Late presentations of retained foreign bodies are uncommon and if symptomatic should be addressed surgically.
Dr. Siva Srivastava Garika, Department of Orthopedics, Jai Prakash Narayan Apex Trauma center, AIIMS, New Delhi, India. E-mail: dr.sivasrivastava@gmail.com
Introduction: Metallic foreign body reactions are observed many times, usually in the early periods. However, late presentations are often uncommon. Management of these foreign bodies varies from a military setting to a civilian setting where saving a patient’s life is the priority.
Case Report: In this case report, we present a 49-year-old soldier with recent onset swelling in the right gluteal region with elevated local temperature and minimal tenderness. The patient suffered a land mine blast injury 10 years ago with multiple injuries to the chest, abdomen, and lower limb. According to military protocols, he was initially managed for life-threatening chest and open abdominal injuries. The right lower limb was non-salvageable and underwent above-knee amputation. A dormant metallic foreign body, which was retained inside the right iliac bone, presented a decade later with a subacute non-pyogenic abscess.
Conclusion: The primary goal in military injuries is always to save a patient’s life. While acute management remains the same for both military and civilian injuries. In military injuries, deep-seated, inactive foreign bodies are often left behind in order to avoid fresh plane dissection, and to minimize blood loss for early stabilization and save patient lives. Late-onset inflammatory responses are the cause of the delayed presentation of retained foreign bodies.
Keywords: Military injuries, foreign body reaction, late onset.
Metallic foreign body reactions are observed many times and often within a period of a few months to a year [1]. However, the late presentations, almost a decade later, of a foreign body are very rarely seen [2-4]. Even though the underlying possible mechanisms were explained by some authors, they still remain unclear [2]. Metallic foreign bodies are rarely retained in the management of civilian injuries [5]. Military injuries are addressed by lifesaving surgeries, and at times, inactive, deep-seated foreign bodies not lodged near neurovascular or vital structures are retained [5]. Patients with retained foreign bodies may have different types of symptoms, such as pain, soft-tissue swelling, and hardware irritation [3, 4]. Deep-seated foreign body removal surgeries involve long, extensive soft tissue dissection and, at times, failure to locate them in tissue planes [6]. Here we present a peculiar case of a retained foreign body in the pelvis that became symptomatic after 10 years of injury.
A 49-year-old soldier presented to us with a large ovoid right gluteal region swelling of nearly 15 cm × 10 cm × 15 cm for the past 5 months (Fig. 1).
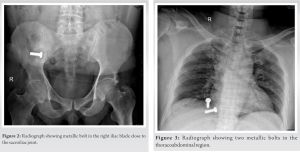
The patient had no history of any kind of recent trauma or any symptoms related to malignancy. In the past, the patient had sustained a land mine blast injury 10 years ago with secondary blast injuries to the chest, abdomen, and pelvis. On radiological evaluation, the patient had one retained metallic bolt near the right iliac blade (Fig. 2) and two bolts in the thoracoabdominal region (Fig. 3).
Following the blast, the patient was initially managed as a casualty with ATLS protocol, and a chest tube was inserted for hemopneumothorax. Later, he was taken for damage control surgery, where a laparotomy with repair of the omentum and kidney was done. The patient also sustained open fractures of the right lower limb with absent distal pulses, for which he underwent above-knee amputation. The patient had a punctured wound over the right iliac region without any sign of active bleeding. Under the principles of damage control surgery, the iliac region punctured wound was debrided and closed. He was kept in intensive care monitoring for several weeks. In the follow-up period, the patient’s right iliac region wound healed without any complications, and he was reviewed regularly on an outpatient basis. Lower-limb prosthesis for the amputation was provided to the patient. With proper rehabilitation, he improved eventually. For the past 10 years, he has been asymptomatic without any pain, swelling, or symptoms around the right gluteal region.
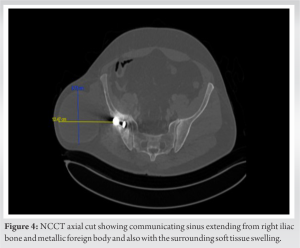
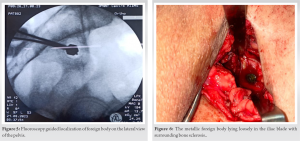
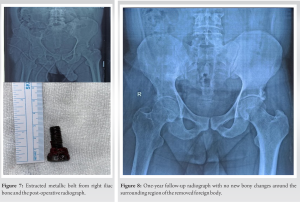
On clinical examination, there was a large ovoid swelling measuring 15 cm × 10 cm × 15 cm with a slightly raised local temperature and no localized tenderness. Serum chemistry markers for suspected infection were marginally elevated [ESR-35 mm/hour and CRP-5.6 mg/L]. On non-contrast computed tomography, there was a communicating tract extending from the right iliac bone and the metallic foreign body with surrounding soft tissue edema, suggesting an abscess formation (Fig. 4). The patient was planned for surgical intervention using the previous incision. Under fluoroscopy, the foreign body was localized (Fig. 5). Muscular planes were dissected, and roughly 750 ml of pus was evacuated. The metallic foreign body was found loosely lying in the iliac blade with surrounding bone sclerosis (Fig. 6). The sinus tract was excised, and the metallic foreign body was removed (Fig. 7).
Pus samples were sent for culture and sensitivity testing of bacterial, fungal, and slow-growing organisms, which were subsequently negative. On histopathological evaluation, scanty pus cells with non-caseation granulomas were seen. All the laboratory evaluations were in favor of a late-onset, slow reaction to the foreign body with subacute non-pyogenic abscess formation. The patient was followed up regularly for 1 year. He was completely asymptomatic without any recurrence (Fig. 8).
Following the case, the first question that comes to mind is why a foreign body was not retrieved at the initial presentation. Here, it is very important to understand that the management of injuries in a military setting is different from that of a civilian. In military injuries, there are primary and secondary blast injuries that lead to multiple foreign body retentions in the human body, along with life-threatening injuries. In this scenario, saving patients’ lives remains the primary goal [5, 7]. Absolute indications for foreign body removal are very few and only advisable in the case of any neurovascular structure abutment or involvement, which may pre-dispose to serious complications. Unnecessary exploration and opening fresh planes in healthy tissue to explore the metallic body is not advisable [2]. Common indications for retained metallic foreign body removal are localized infection, disturbed joint or part of body function, and localized pain. While rarer indications for retained metallic foreign bodies include and lead poisoning confirmed by serum lead levels, progressive neurological deficit due to cord compression confirmed by radiological investigations, and foreign body in the anterior eye chamber [2]. Metallic foreign bodies may stay in situ for a long time without causing any symptoms. Very small foreign bodies may get resorbed by degradation. The size and location of the foreign body also correlate to the type and duration of the symptoms. Patients can have minimal symptoms, such as palpable mass, visual difficulty, fever, or decreased joint movements [3,4,8]. A very late presentation of metallic foreign bodies has been reported in other medical fields [2-4,6,8]. Metallic foreign bodies lying on or inside bones mostly remain dormant for a long time. Because of the periosteal reaction, the fibrous capsulated cyst formed at the local site is thicker compared to any other tissue in the human body. Over a period of time, patients can present with acute or subacute symptoms due to the gradual release of lead by the metallic foreign body or may be due to a prolonged dormant systemic infection for which the foreign body may act as a nidus. Increasing age and systemic infection may have synergistic effects in the gradual lysis of long-standing fibrous capsulated metallic foci, which is superadded by lead release in the surrounding area. All these events lead to late-onset inflammatory reactions and subsequent pus formation. This leads to the exaggeration of the late-onset inflammatory response [2]. At times, small foreign bodies may present with serious symptoms, while large ones may remain dormant for many years [3,9,10]. In the presentation of multiple retained foreign bodies in the same patient, some of them may be symptomatic while others may remain dormant. It is still unclear regarding the selective presentation of metallic foreign bodies, like in our case, where two thoracoabdominal metallic bolts remained dormant while the single pelvic bolt presented with a large gluteal abscess [2].
The primary goal in military injuries is always to save a patient’s life. In acute presentations of deep-seated foreign bodies, unnecessary dissection and opening of fresh planes should be avoided. Those lying superficially can be removed at the time of injury with minimal exploration and breach of the fresh planes. The reason behind the selective presentation of multiple retained foreign bodies in the same patient remains unknown. Late-onset inflammatory responses are the cause of the delayed presentation of retained foreign bodies.
Foreign bodies lying in superficial planes should be removed at the time of primary management, while deep-seated foreign bodies lying in inactive planes can be left behind in polytrauma and life-saving surgeries. Out of multiple foreign bodies, some of them can present with different clinical manifestations, while others remain inactive.
References
- 1.Nusselt T, Freche S, Klinger HM, Baums MH. Intraosseous foreign body granuloma in rotator cuff repair with bioabsorbable suture anchor. Arch Orthop Trauma Surg 2010;130:1037-40. [Google Scholar]
- 2.Baldan, Marco, Christos Giannou, V. Sasin, and G. Morino. “The ICRC Metallic Foreign Bodies After War Injuries: Should We Remove Them? Experience.” East and Central African Journal of Surgery (ISSN: 1024-297X) Vol 9 Num 1 9 (January 1, 2007).. [Google Scholar]
- 3.Gupta M, Kumar Y, Rizvi A, Vig H. Accidentally lodged airgun pellet in maxilla during childhood play retrieved surgically after a decade. BMJ Case Rep 2021;14:e246709. [Google Scholar]
- 4.Rajput D, Gupta A, Shasheendran S, Mani R, Tandon A, Krishnasamy SK, et al. Laparoscopic retrieval of a 13-year-old retained iatrogenic metallic foreign body from the pelvis: An uncommon case report. Surg J (N Y) 2023;9:e62-6. [Google Scholar]
- 5.Parker W, Despain RW, Bailey J, Elster E, Rodriguez CJ, Bradley M. Military experience in the management of pelvic fractures from OIF/OEF. BMJ Mil Health 2023;169:108-11. [Google Scholar]
- 6.Botsford TW, Freni DR. Late reactions to metallic foreign bodies. N Engl J Med 1948;238:385-90. [Google Scholar]
- 7.Pilgrim CH, Brennan L. Surgical management of injured ADF personnel deployed to AFGHANISTAN 2001–2021. ANZ J Surg 2023;93:821-8. [Google Scholar]
- 8.McGimpsey SJ, Rankin SJ. Presentation of intraocular foreign body 25 years after the event. Clin Exp Ophthalmol 2005;33:665-6. [Google Scholar]
- 9.AlBilasi TM, AlDhawi LF, AlOlaywi AN, Al Mutairy AS, AlGhamdi FR, Alamry SS, et al. Fluoroscopy-guided metallic foreign body removal: A report of three cases and literature review. Cureus 2023;15:e40462. [Google Scholar]
- 10.Helito CP, Faria CE, Bonadio MB, Pecora JR, Camanho GL, Demange MK. An unusual metallic foreign body inside the knee medial femoral condyle. Case Rep Orthop 2014;2014:849020. [Google Scholar]