If pain recurs after a first episode of subchondral insufficiency fracture (SIF) of the femoral head, it should be kept in mind not to overlook the possibility of a recurrent SIF.
Dr. Koichi Kinoshita, Department of Orthopedic Surgery, Fukuoka University, Faculty of Medicine, 7-45-1 Nanakuma, Jonan-ku, Fukuoka 814-0180, Japan. E-mail: kinopfukuoka@yahoo.co.jp
Introduction: Subchondral insufficiency fracture (SIF) of the femoral head has been reported to occur in older women with osteoporosis. No cases with recurrence of SIF at another site in the ipsilateral femoral head have been described.
Case Report: We report a case of a 75-year-old woman with recurrent SIF at another site in the ipsilateral femoral head. SIF was first observed at an anterolateral site on the femoral head and treated non-operatively. The hip pain disappeared after 3 months but recurred 5 months later when another SIF was newly observed at a posterolateral-to-medial site on the femoral head. This SIF was also treated non-operatively. Five months later, the pain was alleviated, but progression of osteoarthritis was seen on X-rays.
Conclusion: After an initial SIF, the possibility of recurrence should be considered if pain recurs, even on the ipsilateral side.
Keywords: Recurrence, subchondral insufficiency fracture, ipsilateral femoral head.
Subchondral insufficiency fracture (SIF) of the femoral head has been reported to occur in older women with osteoporosis [1, 2]. In a few cases, SIF was reported to occur in young people and after renal transplantation [3-6]. Regarding treatment, non-operative treatments were reported to be effective in some cases [3, 5, 6]. Bilateral SIF has been reported in three cases [5, 6]. However, no cases with recurrence of SIF at another site in the ipsilateral femoral head have been described. Herein, we report a case of SIF recurrence at a different site in the same femoral head after an interval of 5 months.
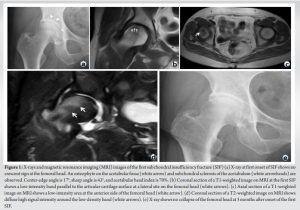
A 75-year-old woman presented to an orthopedic clinic with right hip pain caused by a misstep. Her height was 156 cm and her body weight was 63 kg, giving a body mass index of 25 kg/m2. She had no history of steroid treatment or alcohol consumption. On X-ray examination, an osteophyte on the acetabular fossa and subchondral sclerosis of the acetabulum were observed (Fig. 1a), but a crescent sign and collapse of the femoral head were not seen. A center-edge angle of 17°, a sharp angle of 43°, and an acetabular head index of 70% were noted. The patient was diagnosed with acetabular dysplasia for the first time. T1-weighted images on magnetic resonance imaging (MRI) revealed a low-intensity band parallel to the articular cartilage at an anterolateral site on the right femoral head (Fig. 1b and c). The length of the low-intensity band was 11 mm, and the band ratio (ratio of weight-bearing portion length to band length) [7] was 35%. A T2-weighted image on MRI showed diffuse high signal intensity around the low-intensity band (Fig. 1d). The bone mineral density (BMD) was not measured at this time. The patient was diagnosed with SIF involving bone marrow edema based on previously reported diagnostic criteria [8, 9]. The patient was treated non-operatively, including the administration of NSAIDs, and was allowed to walk according to the degree of pain. The pain disappeared 3 months after the onset (Fig. 1E). Subsequently, the patient experienced ipsilateral hip pain while lifting her husband during nursing care, 5 months after disappearance of the first hip pain. X-ray examination revealed a 1-mm collapse at a lateral site on the femoral head and osteophyte formation at the lateral head-neck junction of the femoral head (Fig. 2a). The osteophyte on the acetabular fossa and subchondral sclerosis of the acetabulum were more clearly observed on the X-ray, and the minimum joint space was 1 mm narrower than that observed 5 months previously (Fig. 1e).
The progression of osteoarthritis was observed. T1-weighted images on MRI showed a new low-intensity band at a posterolateral-to-medial site on the femoral head (Fig. 2b and c). The length of the low-intensity band was 10 mm, and the band ratio [7] was 32%. A T2-weighted image on MRI showed diffuse high signal intensity around the low-intensity band (Fig. 2d). The high signal intensity area revealed in the first SIF had disappeared in the second SIF. The patient was diagnosed with a recurrence of SIF at a different sites on the ipsilateral femoral head from the first SIF. Osteoporosis was also diagnosed after dual X-ray absorptiometry demonstrated a BMD of 0.675 g/cm2 (T-score: −1.0) in the right femoral head and a total BMD of 0.792 g/cm2 (T-score: −1.8) in the lumbar spine (L1–L4). Administration of teriparatide was prescribed for the second SIF. The patient was treated non-operatively and was allowed to walk with a T-cane according to the degree of pain. At 5 months after the onset of the second SIF, the pain had gradually alleviated but was still present (Fig. 2e). In particular, walking pain remained, but the patient was able to walk with a T-cane. An X-ray showed progression of osteoarthritis of the hip at 3 years after the first SIF onset (Fig. 2f).
SIF has been reported to occur in older women with osteoporosis and patients with organ transplantation [1, 2, 4, 10]. Bilateral SIF in patients who underwent renal transplantation was also reported [5, 6]. However, there are no reports of recurrence of SIF at another site in the ipsilateral femoral head. The reason for recurrence at another site may be related to the position of the injured limb. Bachtar et al. [11] reported that load stress was concentrated at an anterior site on the femoral head during walking, based on a patient-specific finite element analysis. At the first SIF onset, the patient missed her step during walking, and the load stress may have been concentrated at an anterior site on the femoral head, leading to a fracture at the anterior site. Meanwhile, Anderson et al. [12] reported that load stress was concentrated at a posterior site on the femoral head during hip flexion and internal rotation. At the second onset, the patient had hip flexion and internal rotation when lifting her husband and the load stress may have been concentrated at a posterior site on the femoral head, causing a fracture at the posterior site. Iwasaki et al. [7] reported that the length of the low-density band on a T1-weighted image on MRI, namely the length of the fracture line, and its ratio to the length of the weight-bearing portion (band ratio) were important factors for predicting collapse of the femoral head. If the band ratio was ≥57.9% or less, conservative treatment was considered effective [13]. Owing to the short fracture line and small band ratio in the present patient, non-operative treatment may have resulted in bone union after the first episode of SIF. Although bone union was also observed after the second episode of SIF and there was no progressive collapse of the femoral head, osteoarthritis of the hip had progressed. Specifically, the X-ray examination at the onset of the second SIF revealed that osteoarthritis had progressed compared with the X-ray examination after the healing of the first SIF. As the first SIF had healed and a collapse of the femoral head was very slight, the joint space was not usually narrowed. Progressive osteoarthritis may have occurred through acetabular dysplasia. Yamamoto et al. [14] reported that the prevalence of SIF in cases with a pre-operative clinical diagnosis of osteoarthritis was 6.3% (460 of 7349 cases). SIF may be involved in the progression of osteoarthritis, requiring surgical treatment. In our case, osteoarthritis may have progressed as a result of SIF overlapping with progressive osteoarthritis with acetabular dysplasia. Iwasaki et al. [15] reported that the most common site of SIF was an anterior site on the femoral head. They classified SIF into lateral type and central type and found that lateral type was predominant in patients with acetabular dysplasia of the hip and represented a poor prognostic factor. The present patient had a lateral-type SIF and also had acetabular dysplasia of the hip, consistent with their report.
We provide the first case report of recurrent SIF at another site in the ipsilateral femoral head. The reason for recurrence at another site may be related to the position of the injured limb. After a first episode of SIF, the possibility of recurrence should be kept in mind if pain recurs, even on the ipsilateral side.
If pain recurs after the first episode of SIF, it may be diagnosed as resulting from the same site. It should be kept in mind not to overlook the possibility of a recurrent SIF.
References
- 1.Rafii M, Mitnick H, Klug J, Firooznia H. Insufficiency fracture of the femoral head: MR imaging in three patients. AJR Am J Roentgenol 1997;168:159-63. [Google Scholar]
- 2.Yamamoto T, Bullough PG. Subchondral insufficiency fracture of the femoral head: A differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum 1999;42:2719-23. [Google Scholar]
- 3.Visuri T. Stress osteopathy of the femoral head. 10 military recruits followed for 5-11 years. Acta Orthop Scand 1997;68:138-41. [Google Scholar]
- 4.Vande Berg BC, Malghem J, Goffin EJ, Duprez TP, Maldague BE. Transient epiphyseal lesions in renal transplant recipients: Presumed insufficiency stress fractures. Radiology 1994;191:403-7. [Google Scholar]
- 5.Ikemura S, Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Iwamoto Y. Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: A case report. Arthritis Rheum 2005;52:1293-6. [Google Scholar]
- 6.Ohtsuru T, Yamamoto T, Murata Y, Morita Y, Munakata Y, Kato Y. Bilateral subchondral insufficiency fractures of the femoral head in patients with living renal transplantation: A report of two cases. J Orthop Sci 2017;22:972-5. [Google Scholar]
- 7.Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Mawatari T, Nakashima Y, et al. Prognostic factors associated with a subchondral insufficiency fracture of the femoral head. Br J Radiol 2012;85:214-8. [Google Scholar]
- 8.Yamamoto T, Schneider R, Bullough PG. Insufficiency subchondral fracture of the femoral head. Am J Surg Pathol 2000;24:464-8. [Google Scholar]
- 9.Miyanishi K, Hara T, Kaminomachi S, Maeda H, Watanabe H, Torisu T. Contrast-enhanced MR imaging of subchondral insufficiency fracture of the femoral head: A preliminary comparison with that of osteonecrosis of the femoral head. Arch Orthop Trauma Surg 2009;129:583-9. [Google Scholar]
- 10.Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: Histopathologic correlation with MRI. Skeletal Radiol 2001;30:247-54. [Google Scholar]
- 11.Bachtar F, Chen X, Hisada T. Finite element contact analysis of the hip joint. Med Biol Eng Comput 2006;44:643-51. [Google Scholar]
- 12.Anderson AE, Ellis BJ, Maas SA, Peters CL, Weiss JA. Validation of finite element predictions of cartilage contact pressure in the human hip joint. J Biomech Eng 2008;130:051008. [Google Scholar]
- 13.Iwasaki K, Yamamoto T, Motomura G, Ikemura S, Yamaguchi R, Iwamoto Y. Radiologic measurements associated with the prognosis and need for surgery in patients with subchondral insufficiency fractures of the femoral head. AJR Am J Roentgenol 2013;201:W97-103. [Google Scholar]
- 14.Yamamoto T, Iwamoto Y, Schneider R, Bullough PG. Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis 2008;67:150-3. [Google Scholar]
- 15.Iwasaki K, Yamamoto T, Motomura G, Karasuyama K, Sonoda K, Kubo Y, et al. Common site of subchondral insufficiency fractures of the femoral head based on three-dimensional magnetic resonance imaging. Skeletal Radiol 2016;45:105-13. [Google Scholar]