Modular prosthesis could decrease the chances of limb lengthening following hemiarthroplasty in neck of femur fractures.
Dr. Prannoy Paul, Department of Orthopedics, Government Medical College, Kannur, Kerala, India. E-mail: prannoypaul@gmail.com
Introduction: The incidence of hip fractures is increasing every year worldwide. Even though hemiarthroplasty is one of the most common procedures performed for a fractured neck of the femur, there is very little research comparing the outcomes of monoblock and modular systems, the two most commonly used prostheses in neck of the femur fractures. It was hypothesized that in narrow femoral canals, the single-size monoblock stem would be more difficult to insert and lead to complications like limb lengthening and intra-operative calcar fractures. The objective of our study was to compare the outcomes of a modular prosthesis with that of a monoblock prosthesis in a fractured neck of the femur.
Materials and Methods: This study analyzed the surgical outcomes of 192 cases of hemiarthroplasties performed over a 4-year period using a modular system and compared it to 192 cases performed using a single-sized monoblock system.
Results: The monoblock systems were more likely to cause post-operative limb lengthening compared to their modular counterparts (P = 0.01). The incidence of intra-operative fractures was also more in the monoblock system, although it was not statistically significant. Up to 45% of patients required a femoral stem size smaller than the single-sized monoblock system as the optimum size for their femoral canals, which was available only in the modular system
Conclusions: Modular prosthesis was found to have lower chances of post-operative limb lengthening and lower chances of intraoperative calcar fractures compared to monoblock prosthesis. Careful pre-operative radiologic planning is essential in cases where monoblock systems are used, and the modular system might serve as a viable solution in such scenarios.
Keywords: Hip fracture, hemiarthroplasty, modular, monoblock, lengthening, complications.
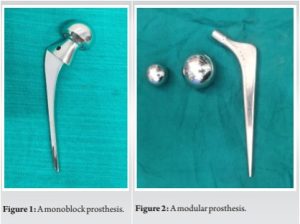
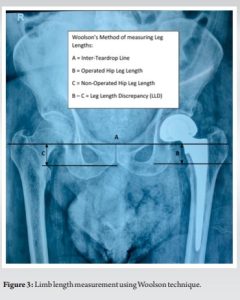
Hip fractures account for a good proportion of cases reporting to the orthopedic department and amount to a major public health issue worldwide. Around 1.5 million cases of hip fractures occur annually across the world, with estimates predicting an increase in this number to an annual incidence of about 3.9 million cases by the year 2050 [1]. Hip fractures are associated with high rates of morbidity and mortality, with around half a million hip fracture-related deaths reported annually across the world [2]. With increasing life expectancy and a rise in the geriatric population, these numbers are expected to rise significantly in the coming decades. Hip fracture surgeries are also associated with various short- and long-term complications. Ten-year follow-up studies have reported that up to 20% of cases of hemiarthroplasties required a revision surgery in the future [2]. Hence, adequate pre-operative planning is required to reduce the incidence of complications in these patients. Various prostheses are now available for hemiarthroplasty in femoral neck fractures. The updated National Institute of Clinical Excellence CG124 (NICE) guidelines recommend smooth stem prosthesis inserted with cement for hip hemiarthroplasty from the results of recent studies [3]. Review studies have reported less pain, improved mobility, and long-term survivorship with cemented stems over uncemented stem prosthesis [4]. Further, a recent meta-analysis has also reported better range of motion, lower rates of acetabular erosion, and lower reoperation rates for bipolar prosthesis compared to the unipolar variant, but at the expense of longer operative time [5]. The prostheses are also available in monoblock and modular variants. Monoblock prosthesis is manufactured as a single piece (Fig. 1), and the size of the prosthesis to be implanted is chosen based on the dimensions of the femoral head. A monoblock prosthesis rests on the femoral neck at a fixed point decided by the level of the osteotomy above the lesser trochanter. Hence, the level of femoral neck cut plays a key role in the post-operative limb length in monoblock prosthesis. Thus, it may not be able to recreate the patient’s anatomy very accurately. A modular prosthesis, on the other hand, is manufactured in three separate components: the bipolar cup, the femoral metal head, and the stem (Fig. 2). For each size of the bipolar cup, various options are available for the femoral head (offset) as well as the femoral stem component. This provides the surgeon with a better opportunity to recreate the patient’s anatomy more accurately with the modular prosthesis. However, the clinical relevance of such a difference is still uncertain. Monoblock systems are universal in size and usually have a fixed offset of 40 mm [6]. Furthermore, due to the universal stem size of the prosthesis, there are chances for intra-operative calcar or femoral fractures, increased operating time, and post-operative over lengthening of the limb [6]. Modular stems, on the other hand, have various stem sizes available to match with the diameter of the femoral canal better and also provide various offset options within the same stem. Thus, it is hypothesized that modular stems are superior in controlling over lengthening and have a lower tendency for calcar fractures. However, very few studies have compared a monoblock system with a modular system in the treatment of intracapsular neck of femur fractures. Our study compared the intra-operative and post-operative complications associated with monoblock prosthesis with that of a modular prosthesis.
This was a prospective observational study. The study was approved by the institutional review board and the institutional ethics committee. Informed consent was obtained from all patients who participated in the study. All patients undergoing a hemiarthroplasty of the hip for a fractured neck of the femur in our hospital from January 2019 to December 2022 were recruited into the study sample. A total of 192 patients underwent hemiarthroplasty with a modular prosthesis during the study period. A cohort of 192 patients who underwent hemiarthroplasty of the hip with monoblock prosthesis during the same study period was also recruited for the study sample. Both monoblock and modular prostheses were routinely being used in our department, and the implant was chosen according to the preference of the operating surgeon. For modular hemiarthroplasty, prostheses by Biorad Medisys (Biorad Medisys Pvt. Ltd.,) were used, and for monoblock systems, prostheses by Hardik (Hardik International Pvt. Ltd.) were used. Pre-operative template was done to assess the level of the femoral neck cut required, adjusting for the dimensions of the prosthesis and any pre-existing limb length discrepancies. The approach used in all cases was the anterolateral modified Hardinge approach to the hip, with the patient in lateral position. The femoral head was extracted and sized appropriately to choose the appropriate size for the femoral head. Trial reduction was performed in all cases before definite implantation. All femoral stems, both modular and monoblock, were implanted using DePuy gentamicin bone cement (DePuy International Ltd., Leeds, UK). All patients received ceftriaxone 1 g IV 30 min before induction and 12 h post-operatively. The wounds were closed using Vicryl sutures and skin staplers. All patients were made to mobilize early and encouraged weight bearing from post-operative day 1. All relevant patient data, including age, American Society of Anesthesiologists (ASA) score, and pre-operative albumin and hemoglobin levels, were recorded. The primary outcome measured was post-operative limb length discrepancy, and the secondary outcomes were operating time, incidence of calcar fractures, blood loss, duration of hospital stay, and mortality. The X-rays were analyzed using the Patient Archiving and Administration System (PACS, GE Medical Systems 2022). Post-operative limb length was measured on post-operative day 12 (at the time of discharge) radiographically on a pelvis X-ray with both hips in anteroposterior view with the patient standing with hips in extension and maximal internal rotation, using the Woolson methodology, from the acetabular teardrop to the lesser trochanter (Fig. 3) by a single reviewer for all patients [7].
Blood loss was calculated by the drop in hemoglobin levels compared to the pre-operative value. Patients were followed up at 1 month, 3 months, and 6 months. The statistical analysis was carried out using SPSS software for Windows (version 20). Continuous variables were analyzed using an unpaired t-test, and a p< 0.05 was considered statistically significant.
The age of the patients ranged from 52 years to 97 years, with a mean age of 68 years. The mean follow-up period was 1.3 years. Females constituted 61% of the total patients. The patient characteristics of the monoblock and the modular group are summarized in Table 1.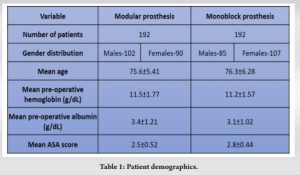
The mean age, ASA score, pre-operative hemoglobin, and albumin levels of both groups were similar, and the differences between the two groups were not statistically significant. The details of the surgery and post-operative X-ray analysis of the two groups are summarized in Table 2. The monoblock prosthesis was more likely to produce post-operative limb lengthening than the modular system, and the difference was statistically significant (p = 0.01). In the monoblock prosthesis group, 21 patients had a post-operative limb lengthening and 7 had a limb shortening, compared to the modular group, where only 8 patients had a post-operative limb lengthening and 3 patients had a limb shortening. The average limb lengthening and shortening of each group is shown in Table 2.
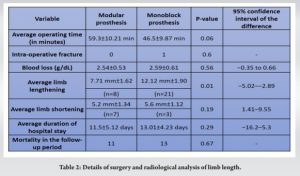
The operating time was relatively lesser for monoblock prosthesis than modular variants; however, the difference was not statistically significant (p = 0.06). The differences in average blood loss, which was measured by the drop in hemoglobin compared to the pre-operative level, were comparable. There was one incident of intraoperative calcar fracture, and this was in the monoblock group. The modular group did not have any fractures intraoperatively. The duration of hospital stays was comparable between the 2 groups. The mortality rate overall was 6% at the end of the follow-up period. Various stem sizes were used in the modular group according to the size of the femoral canal. The distribution of various stem sizes used in the modular prosthesis group is shown in Table 3. There were 2 cases of post-operative prosthesis dislocation, one each in the modular and monoblock groups, during the follow-up period.
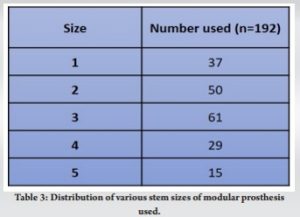
As the incidence of hip fractures increases, risk stratification and pre-operative planning become more important in reducing the rates of complications associated with the surgery. Previous studies have analyzed the outcomes of cemented with uncemented prostheses and bipolar with monopolar prostheses [8, 9]. The latest NICE clinical guidelines recommend a cemented prosthesis as the preferred implant for neck of femur fractures [3]. Modular and monoblock systems are widely available and are being used for hemiarthroplasties in fractures of the neck of the femur worldwide. However, there is very little research comparing the outcomes of these implants. The femur size and density differ in each patient and are also influenced by the age and gender of the patient [10]. For instance, females usually have relatively smaller and more osteoporotic femurs compared to males in the same age group [10]. Interestingly, females also constitute the majority of the patients presenting with a fractured neck of the femur due to pre-existing osteoporosis, as was the case in our study. A recent study on patients undergoing hip replacement noted that up to 20.6% of female patients and 10.3% of male patients had offset lengths different than the standard lengths available with the prosthesis [11]. Hence, proper pre-operative assessment of the femoral canal is essential to avoid complications and attain optimum results. This study indicates that monoblock stems are more likely to cause post-operative limb lengthening compared to modular systems (p = 0.01). The dimensions of the stem of the monoblock prosthesis were similar to the size 3 stem of the modular system, as measured from the implant templates. However, in our study, 45% (n = 87) of the patients who underwent a modular prosthesis required stem sizes <3 as the optimum size for their femoral canals. If a monoblock system was used for these patients, it could have resulted in complications like limb lengthening, difficulty in reduction, or intra-operative fractures. Another added advantage of the modular system is that it can be converted into a total hip replacement if such a need arises in the future by changing only the femoral head and retaining the stable cemented femoral stem. The revision rate after a hemiarthroplasty is about 20% at 9 years [2]. Hence, with increasing life expectancy, a modular system that is easier to revise should be considered in patients for whom a future revision might be required. However, modular prosthesis is generally more expensive compared to non-modular variants, so cost may be a concern for some patients. The results from our study stress on the importance of pre-operative planning in deciding the implant for hemiarthroplasties of the hip to avoid complications and suboptimal results. With the rise of personalized implants in orthopedic surgeries, the standard “one size fits all” prosthesis may soon be outdated. Ours was a single-center observational study. To validate the results, a multicentric randomized trial would be required.
With increasing rates of hemiarthroplasties and greater patient demands, choosing the optimal implant for each patient has never been more important. Our study is one of the very few studies comparing the surgical outcomes of the two most widely used implants for hip hemiarthroplasties. Without adequate pre-operative assessment, the monoblock prosthesis has a risk of over lengthening, difficult reduction, and intra-operative fractures, especially in patients with narrow femoral canals. In such patients, the modular system provides a greater advantage to choose an appropriate-sized prosthesis to avoid such complications.
Modular prosthesis for hemiarthroplasty could be superior to monoblock systems in fracture neck of femur with fewer complications such as limb lengthening and intra-operative fractures.
References
- 1.Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int 2004;15:897-902. [Google Scholar]
- 2.Avery PP, Baker RP, Walton MJ, Rooker JC, Squires B, Gargan MF, et al. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: A seven- to ten-year follow-up report of a prospective randomised controlled trial. J Bone Joint Surg Br 2011;93:1045-8. [Google Scholar]
- 3.NICE Clinical Guide Lines. The Management of Hip Fracture in Adults. National Clinical Guideline Centre (NICE) London: National Clinical Guideline Centre; 2011. Available from: ??? [Last accessed on 2023 Jan 06]. [Google Scholar]
- 4.Reddy AK, Scott JT, Norris GR, Moore C, Checketts JX, Hughes GK, et al. Cemented vs Uncemented hemiarthroplasties for femoral neck fractures: An overlapping systematic review and evidence appraisal. PLoS One 2023;18:e0281090. [Google Scholar]
- 5.Imam MA, Shehata M, Abdallah AR, Ahmed H, Kader N, Ernstbrunner L, et al. Unipolar versus bipolar hemiarthroplasty for displaced femoral neck fractures: A pooled analysis of 30,250 participants data. Injury 2019;50:1694-708. [Google Scholar]
- 6.Cash D, Bayer J, Logan K, Wimhurst J. The exeter trauma stem: Early results of a new cemented hemiarthroplasy for femoral neck fracture. Br J Med Pract 2020;3:303. [Google Scholar]
- 7.Woolson ST, Hartford JM, Sawyer A. Results of a method of leg-length equalization for patients undergoing primary total hip replacement. J Arthroplasty 1999;14:159-64. [Google Scholar]
- 8.Parker MJ. Cemented Thompson hemiarthroplasty versus cemented exeter trauma stem (ETS) hemiarthroplasty forintracapsular hip fractures: A randomised trial of 200 patients. Injury 2012;43:807-10. [Google Scholar]
- 9.Elmenshawy AF, Salem KH. Cemented versus cementless bipolar hemiarthroplasty for femoral neck fractures in the elderly. EFORT Open Rev 2021;6:380-6. [Google Scholar]
- 10.Looker AC, Melton LJ 3rd, Borrud LG, Shepherd JA. Changes in femur neck bone density in US adults between 1988–1994 and 2005–2008: Demographic patterns and possible determinants. Osteoporos Int 2012;23:771-80. [Google Scholar]
- 11.Hourston GJ, Patel J, McDonnell SM. Comparison of exeter stem offset size for total hip arthroplasty between males and females: A retrospective series of 780 hips. J Clin Orthop Trauma 2022;32:101966. [Google Scholar]







