Early recognition and comprehensive treatment are essential for managing low-impact Schenck type IV knee dislocations and preventing severe complications.
Prof. Dr. Christian Heiss, Department of Trauma, Hand and Reconstructive Surgery, University Hospital Giessen, Rudolf-Buchheim-Str. 7, 35392 Giessen, Germany. E-mail: Christian.Heiss@chiru.med.uni-giessen.de
Introduction: Dislocations of the knee joint represent very rare injuries in the literature, accounting for less than 0.02% of all musculoskeletal injuries.
Case report: This report describes a patient suffered a knee joint dislocation of the knee joint caused by a low impact injury following a stumbling trauma during volunteer of a sport competition. Anterior knee joint dislocation with incipient compartment syndrome was clinically prognosed. Vascular and nerve injuries were radiologically examined. Taken together the injury was classified as Schenck type IV CN, and surgical management of the current knowledge was pursued. A satisfying range of motion was examined during surgery next to solid vascular und nerve conditions post-surgery.
Conclusion: In case of severe knee joint dislocations, the current standard of a closed reduction with subsequent diagnostic is recommended. Compartment syndrome, nerve, and vascular tears indicate emergency surgery.
Keywords:Knee dislocation, compartment syndrome, knee joint, dislocation, trauma surgery, tibiofemoral dislocation.
Dislocations of the knee joint account for less than 0.02% of all musculoskeletal injuries [1,2]. Concomitant injuries accompanies knee joint dislocation, such as vascular (5%) and nerve (19%) tears, ruptures of the posterior (PCL, 51%) and anterior (ACL, 19%) cruciate ligament and ruptures of the medial (MCL, 46%) and lateral (LCL, 84%) collateral ligament are mentioned [1,3,4]. However, severe musculoskeletal injuries might occur in exceptional cases [1,3]. Intriguingly, 33% of low-impact injuries result in knee joint dislocation [1,5,6]. The Schenck classification subdivides knee joint dislocations on the basis of concomitant injuries [7]. Current literature described only few cases of Schenck IV injuries with acute compartment syndrome [8]. More commonly, compartment syndrome is observed as a complication after knee joint dislocation [9]. To the best of the authors knowledge less cases reported of anterior knee dislocation with low impact are reported in PubMed using the search keywords “anterior knee dislocation, low impact” [5,9].
A 33-year-old male with a slightly overweight body mass index (26.3 kg/m2) and no known comorbidities was presented to the emergency department with a deformity and swelling of the lower left leg with any pucker sign. Being a volunteer during a long jump competition, the patient twisted his knee joint while upon impact in the sand-filed landing area. Initial examination, including palpation revealed a cold sensation on the foot, while the posterior tibial artery and dorsalis pedis artery were not palpable with simultaneous swelling of the knee joint and upper part of lower leg. A radiograph after failed closed injury reduction at the primary care hospital demonstrated an anterior knee dislocation (Fig. 1). Unfortunately, realizing this emergency situation there was neither clinical picture taken.
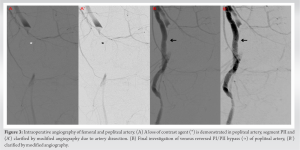
CT angiography (CTA) showed signal loss in the popliteal artery (Fig. 2).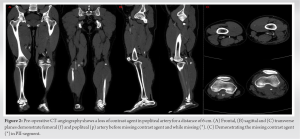
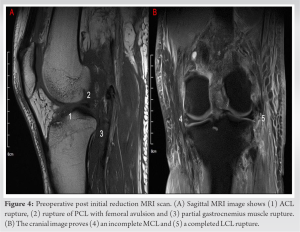
Postoperative magnetic resonance imaging (MRI) diagnosis revealed a multiligamentous injury (Fig. 4). Both cruciate ligaments were affected: the ACL showed a complete rupture, the PCL a femoral avulsion fracture. In addition, both collateral ligaments were injured: the LCL demonstrated a complete the MCL an incomplete rupture. The gastrocnemius muscle revealed a bundle tear. The medial meniscus showed a decent degeneration. In addition, a hemorrhagic joint effusion was present.
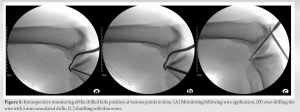
10 days after trauma, remaining ligamentous portions were preserved by reinforcing the distal PCL tendon and the tibial ACL stump. Furthermore, neurolysis of peroneal nerve, refixation of the biceps femoris, and debridement with subsequent vacuum assisted closure (VAC) therapy. Due to medial arthrotomy femoral avulsion PCL rupture, intra-ligamentous ACL rupture, partial rupture of the MCL, complete rupture of the LCL and a femoral biceps rupture were noticed. Attaching the cruciate ligament ruptures, ligamentous remain ligamentous structures were armored. For PCL reconstruction, drill holes were performed for reattaching the avulsion fracture without necessarily of augmentation due to robust ligamentous structure. ACL was reconstructed by wire application, over-drilling using a 5 mm cannulated drill and introducing a wire for shuttling at the anatomical footprint controlled radiological (Fig. 5). After being prepared, PCL armored threads, were fixed femoral using suture discs (Tight Rope®, Arthrex, Florida, USA). ACL augmentation was performed (FiberTape®, Arthrex, Florida, USA) and reinforced using a Suture Disk (B Braun, Melsungen, Germany) femoral and a Tight Rope® button (Arthrex, Florida, USA) tibial.
Testing the ligamentous tension satisfactory results were obtained, therefore no suture tapes had to be added.
The combined LCL and femoral biceps rupture was reconstructed with a modified Larson plastic using a gracilis tendon graft with a graft length of 27 cm. LCL reconstruction was performed due to the gracilis tendon graft and attaching both sides with a 7 mm interference screw (Arthrex, Florida, USA). The femoral biceps was stabilized using a 5 mm bone anchor machining (Corkscrew® Suture Anchor, Arthrex, Florida, USA). During surgery, partial damage to the peroneal nerve was noted and treated by neurolysis. Due to the fasciectomy, the defect was addressed by VAC therapy. Post-surgical treatment included a dynamic PCL knee brace. Postoperative radiographs showed congruent articular surfaces and properly placed suture discs (Fig. 6). Intraoperatively, a passive flexion of 100° was achieved. Based on CTA, MRI and intraoperative findings the injury was classified as Schenck IV CN.
The soft tissue defect was covered by split skin grafting some weeks later.
Patient was under clinical evaluation one year following traumatic surgery. Due to missing agreement for radiological examination and clinical pictures, clinical follow-up presented a flection of 75° and extension of 5° without suspicion of arthrofibrosis. There were no abnormalities at the varus- as well as the valgus-stress-test. Further on, Lachmann and anterior drawer test demonstrated physiological values with hard jolts. Lateral instability achieved first-degree instability. Clinical examination was supplemented by Knee Injury and Osteoarthritis Outcome Score (KOOS). Symptoms of the knee were evaluated with 75 points, pain following intervention with 86 of 100 points. Activities of daily living (82/100) and quality of life (88/100) demonstrated fewer problems compared with leisure time and sports (70 points). A diagnosis of Schenck IV CN was made based on CT-A, MRI, and intraoperative evaluation [7].
Analyzing the literature and the clinical experience in this case, coherent therapeutic treatment options were presented for this special type of trauma. Being a rare injury accounting less than 0.02% of all musculoskeletal injuries, less reports discuss the evidence. More common, tibiofemoral dislocation following total knee arthroplasty were well discussed in various studies [10]. Recently, various publications postulated higher velocity injuries resulting in tibiofemoral dislocation are associated with severe multi-ligamentous injuries compared with dislocations occurred at a lower velocity [2]. In contrast, the presented case demonstrated a low impact injury leading in a multi-ligamentous anterior tibiofemoral dislocation. Demonstrating a slightly overweighted BMI, the patient could suffer the injury by body weight´s impact, Closed reduction procedure followed by ligament reconstruction for knee joint dislocation is discussed in case reports and publications [11,12]. Previous case reports demonstrated advantages in open reduction and simultaneous definitive treatment [12]. Currently, the optimal medical treatment is still debated. Based on this case report, there could be advantages in primary closed reduction and emergency vessel surgery with fasciotomy for preventing compartment syndrome. It is required, performing traumatic and orthopedic surgery following preventing severe lower limb consequences in a second reconstructive surgery. At, least, treatment strategy is debated based on clinical experience of surgeons and vascular surgeons [1,3,5,9,13].
This case highlights the relevance of prompt examination of the popliteal artery. The treatment of such cases without the possibility of ensuring the vascular supply, as well as the treatment of a compartment syndrome is not sustainable. It is essential to expect and exclude ischemia between the adductor muscle ring and the soleus muscle arcade, although the prevalence ranges from 4% to 20%. A small risk of primary compartment syndrome in popliteal artery is mainly reported in pediatrics and therefore an important concern in injured children.
Severe knee joint dislocations demonstrate a challenge for trauma surgery due to worse complications for the lower limb. Following this case, there is a recommendation for closed reduction hereinafter radiological diagnosis and emergency surgery to prevent compartment syndrome and vascular injuries in an interprofessional team consisting of emergency surgeons, vascular surgeons and orthopedic surgeons. Orthopedic surgery is recommended for subsequent days following the acute limb rescue.
References
- 1.Hegyes, M.S.; Richardson, M.W.; Miller, M.D. Knee dislocation. Complications of nonoperative and operative management. Clin Sports Med 2000, 19, 519-543, doi:10.1016/s0278-5919(05)70222-2. [Google Scholar]
- 2.Darcy, G.; Edwards, E.; Hau, R. Epidemiology and outcomes of traumatic knee dislocations: Isolated vs multi-trauma injuries. Injury 2018, 49, 1183-1187, doi:10.1016/j.injury.2018.02.016. [Google Scholar]
- 3.Moatshe, G.; Dornan, G.J.; Loken, S.; Ludvigsen, T.C.; LaPrade, R.F.; Engebretsen, L. Demographics and Injuries Associated With Knee Dislocation: A Prospective Review of 303 Patients. Orthop J Sports Med 2017, 5, 2325967117706521, doi:10.1177/2325967117706521. [Google Scholar]
- 4.Woodmass, J.M.; Romatowski, N.P.; Esposito, J.G.; Mohtadi, N.G.; Longino, P.D. A systematic review of peroneal nerve palsy and recovery following traumatic knee dislocation. Knee Surg Sports Traumatol Arthrosc 2015, 23, 2992-3002, doi:10.1007/s00167-015-3676-7. [Google Scholar]
- 5.Bonnevialle, P.; Chaufour, X.; Loustau, O.; Mansat, P.; Pidhorz, L.; Mansat, M. [Traumatic knee dislocation with popliteal vascular disruption: retrospective study of 14 cases]. Rev Chir Orthop Reparatrice Appar Mot 2006, 92, 768-777, doi:10.1016/s0035-1040(06)75945-1. [Google Scholar]
- 6.McCoy, G.F.; Hannon, D.G.; Barr, R.J.; Templeton, J. Vascular injury associated with low-velocity dislocations of the knee. J Bone Joint Surg Br 1987, 69, 285-287, doi:10.1302/0301-620X.69B2.3818761. [Google Scholar]
- 7.Goebel, C.P.; Domes, C. Classifications in Brief: The Schenck Classification of Knee Dislocations. Clin Orthop Relat Res 2020, 478, 1368-1372, doi:10.1097/CORR.0000000000001186. [Google Scholar]
- 8.Teresinski, G.; Madro, R. Knee joint injuries as a reconstructive factors in car-to-pedestrian accidents. Forensic Sci Int 2001, 124, 74-82, doi:10.1016/s0379-0738(01)00569-2. [Google Scholar]
- 9.Mohseni, M.; Simon, L.V. Knee Dislocation. In StatPearls; Treasure Island (FL), 2022. [Google Scholar]
- 10.Rouquette, L.; Erivan, R.; Pereira, B.; Boisgard, S.; Descamps, S.; Villatte, G. Tibiofemoral dislocation after primary total knee arthroplasty: a systematic review. Int Orthop 2019, 43, 1599-1609, doi:10.1007/s00264-019-04287-0. [Google Scholar]
- 11.Schmicker, T.; Kocher, T.; Patel, T.; Lycans, D. Closed Reduction of an Irreducible Knee Dislocation: A Case Report. J Orthop Case Rep 2020, 10, 6-10, doi:10.13107/jocr.2020.v10.i07.1894. [Google Scholar]
- 12.Gray, S.F.; Dieudonne, B.E. Pucker sign in irreducible posterolateral knee dislocation. Pan Afr Med J 2018, 30, 153, doi:10.11604/pamj.2018.30.153.15365. [Google Scholar]
- 13.Maithel, S.; Fujitani, R.M.; Grigorian, A.; Kabutey, N.K.; Gambhir, S.; Sheehan, B.M.; Nahmias, J. Outcomes and Predictors of Popliteal Artery Injury in Pediatric Trauma. Ann Vasc Surg 2020, 66, 242-249, doi:10.1016/j.avsg.2020.01.079. [Google Scholar]