The purpose of this case report is to present exceptionally rare presentation of vertebral body osteochondroma and its management.
Dr. Kaman Kuity, Department of Orthopaedic Surgery, Dr. D. Y. Patil Medical College, Hospital and Research Centre, Pimpri, Pune - 411018, Maharashtra, India. E-mail: Kamaniimsar11@gmail.com
Introduction: Vertebral body osteochondroma presenting with myelopathic symptoms is exceptionally rare entity of spinal osteochondroma which arises from the posterior surface of vertebral body and leading to spinal canal stenosis and cord compression. Early definitive diagnosis and subsequent successful treatment is necessary in such cases to prevent life threatening complications.
Case Report: In this context, we report a case of a 20-years old female presented with mechanical neck pain, unsteady gait, giddiness with neurological deficit for the past 3 months. An MRI of the cervical spine revealed a mass growing from the posterior aspect of the C6 vertebral body and extending toward the vertebral canal, causing marked spinal cord compression.
Conclusion: The following case report not only describes the rare presentations of vertebral body osteochondroma but also emphasizes on surgical management by en bloc resection of tumor and anterior cervical fusion, resulting in a favorable outcome without any recurrence.
Keywords: Vertebral body osteochondroma, corpectomy, en bloc excision, cervical fusion
Myelopathic symptoms due to cervical vertebral body osteochondroma are an extremely rare presentation of spinal osteochondroma. The prevalence of spinal osteochondroma has been reported 3% in solitary forms and 7-9% in multiple appearances associated with hereditary multiple exostosis [1]. Spinal osteochondroma usually arises from posterior elements of spine like posterior arch (other than the lamina, pedicle, and spinous process) followed by lamina [2], whereas vertebral body osteochondroma is significantly rare. Earlier data shows that osteochondroma arises from the cervical vertebral body growing away from the spinal cord [3]. However, we report an exceptionally rare case of C6 vertebral body osteochondroma presenting with myelopathic symptoms and neurodeficits due to spinal cord compression, which was successfully managed by Corpectomy and En bloc excision of the tumor followed by cervical fusion through anterior approach. Early diagnosis and prompt surgical management is necessary in such cases, otherwise it may leads to life threatening complications.
A 20-year old female appeared with neck pain and progressive weakness of bilateral upper limbs for the past 3 months. The pain was insidious onset, progressively worsening, and radiating to bilateral upper limb. She was also suffering from unsteady gait, giddiness, and difficulty in walking. There had been no history of recent trauma before the onset of symptoms, no history of any constitutional symptoms. She had no history of medical and surgical intervention before the onset of symptoms.
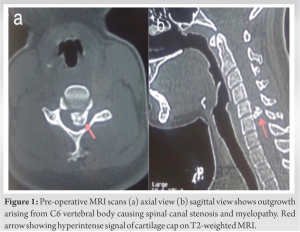
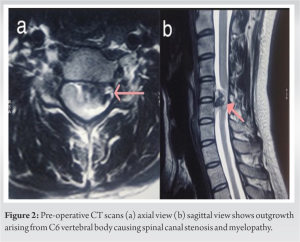
On examination, neck flexion was painful, restricted, and decreased sensation over lateral aspect of right arm and forearm. Hoffmann’s sign was positive and supinator reflex was inverted. Biceps and triceps power of both upper limbs were MRC grade 3 and handgrip was weak. Spasticity and MRC grade 4 power were elicited in bilateral lower limbs. Deep tendon reflexes of both lower limbs were exaggerated with bilateral ankle clonus. Babinski sign was positive and supinator reflex was inverted. The patient also had multiple exostoses around the knee, pelvis, and scapula. There was no case of MHE reported in the family. Plain cervical spine radiography (AP and lateral view) revealed a lytic lesion on the C6 vertebral body but could not show complete details. Axial and sagittal view of MRI cervical spine (Fig. 1) revealed mass growing from the posterior aspect of the C6 vertebral body (left side) with 1.2 cm cartilage cap and extend toward the vertebral canal leads to marked spinal cord compression and CT scans (Fig. 2) revealed bony overgrowth arising from left C6 vertebral body extended superiorly into the spinal canal.
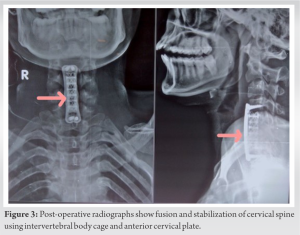
En bloc excision and cervical fusion through anterior approach was planned after complete pre-operative work up. The procedure was done in supine position under general anesthesia. A 6 cm horizontal incision was made over a front of neck. After platysma transection, sternocleidomastoid was divided. Trachea, esophagus retracted medially and carotid sheath retracted laterally to expose vertebral body. C4 to C7 vertebral bodies were identified. C4-C5 and C6-C7 discectomy were performed before corpectomy. C5, C6 corpectomy was performed by utilizing burr, osteotome, curettes and the tumor underwent en bloc excision during corpectomy. Reconstruction was done using an intervertebral body mesh cage and bone graft. Remove cartilage from either endplates before cage placement for stable fusion. Anterior cervical plate and screws were used to stabilize the cervical vertebra (Fig. 3).
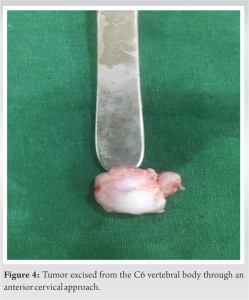
The surgery lasted 4 hours with a minimal blood loss of 200 ml. The excised mass was sent for histopathological examination, in which it was confirmed to be a benign osteochondroma without malignant changes (Fig. 4). The perioperative period was uneventful without any significant complications. The patient started walking on post-operative day two with disappearance of neurological symptoms and complete recovery of power and reduction in spasticity were observed within 20 days. The patient’s reflexes became normal after 1 month of the surgery. At 2-year follow-up, MRI and CT scans showed no evidence of recurrence.
Osteochondroma (exostosis) is a benign cartilaginous tumor derived from abnormal subperiosteal physeal cartilage that matures according to normal enchondral ossification, constituting 20-50% of all benign bone neoplasms [4]. Young adult males are most predominantly affected, accounting for 70% of patients. The lesions mostly affect metaphyseal region of long bones, such as the distal femur, proximal tibia, and humerus [5]. Spinal osteochondroma is an extremely rare entity (<3% of all osteochondroma) whereas, the cervical spine is the most commonly affected level among all spinal osteochondromas [2]. The proposed mechanism of cervical osteochondroma is a cervical spine mobility-induced stress could lead to repetitive micro-trauma and cartilage displacement, with subsequent formation of osteochondroma [6]. Exostosis generally involves posterior elements of spine such as posterior arch, lamina, pedicle, and spinous process [2]. Our case describes a osteochondroma arising from the posterior surface of vertebral body which is significantly rare in literature. Very few cases of cervical osteochondroma arising from the anterior column of the spine have been reported. Grivas et al. in 2005 [7], Wang and Chou, Reckelhoff et al. in 2010, [8] and Certo et al. in 2014 [3] reported 18 cases of exostosis rising from the anterior column (anterior surface of cervical vertebral bodies) growing away from the spinal cord, with dysphagia, hoarseness of voice, and neck pain as chief complaints [3,7,8]. Spinal osteochondroma rarely causes any neurological symptoms as the majority of the tumors arise from the posterior column grow away from the spinal cord [9]. Neck pain radiating to the upper limbs, motor, and sensory neurodeficits are the most prevalent symptoms of intracanal extension of osteochondroma. Our case describes a unique presentation of C6 vertebral body osteochondroma: Spinal canal stenosis and myelopathy with neurological deficits, which is an exceptionally rare presentation. Complications of cervical spine osteochondroma are rare, including pathological fracture of vertebra, sudden death due to subtotal spinal cord compression, Brown-Sequard syndrome [8]. The incidence of malignant transformation among solitary osteochondroma is <3% [4]. Any breach in the perichondrium of lesion raises the suspicion of malignancy. A retained cartilaginous cap after skeletal maturation may be a risk for the development of chondrosarcoma. Hence, assessing the change in the size of the cartilaginous part of the tumor is crucial in cases of osteochondroma [10]. Thus, MRI and non-contrast CT scan are the investigations of choice for the detailed diagnostic assessment in cases of osteochondromas [5]. In this case, MRI and CT scans showed no evidence of malignant transformation. The management of spinal osteochondroma should begin with a history and clinical examination to rule out any neurovascular compromise. Most of the lesions are benign and painless, which can be managed by observation with occasional radiographic surveillance [6]. Osteochondromas associated with neurological sequelae such as radiculopathy, myelopathic symptoms, vascular compression, or unrelenting pain require surgical management [3]. Complete surgical resection of the tumor along with the cartilaginous part is the treatment of choice in cases of symptomatic cervical osteochondroma. Depending on the location of the tumor, the approach can be either anterior or posterior. Nerve root decompression with instrumented stabilization of vertebra with or without fusion is most effective treatment in some cases. Complete resection of the cartilaginous part of the tumor is the most important step to prevent recurrence [5]. In cases of incomplete resection, there is a 2-5% chance of recurrence of the lesion and after complete resection, recurrence is <2% [6, 11]. As per surgical management of spinal osteochondroma, the patient underwent through corpectomy, en bloc excision of mass, and cervical fusion with cervical plate, screws, intervertebral body cage. The patient had a complete recovery from the pre-operative symptoms with no complications or recurrence in a follow-up of 2 years. Complete resection of osteochondroma with cervical fusion looks like most reliable management of cervical osteochondroma with no major complication and good functional outcome.
Myelopathic symptoms such as unsteady gait, positive Hoffman sign, and exaggerated deep tendon reflexes are extremely rare presentation of vertebral body osteochondroma, making the diagnosis challenging. Early recognition and appropriate surgical technique are crucial to improving functional outcome and reducing recurrence. Surgical intervention consists of corpectomy, followed by en bloc excision of the tumor, reconstruction, and instrumented stabilization of cervical vertebrae through anterior approach is the treatment of choice in such cases.
Myelopathic symptoms due to vertebral body osteochondroma are exceptionally rare and challenging condition. Corpectomy with a combination of en bloc excision and instrumented stabilization through anterior approach provide excellent functional outcome without any recurrence.
References
- 1.Joshi G, Bhatta OP, Chand H, Mudbhari B, Dangol N, Bhetwal P. A solitary osteochondroma of the sixth cervical spine: A case report. Int J Surg Case Rep 2023;110:108729. [Google Scholar]
- 2.Yakkanti R, Onyekwelu I, Carreon LY, Dimar JR 2nd. Solitary osteochondroma of the spine-A case series: Review of solitary osteochondroma with myelopathic symptoms. Global Spine J 2018;8:323-39. [Google Scholar]
- 3.Certo F, Sciacca G, Caltabiano R, Albanese G, Borderi A, Albanese V, et al. Anterior, extracanalar, cervical spine osteochondroma associated with DISH: Description of a very rare tumor causing bilateral vocal cord paralysis, laryngeal compression and dysphagia. Case report and review of the literature. Eur Rev Med Pharmacol Sci 2014;18 1 Suppl:34-40. [Google Scholar]
- 4.Albrecht S, Crutchfield JS, SeGall GK. On spinal osteochondromas. J Neurosurg 1992;77:247-52. [Google Scholar]
- 5.Prasad A, Renjen PN, Prasad ML, Bhatty GB, Madan VS, Buxi TB, et al. Solitary spinal osteochondroma causing neural syndromes. Paraplegia 1992;30:678-80. [Google Scholar]
- 6.Fowler J, Takayanagi A, Fiani B, Cathel A, Sarhadi KJ, Arshad M, et al. Diagnosis, management, and treatment options: A cervical spine osteochondroma meta-analysis. World Neurosurg 2021;149:215-25.e6. [Google Scholar]
- 7.Grivas TB, Polyzois VD, Xarchas K, Liapi G, Korres D. Seventh cervical vertebral body solitary osteochondroma. Report of a case and review of the literature. Eur Spine J 2005;14:795-8. [Google Scholar]
- 8.Reckelhoff KE, Green MN, Kettner NW. Cervical spine osteochondroma: Rare presentation of a common lesion. J Manipulative Physiol Ther 2010;33:711-5. [Google Scholar]
- 9.Lotfinia I, Vahedi A, Aeinfar K, Tubbs RS, Vahedi P. Cervical osteochondroma with neurological symptoms: Literature review and a case report. Spinal Cord Ser Cases 2017;3:16038. [Google Scholar]
- 10.Murphey MD, Choi JJ, Kransdorf MJ, Flemming DJ, Gannon FH. Imaging of osteochondroma: Variants and complications with radiologic-pathologic correlation. Radiographics 2000;20:1407-34. [Google Scholar]
- 11.Tepelenis K, Papathanakos G, Kitsouli A, Troupis T, Barbouti A, Vlachos K, et al. Osteochondromas: An updated review of epidemiology, pathogenesis, clinical presentation, radiological features and treatment options. In Vivo 2021;35:681-91. [Google Scholar]