Disseminated cryptococcal disease is a rare but possible phenomenon which can manifest in immunocompromised patients. This should be on the differential for patients manifesting systemic disease in setting of immunocompromised state to deliver care as urgently as possible to save life and limb.
Dr. Jeffrey Bair, Department of Orthopaedic Surgery, ProMedica Toledo Hospital, 2121 Hughes Drive, HMT Suite 310, Toledo, Ohio, USA. E-mail: jeffrey.bairmd@promedica.org
Introduction: Cryptococccus neoformans is a fungus which typically presents in immunocompromised hosts, commonly presenting as meningoencephalitis. There have been very few documented incidents of intramuscular manifestations of this pathogen.
Case Report: We report on a case of a 45-year-old caucasian male with disseminated Cryptococcus neoformans who developed cryptococcal intramuscular abscesses of all extremities and osteomyelitis of the left upper limb. Clinical treatment and surgical debridement of the forearm was performed. Persistent infection resulted in a left humeral amputation and ultimately the patient’s death. This is one of the few documented intramuscular abscesses of Cryptococcus neoformans.
Conclusion: Orthopedic manifestations of cryptococcal infections are rare; however, awareness and prompt diagnosis may improve outcomes.
Keywords: Immunocompromised, Cryptococcus neoformans, intramuscular abscesses, Osteomyelitis.
The encapsulated budding yeast, Cryptococcus neoformans, is the number one cause of fungal meningitis in humans [1]. Cryptococcus typically targets individuals with compromised immune systems and impaired cell-mediated immunity, particularly those with HIV and CD4 counts of <100 cells/μL [2]. Globally, cryptococcal meningitis (CM) accounts for 19% of AIDs-related deaths [3]. Due to antiretroviral therapies, the prevalence of severe immunosuppression in HIV patients in the developed world has substantially decreased [2]. However, other reported factors causing immunosuppression have been disproportionately linked to CM in non-HIV infected patients [4]. We report a rare case of disseminated Cryptococcus neoformans in a severely, immunocompromised patient that manifested as soft tissue abscesses and intramuscular necrosis in all extremities, requiring multiple irrigation and debridements, an amputation of one of the limbs that developed osteomyelitis, and his death.
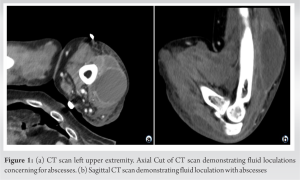
A 45-year-old immunocompromised male with stage 2 esophageal adenocarcinoma, a past medical history of Crohn’s disease treated with daily dexamethasone, and pulmonary sarcoidosis developed cryptococcal meningitis. The patient was 4 months removed from radiation and chemotherapy with taxol and carboplatin. The patient initially presented with shortness of breath and was diagnosed and treated for community-acquired pneumonia. He showed improvements but went on to develop altered mental status, word-finding difficulty, fever, unequal pupil sizes, and a petechial rash affecting his extremities 1 month later. A brain MRI showed findings suggestive of infectious meningitis, and a lumbar puncture returned positive for Cryptococcus neoformans. Further questioning of the patient revealed that he was a carpenter, having recently completed work on chicken coop structures. Infectious disease was consulted and initiated treatment with flucytosine and amphotericin B, with plans to progress to consolidation therapy with fluconazole. Over the next couple of months, despite appropriate treatment for cryptococcal infection, the patient’s CSF cryptococcal antigen titer remained elevated. The patient went on to develop diffuse left upper extremity pitting edema and cellulitic changes at the tip of his olecranon with no clear articular involvement. In addition, he demonstrated upper motor neurologic deficits of his left upper extremity including decorticate posturing throughout the elbow, wrist and fingers, and spasticity-impaired active motor control. Orthopedics were consulted and ordered advanced imaging. CT scan demonstrated loculated fluid collections which were aspirated with the return of gross purulence from the subcutaneous ulnar region (Fig. 1). Aspiration cultures as well as blood cultures demonstrated rare budding yeast, positive for Cryptococcal neoformans.
A surgical incision and debridement were performed on the left upper extremity. Gross purulence with evidence of significant myonecrosis and intramuscular abscesses were observed, requiring extensive debridement. The open wounds were initially managed with wet-to-dry dressings followed by subsequent negative pressure wound therapy (NPWT). Despite several repeat surgical debridements, he continued to develop progressive myonecrosis of his extensor musculature with observable purulence during dressing changes (Fig. 2). Further tissue cultures of the left upper extremity following debridements showed methicillin-resistant Staphylococcus aureus (MRSA), micrococcus luteus, pseudomonas aeruginosa, and rare budding yeast, confirmed as Cryptococcus. His clinical course showed brief improvements after each debridement; however, his limb continued to be a source of concern given the persistent infection and volume of necrotic tissue. These factors coupled with his poor wound healing potential led to a plan for amputation. A left humeral guillotine amputation was performed 5 weeks after his initial debridement. Pathology of the amputated limb revealed skin and soft tissue necrosis and acute osteomyelitis. Clinically, he demonstrated brief improvement following the amputation, although this response was short lived.
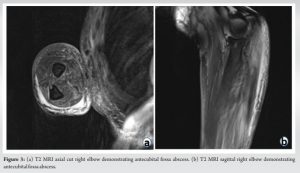
The right upper extremity soon developed nodules and abscess formation above the right forearm and antecubital fossa. MRI of the right upper extremity demonstrated multiple non-enhancing lesions at the elbow and proximal forearm which were concerning for abscess formation (Fig. 3).
Surgical debridement was performed which showed purulence and active infection (Fig. 4). Tissue and aspiration cultures similarly demonstrated rare, encapsulated yeast.
The patient continued to decompensate, developed acute respiratory failure, and was intubated, followed later by a tracheostomy. He then developed an additional fluid collection of the right lower extremity that required extensive surgical debridement (Fig. 5). Along with extensive necrosis, purulence, and abscess formation of the right lower extremity, there were observable pale, plaque pockets of suspected fungal abscesses ranging in size from 2-3 mm to 2 cm in the deep posterior compartment. Surgical pathology of the right lower extremity demonstrated extensive acute inflammation and necrosis, with the presence of numerous yeast formations.
A repeat debridement of the right lower extremity was deferred after an additional CT scan revealed fluid collections forming in the patient’s abdomen, pelvis, and remaining extremities. His code status was transitioned to Do-Not-Resuscitate Comfort Care (DNR-CC). The patient expired that day 6 months after his initial cryptococcal meningitis diagnosis and 3 months after the first I&D of his left upper extremity. Cause of death was determined as disseminated cryptococcal infection secondary to immunosuppression.
Cryptococcus neoformans is an encapsulated yeast distributed globally within soil and in the feces of birds, particularly pigeons [5]. Exposure is believed to occur during early childhood, primarily through inhalation [6]. Its major virulence factor originates from its polysaccharide capsule which inhibits antibodies, leukocyte migration, and phagocytosis [5]. In general, the pathogen will remain latent in immunocompetent hosts within granulomas in the lungs [7, 8] or infection is evaded through macrophage-mediated destruction [5]. Immunocompromised hosts, such as those with HIV, have dysfunctional alveolar macrophages which can lead to replication and dissemination into the bloodstream and brain [5]. With the introduction of HAART therapy, there was a sharp decline in HIV-positive cryptococcal cases from 1995 to 1997. Other mechanisms behind immunosuppression have shown to elicit a similar risk of developing disseminated cryptococcal infection. A study done by Pyrgos et al. [4] analyzed cryptococcal meningitis hospitalizations in the U.S. from 1997 to 2007. Several non-HIV co-morbidities were identified representing risk factors for cryptococcal meningitis infection, including hematopoietic tumors, immunosuppressive conditions associated with leukopenia, sarcoidosis, T-cell defects, hypogammaglobulinemia, liver disease, and rheumatological diseases requiring steroid treatment. Further, sarcoidosis has been identified as an independent risk factor for cryptococcal infection [9]. Our patient carried several risk factors that contributed to his cryptococcal disseminated infection. These included sarcoidosis, esophageal carcinoma, recent chemotherapy and radiation treatment, as well as chronic steroid treatment with dexamethasone. The most common clinical manifestation of cryptococcal neoformans is meningoencephalitis [10-13]. Typical symptoms for CM are subacute headache and altered mental status, with other manifestations including elevated intracranial pressure (ICP), ocular involvement among 40% of CM patients [14, 15], progressive pneumonia, cryptococcomas in the lungs, and skin lesions. Less than 20% of patients with CM have the classic meningitis presentation of a “stiff neck [10]. Skin manifestations are the third most common presenting symptom behind CNS and pulmonary infection. Skin symptoms commonly present as “molluscum-contagiosum like” lesions [16]. Soft-tissue abscesses and cellulitis can present in immunocompromised patients, representing cryptococcal dissemination [17]. Dissemination is confirmed through a positive blood culture [10]. We can hypothesize that our patient’s initial presentation to the ED with pneumonia was due to cryptococcal infection through pulmonary inhalation. His blood cultures were negative at the time, and he was treated with antibiotics for a suspected community-acquired pneumonia. Improper treatment and his risk factors resulted in cryptococcal dissemination to the bloodstream and brain. He presented about a month later after his initial pneumonia diagnosis with the classic cryptococcal meningoencephalitis symptoms including a headache, altered mental status, ocular involvement, and a petechial rash. Although a correct diagnosis and antifungal treatment were initiated at the time, his severely immunosuppressed state and malnutrition resulted in further dissemination to his limbs, developing as intramuscular abscesses. A rare presentation of disseminated cryptococcal infection is within the bone, occurring in 5-10% of patients with cryptococcus [18]. Cryptococcal osteomyelitis and abscess formation often present together [19]; it has been thought that cryptococcus seeds the bone first, spreading then to the surrounding musculature and forming the cryptococcal abscess [20-22]. Although our patient developed osteomyelitis of the left upper extremity, this was after first developing intramuscular abscesses and necrosis. In addition, formation of widespread abscesses and intramuscular necrosis of his right upper extremity and bilateral lower extremities occurred without any evidence of osteomyelitis. The left lower extremity was never formally debrided but similar abscess could be appreciated on CT scan without bony involvement. We were only able to identify one other case of cryptococcal dissemination manifesting as an intermuscular mass in the absence of bony invasion [19]. Orthopedic surgeons treating patients with active cryptococcal infection with soft tissue abscesses should have a high index of suspicion for dissemination and pursue prompt treatment with rapid irrigation and debridement and a multi-disciplinary approach involving an Infectious Disease team. Furthermore, consider the osseous involvement and pursue confirmatory osteomyelitis diagnostic testing such as MRI, CT scan, or nuclear medicine studies bone scans. This may allow for more aggressive surgical strategies as well as drive conversations related to goals of care.
Cryptococcus neoformans is reasonably treatable in its meningoencephalitis stage, however, a patient’s immune status and concurrent risk factors may ultimately fuel dissemination into other organs. While cryptococcal pneumonia and subsequent dissemination into the CNS is a common presentation of this fungus, dissemination into soft tissue in the absence of bone invasion is a rare phenomenon. Without prompt diagnosis and treatment, patients may rapidly deteriorate when faced with systemic cryptococcal dissemination requiring considerable medical and surgical treatment.
Disseminated cryptococcal disease is a rare but possible phenomenon which can manifest in immunocompromised patients. This should be on the differential for patients manifesting systemic disease in setting of immunocompromised state to deliver care as urgently as possible to save life and limb.
References
- 1.Chaudhuri A. Fungal Meningitis-Symptoms, Diagnosis and Treatment; 2022. Available from: https://bestpractice.bmj.com/topics/en-us/541 [Last accessed on 2023 Jan 30]. [Google Scholar]
- 2.Sloan DJ, Parris V. Cryptococcal meningitis: Epidemiology and therapeutic options. Clin Epidemiol 2014;6:169-82. [Google Scholar]
- 3.Rajasingham R, Govender NP, Jordan A, Loyse A, Shroufi A, Denning DW, et al. The global burden of HIV-associated cryptococcal infection in adults in 2020: A modelling analysis [published correction appears in Lancet Infect Dis 2022]. Lancet Infect Dis 2022;22:1748-55. [Google Scholar]
- 4.Pyrgos V, Seitz AE, Steiner CA, Prevots DR, Williamson PR. Epidemiology of cryptococcal meningitis in the US: 1997-2009. PLoS One 2013;8:e56269. [Google Scholar]
- 5.Del Valle L, Piña-Oviedo S. HIV disorders of the brain: Pathology and pathogenesis. Front Biosci 2006;11:718-32. [Google Scholar]
- 6.Goldman DL, Khine H, Abadi J, Lindenberg DJ, Pirofski LA, Niang R, et al. Serologic evidence for Cryptococcus neoformans infection in early childhood. Pediatrics 2001;107:E66. [Google Scholar]
- 7.Goldman DL, Lee SC, Mednick AJ, Montella L, Casadevall A. Persistent Cryptococcus neoformans pulmonary infection in the rat is associated with intracellular parasitism, decreased inducible nitric oxide synthase expression, and altered antibody responsiveness to cryptococcal polysaccharide. Infect Immun 2000;68:832-8. [Google Scholar]
- 8.Garcia-Hermoso D, Janbon G, Dromer F. Epidemiological evidence for dormant Cryptococcus neoformans infection. J Clin Microbiol 1999;37:3204-9. [Google Scholar]
- 9.Bernard C, Maucort-Boulch D, Varron L, Charlier C, Sitbon K, Freymond N, et al. Cryptococcosis in sarcoidosis: CryptOsarc, a comparative study of 18 cases. QJM 2013;106:523-9. [Google Scholar]
- 10.Mada PK, Jamil RT, Alam MU. Cryptococcus. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. [Google Scholar]
- 11.Kaplan JE, Hanson D, Dworkin MS, Frederick T, Bertolli J, Lindegren ML, et al. Epidemiology of human immunodeficiency virus-associated opportunistic infections in the United States in the era of highly active antiretroviral therapy. Clin Infect Dis 2000;30 Suppl 1:S5-14. [Google Scholar]
- 12.Mirza SA, Phelan M, Rimland D, Graviss E, Hamill R, Brandt ME, et al. The changing epidemiology of cryptococcosis: An update from population-based active surveillance in 2 large metropolitan areas, 1992-2000. Clin Infect Dis 2003;36:789-94. [Google Scholar]
- 13.Van Elden LJ, Walenkamp AM, Lipovsky MM, Reiss P, Meis JF, De Marie S, et al. Declining number of patients with cryptococcosis in the Netherlands in the era of highly active antiretroviral therapy. AIDS 2000;14:2787-8. [Google Scholar]
- 14.Lesser RL, Simon RM, Leon H, Siegel N. Cryptococcal meningitis and internal ophthalmoplegia. Am J Ophthalmol 1979;87:682-7. [Google Scholar]
- 15.Kestelyn P, Taelman H, Bogaerts J, Kagame A, Abdel Aziz M, Batungwanayo J, et al. Ophthalmic manifestations of infections with Cryptococcus neoformans in patients with the acquired immunodeficiency syndrome. Am J Ophthalmol 1993;116:721-7. [Google Scholar]
- 16.Chayakulkeeree M, Perfect JR. Cryptococcosis. In: Hospenthal, DR, Rinaldi MG, editors. Diagnosis and Treatment of Human Mycoses. Infectious disease. United States: Humana Press; 2008. [Google Scholar]
- 17.Bernardes T, Ostilla L, Fazal A, Nasseri-Nik N, Otrakji C, Haddad G, et al. When in doubt, cut it out: Biopsy as key in diagnosing cryptococcal soft tissue infection. Cureus 2022;14:e21111. [Google Scholar]
- 18.Sethi S. Cryptococcal osteomyelitis in the ribs. J Glob Infect Dis 2010;2:63-4. [Google Scholar]
- 19.Cho YJ, Han SI, Lim SC. Cryptococcal infection presenting as soft tissue abscess and arthritis: Case report. Medicine (Baltimore) 2021;100:e26656. [Google Scholar]
- 20.DiNardo AR, Schmidt D, Mitchell A, Kaufman Y, Tweardy DJ. First description of oral Cryptococcus neoformans causing osteomyelitis of the mandible, manubrium and third rib with associated soft tissue abscesses in an immunocompetent host. Clin Microbiol Case Rep 2015;1:17. [Google Scholar]
- 21.Harris RM, Stillman IE, Goldsmith JD, Qian Q, Kirby JE. Pathological rib fracture and soft tissue mass simulating malignancy--Cryptococcus, an unsuspected culprit. Diagn Microbiol Infect Dis 2015;81:189-91. [Google Scholar]
- 22.Poenaru SM, Rofaiel R, Hosseini-Moghaddam SM. Cryptococcus neoformans osteomyelitis and intramuscular abscess in a liver transplant patient. BMJ Case Rep 2017;2017:bcr2017221650. [Google Scholar]