Brodie’s abscess is a type of subacute osteomyelitis that can be easily missed and should be considered in any child presenting with limp and lower extremity pain when there is a lucency seen on imaging.
Dr. Barbara Minkowitz, Department of Orthopedics, Morristown Medical Center, 261 James Street, Suite 3C, Morristown, NJ 07960. E-mail: bminkowitz@aol.com
Introduction: Brodie’s abscess is one type of subacute osteomyelitis that can be difficult to diagnose because characteristic signs and symptoms can be subtle and non-specific. Up to 90% of Brodie’s abscess cases are initially misdiagnosed, with a mean delay of 3 months to the correct diagnosis, with 50% of them misdiagnosed as tumors. Other conditions can also present quite similarly.
Case Report: A 7-year-old male presented with complaints of hip pain and inability to bear weight. X-rays revealed Brodie’s abscess in the proximal femur which was initially misdiagnosed as toxic synovitis with an incidental unicameral bone cyst (UBC).
Conclusion: Brodie’s abscess can be a diagnosis that is easily missed and should be included in the differential diagnosis when a child presents with a limp, inability to bear weight, or when a cortical lucency is seen on X-ray. There are no other cases in the literature of Brodie’s abscess presenting like toxic synovitis. This case is relevant to pediatricians and orthopedists, particularly pediatric orthopedists.
Keywords: Brodie’s abscess, toxic synovitis, septic arthritis, unicameral bone cyst.
A subacute or chronic form of hematogenous osteomyelitis, Brodie’s abscess, is characterized by an encapsulated area of intraosseous abscess formation [1]. Subacute osteomyelitis can be difficult to diagnose because characteristic signs and symptoms of acute osteomyelitis such as fever, focal edema, warmth, or tenderness may be absent. Presentation is often insidious with variable presence of fever and mild pain. The metaphyses of long bones such as the distal tibia, proximal tibia, distal femur, proximal or distal fibula, and distal radius are the most common locations for occurrence [2]. Brodie’s abscess appears on X-ray as an oval or elliptical radiolucency, often greater than 1 cm. It can be surrounded by a reactive sclerotic border which is often scalloped on the radiograph [3]. Brodie’s abscess is best visualized using a computed tomography (CT) scan, although this imaging modality is less frequently used in children given its high cost and higher dose of radiation [4]. Brodie’s abscesses occur in males more frequently than females with a ratio of 2.1:1 [1]. In a study of 407 Brodie’s abscess cases, signs and symptoms consisted primarily of pain (98%) and/or swelling (53%). Eighty-four percent of the patients were afebrile, and <50% had elevated serum inflammatory markers. Diagnosis was made with a combination of imaging modalities: plain radiographs were sufficient in 96%, MRI in 16% and CT-scan in 8%. Treatment consisted of surgery in 94% of cases, in conjunction with long-term antibiotics in 77% of cases. Staphylococcus aureus was the most common pathogen isolated from cultures (67%). Recurrence was reported in 15% of the cases, which required further intervention [5]. In the treatment for the majority of Brodie’s abscess cases, surgery is performed. If the cavity is small, surgical evacuation and curettage are performed and antibiotics are administered. If the cavity is large and the bone is unstable, the abscess space may need packing and reinforcement with bone graft. Brodie’s abscess is a diagnosis that can be easily missed. A thorough history and physical, proper diagnostic imaging, laboratories, and high clinical suspicion are essential to avoiding misdiagnoses and delays in diagnosis.
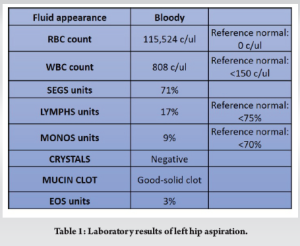
A 7-year-old previously healthy male presented to an outside emergency department (ED) with severe left hip pain and inability to bear weight after a wrestling injury. He reported a history of influenza 2 weeks prior, which was treated with Tamiflu and had resolution of flu symptoms. Radiographs of the pelvis identified a 2-cm oval lucency in the left femoral neck. Initial labs showed ESR 10 (s) and CRP 6 (mg/l) with WBC 10.6 (μl). Concern for septic arthritis was low in the setting of normal inflammatory markers. Given his recent history of influenza, the patient was discharged home with a diagnosis of toxic synovitis. He was advised to take NSAIDs and follow-up with an orthopedist for presumed toxic synovitis and with orthopedic oncology for evaluation of the lucency seen on X-ray. The patient returned to the ED 3 days later with continued inability to bear weight and severe pain which was not relieved by NSAIDs. Radiographs were repeated which showed widened joint space in the left hip and a well-defined lucency in the left femoral neck, presumed to be a unicameral bone cyst (UBC). A septic arthritis work-up was performed given the progression of symptoms and worsening pain. Repeat labs showed ESR 12(s), CRP 9 (mg/l), and WBC 13.3 (μl). The patient was sent for an ultrasound-guided hip aspiration with cell count, gram stain, and cultures. He had symptomatic relief after aspiration and was discharged with 1-week orthopedic follow-up. The hip aspirate results (Table 1) showed no white cells present on the gram stain, with no growth on the culture.
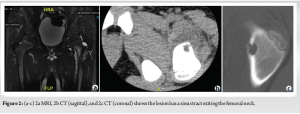
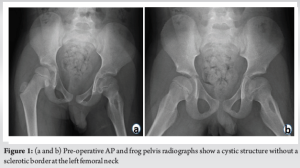
The treating physicians at the time did not suspect infection based on these studies and the patient was not started on empiric antibiotics. The patient continued with severe pain, so his parents sought a second opinion with the author of this paper. On examination, the patient was afebrile, refused to bear weight, and had severe pain with any attempted hip range of motion. New pelvis radiographs were taken that showed a cystic structure without a sclerotic border at the left femoral neck (Fig. 1a and b). The patient was referred to the ED for repeat labs and MRI with and without contrast. At this time, the differential diagnosis included a tumor, infection, and a pathologic fracture. The MRI results were inconclusive (Fig. 2a) in differentiating between tumor versus infection. Findings were not consistent with UBC or pathologic fracture. A CT without contrast showed the lesion had a sinus tract exiting the femoral neck (Fig. 2b and c) and the patient was diagnosed with a Brodie’s abscess.
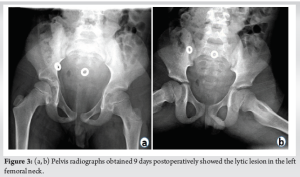
He was brought to the operating room for debridement of the abscess and joint arthrotomy. A c-arm was used intraoperatively to identify the location of the abscess and it was possible to feel the space when the curette entered the abscess. The bone lesion was curetted, antibiotics lavage was performed, and a wound vacuum was placed. Aerobic, anaerobic, fungal, and mycobacterial cultures obtained from the bone in addition to a broad range bacterial polymerase chain reaction (run in Mayo Laboratory, Rochester, MN) were all negative. Bacterial culture from hip joint fluid was also negative. Histopathology of synovial tissue showed benign fibroconnective tissue with mild chronic inflammation; no bone was seen in the specimen. Two days postoperatively, the wound vacuum was removed, a repeat intraoperative washout with antibiotics was preformed, and the wound was closed. He was treated with intravenous clindamycin for 6 days and discharged on oral clindamycin. Clindamycin monotherapy was chosen to achieve coverage against MRSA, effectively treat S. aureus, the most common cause of osteomyelitis in the patient’s age group, and allow for an easy transition to oral antibiotics. Given focal infection and no signs of sepsis, clindamycin was an appropriate antibiotic choice. In total, the patient completed a 3-month course of clindamycin. One week postoperatively, he had a full hip range of motion, was fully weight-bearing with a slight limp, and had resolution of pain. Radiographs (Fig. 3a and b) obtained 9 days postoperatively showed the lytic lesion in the left femoral neck after debridement. At 2-week post-operative, the patient’s limp had fully resolved, and he began strengthening exercises.
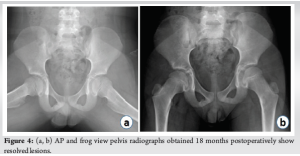
At 6-month follow-up, he had no clinical complaints but the lesion was still seen on radiographs, so an MRI was obtained to further assess the lesion and determine the need for bone grafting. MRI revealed a 2-cm cyst on the anterior femur < 50% diameter of the bone, therefore not increased concern for the structural integrity of the femur. At 1-year follow-up, two view pelvis X-rays were taken showing a resolving cyst in the anterior left femur which appeared smaller than previous X-rays. At an 18-month follow-up, the patient had a full range of motion, no pain, and had resumed full activities with no restrictions. At this time, two-view pelvis X-rays showed a resolved cyst (Fig. 4a and b). This patient will be followed annually until he reaches skeletal maturity.
The 7-year-old patient with a Brodie’s abscess in the proximal femur was initially misdiagnosed as having toxic synovitis with an incidental unicameral bone cyst. This led to a delayed diagnosis, multiple emergency room visits, and numerous diagnostic imaging studies.
The first diagnostic error was made on the radiograph review. Cysts and abscesses can appear very similarly on radiographs but usually have slight differences. UBCs are well-defined lucent lesions with sclerotic borders, mostly found in skeletally immature patients. They frequently occur as a solitary lesion at the end of the bone, near a growth plate. An abscess in the bone usually causes a purely lytic lesion. However, this is not always true, as there are cases of Brodie’s abscess where cortication is formed slowly over time and may be seen on radiographs [5]. UBCs are not painful and are found incidentally unless there is pain from a resulting pathologic fracture which can occur due to weakness in the bone at the site of the UBC. They tend to be found with a male-to-female ratio of 3:1. UBCs make up only 3% of primary bone lesions, with over 30% of these occurring in the proximal femur [6]. While a cyst is a fluid-filled space enclosed by distinct abnormal cells, an abscess is a space caused by bacteria or fungi. Cysts grow slowly and abscesses, like Brodie’s, grow much faster. When an intracortical bone lesion is seen on a radiograph, the differential should include Brodie’s abscess, osteoid osteoma, osteoblastoma, and intracortical hemangioma [2]. Additional imaging is necessary to definitively diagnose a bone lesion [4]. It was an oversight in this case to assume that the bone lesion was simply an incidental finding. The clinician should have followed Occam’s razor by searching for the solution using the smallest possible set of variables and considered that the lesion was the source of the patient’s pain rather than an incidental finding. The prevalence of both toxic synovitis and UBCs is greater than Brodie’s abscesses; however, the likelihood of these two conditions happening simultaneously seems very low.
Toxic synovitis occurs when there is inflammation in the hip joint causing pain and is most commonly seen after a viral infection. Toxic synovitis usually responds to NSAIDs and is associated with antalgic gait or refusal to walk, complaints of thigh or knee pain, low-grade fever, and crying or irritability in younger children [7].
Although initial concern for septic arthritis was low in this patient with normal inflammatory markers and negative cultures, he was ultimately treated similarly to a patient with septic arthritis with hip I&D and antibiotics. “Textbook” septic arthritis is caused by the hematogenous spread of bacteria into the joint space leading to joint pain, limping, and refusal to bear weight. When there is an infection in the proximal femur, the assumption should be that the hip joint is involved until proven otherwise. This is because the proximal femur is contiguous with the hip joint; fluid will drain into the joint space before, and instead of, forming a subperiosteal abscess. The effusion represents a septic hip. The incidence in developed countries is 4–5 cases per 100,000 children/year [8]. The Kocher criteria can be used to predict septic arthritis and criteria include: Non-weight-bearing on the affected side, erythrocyte sedimentation rate > 40, fever > 38.5°C, white blood cell count > 12,000. This patient had one predictor (non-weight-bearing) which has a 9.5% predicted probability of septic arthritis [9, 10].
Laboratory and microbiologic studies can sometimes help differentiate between infection, tumors, and cysts. Over 25% of documented Brodie’s cases did not have an organism recovered on culture [5]. Studies such as ESR, CRP, and CBC can help support one diagnosis over another; however, these are not definitive. An inconclusive interpretation of laboratory studies in this case may have led to delayed diagnosis. There can be a much lower white count in the serum and joint fluid despite the possible presence of infection. It remains unclear if the patient did have an infection in the hip or if the elevated white blood cell count was reactive due to Brodie’s abscess. A table written by Horowitz et al., in 2010, nicely illustrates the differential diagnoses to consider based on interpretation of intra-articular fluid lab values (Table 2) [11]. This patient had a low WBC (808 c/ul) level in the joint aspirate and the serum, placing him in the non-inflammatory arthritis category.
Treatment of Brodie’s abscess includes surgery, antibiotics, and continued monitoring of pain. Patients diagnosed with Brodie’s should be followed until full skeletal maturity. If pain arises with another lesion elsewhere in the body, or the patient does not respond to surgery and antibiotics in the setting of negative microbiologic studies, other etiologies such as chronic recurrent multifocal osteomyelitis (CRMO) or chronic nonbacterial osteomyelitis (CNO) should be considered.
This case demonstrates the challenges in the diagnosis of Brodie’s abscess with initial misdiagnosis, prolonged work-up, and multiple ED visits. Laboratory studies may be misleading and can contribute to delayed diagnosis. Brodie’s abscess should be considered in the differential diagnosis of any child presenting with limp and lower extremity pain when there is a lucency seen on X-ray or other imaging.
Brodie’s abscess should be considered in any child presenting with limp and lower extremity pain when there is a lucency seen on X-ray or other imaging.
References
- 1.Foster CE, Taylor M, Schallert EK, Rosenfeld S, King KY. Brodie abscess in children: A 10-year single institution retrospective review. Pediatr Infect Dis J 2019;38:e32-4. [Google Scholar]
- 2.Alex A. (n.d.). Osteomyelitis - Pediatric. Available from: https://www.orthobullets.com/pediatrics/4031/osteomyelitis--pediatric, Accessed 12/15/22. [Google Scholar]
- 3.Agrawal P, Sobti A. A brodies abscess of femoral neck mimicking Osteoid osteoma: Diagnostic approach and management strategy. Ethiop J Health Sci 2016;26:81-4. [Google Scholar]
- 4.Moser T, Ehlinger M, Bouaziz MC, Ladeb MF, Durckel J, Dosch JC. Pitfalls in osteoarticular imaging: How to distinguish bone infection from tumour? Diagn Interv Imaging 2012;93:351-9. [Google Scholar]
- 5.Naald NV, Smeeing DP, Houwert RM, Hietbrink F, Govaert GA, Velde DV. Brodies abscess: A systematic review of reported cases. J Bone Jt Infect 2019;4:33-9. [Google Scholar]
- 6.Sobeai MA, Hussein I, Shetty S. (n.d.). Unicameral Bone Cyst. Available from: https://www.orthobullets.com/pathology/8035/unicameral-bone-cyst, Accessed 12/15/22. [Google Scholar]
- 7.Swarup I, Lavalva S, Shah R, Sankar WN. Septic arthritis of the hip in children. JBJS Rev 2020;8:e0103. [Google Scholar]
- 8.Krogstad P. Osteomyelitis and septic arthritis. In: Feigin RD, Cherry JD, editors. Textbook of Pediatric Infectious Diseases. 6th ed. Philadelphia, PA: Saunders; 2009. p. 725-48. [Google Scholar]
- 9.Kocher MS, Mandiga R, Zurakowski D, Barnewolt C, Kasser JR. Validation of a clinical prediction rule for the differentiation between septic arthritis and transient synovitis of the hip in children. J Bone Joint Surg Am 2004;86:1629-35. [Google Scholar]
- 10.Kocher MS, Zurakowski D, Kasser JR. Differentiating between septic arthritis and transient synovitis of the hip in children: An evidence-based clinical prediction algorithm. J Bone Joint Surg Am 1999;81:1662-70. [Google Scholar]
- 11.Horowitz DL, Katzap E, Horowitz S, Barilla-LaBarca ML. Approach to septic arthritis. Am Fam Physician 2011;84:653-60. [Google Scholar]