knee arthroplasty. J Arthroplasty 2021;36:1577-83. [Google Scholar]
- 7.Garceau SP, Pivec R, Teo G, Chisari E, Enns PA, Weinblatt AI, et al. Increased rates of tibial aseptic loosening in primary cemented total knee arthroplasty with a short native tibial stem design. J Am Acad Orthop Surg 2022;30:e640-8. [Google Scholar]
- 8.Hegde V, Bracey DN, Brady AC, Kleeman-Forsthuber LT, Dennis DA, Jennings JM. A prophylactic tibial stem reduces rates of early aseptic loosening in patients with severe preoperative varus deformity in primary total knee arthroplasty. J Arthroplasty 2021;36:2319-24. [Google Scholar]
- 9.Worland RL, Jessup DE, Johnson J. Posterior cruciate recession in total knee arthroplasty. J Arthroplasty 1997;12:70-3. [Google Scholar]
- 10.Wasielewski RC. The causes of insert backside wear in total knee arthroplasty. Clin Orthop Relat Res 2002;404:232-46. [Google Scholar]