The case report illustrates the complexities of addressing recurrent anterior dislocation following Reverse Total Shoulder Arthroplasty (RTSA), showcasing the efficacy of secondary pectoralis major transfer as a salvage option for restoring stability in challenging postoperative RTSA associated complication.
Dr. Chang Hee Baek, Department of Orthopaedic Surgery, Yeosu Baek Hospital, Jeollanam-do, Republic of Korea, 50, Yeoseo 1-ro, Yeosu-si, Jeollanam-do, Republic of Korea. E-mail: Yeosubaek@gmail.com
Introduction: Reverse total shoulder arthroplasty (RTSA) has revolutionized the treatment landscape for a spectrum of shoulder pathologies, extending its indications from rotator cuff arthropathy to encompass irreparable rotator cuff lesions, fractures, inflammatory arthritis, and tumors. However, the exponential increase in RTSA usage has brought a proportional rise in associated complications, with dislocation being one of the most common early post-operative complications.
Case Report: This case report details a 65-year-old right-hand dominant male patient presenting with chronic pain and weakness in the right shoulder, diagnosed with advanced glenohumeral arthritis and massive irreparable rotator cuff tears. The patient underwent a Bony Increased-Offset RTSA (BIO-RTSA) procedure, coupled with subscapularis repair. Postoperatively, the patient experienced pain and instability, culminating in an atraumatic anterior dislocation at 4 months. Despite conservative management, recurrent dislocations persisted. Revision surgery was performed with an increase in the linear component size for containment. About 1 year postoperative of the revision surgery, recurrent dislocation reoccurred. Re-revision surgery was performed with secondary pectoralis major (PM) transfer for subscapularis deficiency due to re-tear from recurrent dislocation, and with an increased humeral tray size for better containment. About 1-year and 6-month post-operative to the re-revision surgery, the patient achieved restored stability, improved range of motion, and reported satisfaction with the outcome.
Conclusion: This case report underscores the challenges of managing recurrent anterior dislocation after RTSA. The successful use of secondary PM transfer highlights its efficacy as a salvage procedure in restoring stability for persistent anterior dislocation after RTSA. Yet, further clinical studies are warranted to establish the role of such interventions in the management for RTSA-associated complications.
Level of Evidence IV; Case report
Keywords: Reverse total shoulder arthroplasty, pectoralis major transfer, irreparable rotator cuff tear, rotator cuff arthroplasty, tendon transfer.
Reverse total shoulder arthroplasty (RTSA) has been promising treatment option for rotator cuff arthropathy [1]. Due to its success, the indications for RTSA have expanded to include irreparable rotator cuff lesions, fractures, inflammatory arthritis, or even tumors [2]. As RTSA has shown satisfactory results in both elderly and young patients [3], the rate of RTSA usage has increased, but inevitably leading to a rise in complications and revision surgeries over the past decade [4, 5]. These complications include prosthetic instability, scapular notching, deep infection, periprosthetic fractures, acromial or scapular spine fracture, glenoid or humeral component loosening, and many others [6-8]. Among the complications, the most common case of early complication is dislocation, with the highest reported rate up to 31% [9-11]. Associated factors related dislocation and instability are abnormal version of implant, body mass index over 30, male gender, subscapularis deficiency, prior surgeries, bone deficiencies, and traumas [12, 13]. Managing dislocation or instability following revision RTSA poses a significant challenge. Adjusting component positions and ensuring appropriate arm length with proper soft tissue tension may resolve the majority of unstable RTSA cases; however, instances may persist where patient experiences recurrent dislocation. In our current case report, we present successful management of recurrent anterior dislocation following RTSA, treated with secondary pectoralis major (PM) transfer.
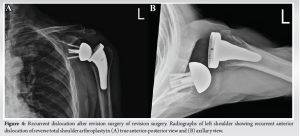
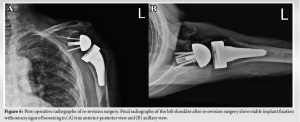
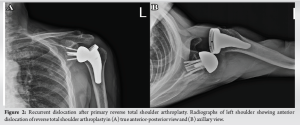
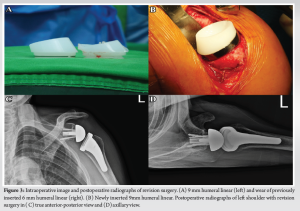
A 65-year-old male patient, right-hand dominant, visited our outpatient clinic with complaints of chronic pain and weakness in his right shoulder. Thorough examination revealed advanced rotator cuff arthropathy. Due to posterior wear of the glenoid, the patient underwent a Bony Increased-Offset RSA (BIO-RTSA, Biomet, Warsaw, IN, USA), along with subscapularis repair (Fig. 1). Following the procedure, the patient reported pain and instability during shoulder movement, culminating in an atraumatic dislocation at 4 months postoperatively (Fig. 2). Despite of conservative treatment, the patient continued to experience recurrent dislocations thereafter. There was no notable abnormality in the implant versions on both the glenoid and humeral sides. A revision surgery was performed as we believed that it is loose of implant containment. Intraoperatively, there was no evidence of implant loosening; however, a re-tear of the previously repaired subscapularis was noted. The subscapularis was medially retracted with poor tendon quality and could not be repaired, and the implant containment was found to be loose. To address this, we exchanged the linear component from 6 mm to 9 mm to enhance tension and implant containment (Fig. 3). After the revision surgery, the patient experienced an improved range of motion (ROM) and no longer suffered from instability or dislocation for the next year. However, at the 1-year post-operative follow-up, the patient revisited our clinic and complained of feeling sense of instability during forward flexion and abduction. The patient underwent a regimen of strengthening exercises. Nevertheless, the patient experienced several anterior dislocations (Fig. 4). To address this problem, we proposed a secondary PM transfer for the anterior dislocation for deficiency and an increase in the humeral tray for further tension and containment.
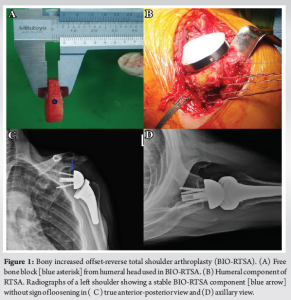
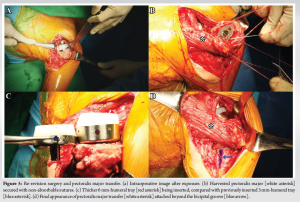
The revision surgery began by using the previous incision of the deltopectoral approach but with the incision extended inferiorly to the lower part of the PM muscle’s insertion site (Fig. 5a). We dislocated the shoulder and extracted humeral tray component. After releasing both the upper and lower borders of the PM muscle from the surrounding soft tissue, the entire PM, without separating the clavicular and sternal heads, was detached from its humeral insertion site. Both the upper and lower edges of the harvested PM were secured with two non-absorbable sutures (Fig. 5b). Next, we inserted a new humeral tray that was thicker than the one previously inserted for better containment (Fig. 5c), and reduction was performed. Subsequently, a drill bit loaded with a 2.0 mm K-wire was used to create two parallel transosseous tunnels from the upper edge of the bicipital groove to the upper edge of the teres minor insertional site in the greater tuberosity. For each upper and lower tunnel, a free non-absorbable suture was shuttled and passed through each tunnel. These transosseous sutures were initially tied together and subsequently threaded through the lateral portion of the harvested PM in a Krockow suture configuration. Finally, these sutures were tied together with non-absorbable sutures of the harvested PM to complete the final attachment of the PM to the humerus laterally beyond the bicipital groove (Fig. 5d). For postoperative rehabilitation, patient was instructed to wear an abduction brace, but allowed intermittent movement for daily tasks for initial post-operative 4 weeks. Afterward, the brace was removed, and active assisted ROM exercises began. By the post-operative 3 months, patient progressed to strengthening exercises. However, heavy labor and sports were prohibited until the postoperative 6 months. Subsequently, at 1-year and 6-month postoperative follow-up of re-revision surgery, the patient’s satisfaction was evident, with a Constant score of 82/100 and an ASES (American Shoulder and Elbow Surgeon) score of 81/100. ROM measurements included 150° for forward elevation, 150° for abduction, 35° for external rotation, and internal rotation to the level of the third lumbar vertebrae. Radiographic images revealed a securely fixed implant without any signs of loosening (Fig. 6). At 1-year and 6-month postoperative to the re-revision surgery, the patient has no longer experienced recurrent dislocations and has reported satisfaction with the outcome.
RTSA has been widely used for rotator cuff arthropathy and its indication has been widened to cover variety of disease including proximal humerus fracture, irreparable rotator cuff tear, tumor, arthritis, and many others [1-3]. As the living age life span of general population has increased, the increasing number of RTSA has also increased [4, 5]. As a result, like any surgical procedure involving prosthesis implantation, it introduces a spectrum of potential complications. These complications include prosthetic instability, scapular notching, acromial fractures, infection, periprosthetic fractures, deltoid weakness, and implant loosening [6-8]. The one of most common complications in early post-operative period is dislocation, with rates ranging from 1.5% to 31% [4, 9, 11, 13]. Many recommendation to treat instability or dislocation has been discussed in literatures [13-15]. These include identifying the mechanism and accompanying pathology of instability, making decisions regarding appropriate implant sizing, considering the potential use of different types of prostheses, and requiring surgical expertise to remove scar tissue near neurovascular structures [13, 15]. Furthermore, surgeon must address arm length, bony impingement, component malposition, component wear, and soft-tissue laxity [4]. However, managing the unstable RTSA is challenging task, with a reported failure rate of revision RTSA ranging between 15% and 40% [13]. Dislocation can be associated with various biomechanical factors, including humeral shortening and/or excessive medialization, the version of the implant, socket constraint, soft-tissue tensioning, and nerve dysfunction [4]. In our case report, patients experienced recurrent dislocation after primary RTSA. For the first revision surgery, our aim was to increase the soft tissue tension, as we believed that the versions of both the glenoid and humeral implants, and glenoid tilt seemed to be normal through CT scan (Computed Tomography scan) and X-ray. Furthermore, after thorough physical examination and electromyography study, there was no nerve dysfunction, including the axillary nerve. However, anterior dislocation recurred even after the revision surgery, leading us to consider the possibility of subscapularis deficiency from recurrent dislocation. Given that PM transfer has been widely recognized for treating irreparable subscapularis tear [16, 17], we applied secondary PM transfer during the final revision surgery. As a result, the patient no longer showed recurrent dislocation even 1 year and 6 months after the postoperative period, and there was no longer a sense of instability experienced. In setting of RTSA, subscapularis deficiency can sometimes cause significant complication. However, the necessity of repairing the subscapularis during RTSA surgery remains a subject of ongoing debate. Some studies have shown that regardless of whether the subscapularis is repaired, the complications or dislocation rates do not differ [18, 19]. However, Edwards et al. [20] found an increased risk of instability when the subscapularis was not repaired. Furthermore, Collin et al. [21] advocated for the repair of reparable subscapularis tendons during RTSA whenever feasible. However, there are cases where the subscapularis is found to be irreparable, either at the primary RTSA surgery or, as in our case, at the revision RTSA. As subscapularis deficiency could lead to a potential complication, alternative treatment options could be necessary. Kany et al. [22] suggested the utilization of RTSA with anterior latissimus dorsi (LD) transfer and Baek et al. [23] proposed the utilization of RTSA with anterior combined anterior LD and Teres major transfer. Although rarely reported, PM transfer with RTSA have been documented in some literature, but mostly for deltoid paralysis [24, 25]. Nevertheless, our case report highlights the promising clinical outcome of secondary PM transfer in a patient with persistent anterior dislocation after primary RTSA.
In this current case report, we detailed persistent anterior dislocation after RTSA treated with secondary PM transfer. In setting of RTSA, subscapularis deficiency can occasionally present a challenging and notable complication. Secondary PM transfer could be a potential treatment option when dealing with recurrent anterior dislocation after RTSA due to subscapularis deficiency. Nonetheless, as there is a lack of clinical studies on RTSA combined with PM transfer, further clinical studies are still warranted.
We report promising clinical outcomes of secondary PM transfer at post-operative 1 year and 6 months after revision surgery for a patient who had previously undergone RTSA but suffered recurrent anterior dislocation. The successful use of secondary PM transfer highlights its efficacy as a salvage procedure in restoring stability for persistent anterior dislocation after RTSA.
References
- 1.Ernstbrunner L, Andronic O, Grubhofer F, Camenzind RS, Wieser K, Gerber C. Long-term results of reverse total shoulder arthroplasty for rotator cuff dysfunction: A systematic review of longitudinal outcomes. J Shoulder Elbow Surg 2019;28:774-81. [Google Scholar]
- 2.Testa EJ, Glass E, Ames A, Swanson DP, Polisetty TS, Cannon DJ, et al. Indication matters: Effect of indication on clinical outcome following reverse total shoulder arthroplasty-a multicenter study. J Shoulder Elbow Surg 2023;33:1235-42. [Google Scholar]
- 3.Bedeir YH, Gawish HM, Grawe BM. Outcomes of reverse total shoulder arthroplasty in patients 60 years of age or younger: A systematic review. J Hand Surg Am 2020;45:254.e1-8. [Google Scholar]
- 4.Chae J, Siljander M, Wiater JM. Instability in reverse total shoulder arthroplasty. J Am Acad Orthop Surg 2018;26:587-96. [Google Scholar]
- 5.Klug A, Herrmann E, Fischer S, Hoffmann R, Gramlich Y. Projections of primary and revision shoulder arthroplasty until 2040: Facing a massive rise in fracture-related procedures. J Clin Med 2021;10:5123. [Google Scholar]
- 6.Ascione F, Schiavone Panni A, Braile A, Corona K, Toro G, Capuano N, Romano AM. Problems, complications, and reinterventions in 4893 onlay humeral lateralized reverse shoulder arthroplasties: A systematic review (part I-complications). J Orthop Traumatol 2021;22:27. [Google Scholar]
- 7.Ascione F, Panni AS, Braile A, Corona K, Toro G, Capuano N, et al. Problems, complications, and reinterventions in 4893 onlay humeral lateralized reverse shoulder arthroplasties, a systematic review: Part II-problems and reinterventions. J Orthop Traumatol 2021;22:49. [Google Scholar]
- 8.Wierks C, Skolasky RL, Ji JH, McFarland EG. Reverse total shoulder replacement: Intraoperative and early postoperative complications. Clin Orthop Relat Res 2009;467:225-34. [Google Scholar]
- 9.Cheung EV, Sarkissian EJ, Sox-Harris A, Comer GC, Saleh JR, Diaz R, et al. Instability after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2018;27:1946-52. [Google Scholar]
- 10.Cronin KJ, Hadley CJ, Hameed D, Williams GR, Lazarus MD, Namdari S. Outcomes of instability after reverse shoulder arthroplasty: Reoperation and persistent instability are common. J Shoulder Elbow Surg 2022;31:1738-42. [Google Scholar]
- 11.Chalmers PN, Rahman Z, Romeo AA, Nicholson GP. Early dislocation after reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014;23:737-44. [Google Scholar]
- 12.Parsons M, Elwell J, Muh S, Wright T, Flurin P, Zuckerman J, et al. Impact of accumulating risk factors on the incidence of dislocation after primary reverse total shoulder arthroplasty using a medial glenoid-lateral humerus onlay prosthesis. J Shoulder Elbow Surg 2024;???:S1058-2746(24)00084-3. [Google Scholar]
- 13.Melbourne C, Munassi SD, Ayala G, Christmas KN, Diaz M, Simon P, et al. Revision for instability following reverse total shoulder arthroplasty: Outcomes and risk factors for failure. J Shoulder Elbow Surg 2023;32:S46-52. [Google Scholar]
- 14.Abdelfattah A, Otto RJ, Simon P, Christmas KN, Tanner G, LaMartina J 2nd, et al. Classification of instability after reverse shoulder arthroplasty guides surgical management and outcomes. J Shoulder Elbow Surg 2018;27:e107-18. [Google Scholar]
- 15.Markes AR, Cheung E, Ma CB. Failed reverse shoulder arthroplasty and recommendations for revision. Curr Rev Musculoskelet Med 2020;13:1-10. [Google Scholar]
- 16.Updegrove G, Kohler J, Ponnuru P, Armstrong AD. Pectoralis major tendon transfer for management of subscapularis failure after anatomic total shoulder arthroplasty: Technique and results. JSES Rev Rep Tech 2022;2:451-7. [Google Scholar]
- 17.Reid JJ, Garrigues GE, Friedman RJ, Eichinger JK. Irreparable subscapularis tears: Current tendon transfer options. Curr Rev Musculoskelet Med 2024;17:68-75. [Google Scholar]
- 18.Franceschetti E, De Sanctis EG, Ranieri R, Palumbo A, Paciotti M, Franceschi F. The role of the subscapularis tendon in a lateralized reverse total shoulder arthroplasty: Repair versus nonrepair. Int Orthop 2019;43:2579-86. [Google Scholar]
- 19.Friedman RJ, Flurin PH, Wright TW, Zuckerman JD, Roche CP. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J Shoulder Elbow Surg 2017;26:662-8. [Google Scholar]
- 20.Edwards TB, Williams MD, Labriola JE, Elkousy HA, Gartsman GM, O’Connor DP. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J Shoulder Elbow Surg 2009;18:892-6. [Google Scholar]
- 21.Collin P, Rol M, Muniandy M, Gain S, Lädermann A, Ode G. Relationship between postoperative integrity of subscapularis tendon and functional outcome in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2022;31:63-71. [Google Scholar]
- 22.Kany J. Tendon transfers in rotator-cuff surgery. Orthop Traumatol Surg Res 2020;106:S43-51. [Google Scholar]
- 23.Baek CH, Kim JG, Baek GR. Restoration of active internal rotation following reverse shoulder arthroplasty: Anterior latissimus dorsi and teres major combined transfer. J Shoulder Elbow Surg 2022;31:1154-65. [Google Scholar]
- 24.Elhassan BT, Wagner ER, Werthel JD, Lehanneur M, Lee J. Outcome of reverse shoulder arthroplasty with pedicled pectoralis transfer in patients with deltoid paralysis. J Shoulder Elbow Surg 2018;27:96-103. [Google Scholar]
- 25.Burkhard MD, Grubhofer F, Wieser K, Elhassan BT. Pedicled pectoralis major transfer for irreparable dehiscence of the deltoid in reverse total shoulder arthroplasty: surgical technique and case report. JSES Rev Rep Tech 2021;1:218-23. [Google Scholar]