In medullary osteosarcoma of the femur, where there is no distant metastasis, radical tumor resection is safe, effective, and potentially curative
Dr. Dominic Konadu-Yeboah, Department of Orthopaedics and Trauma, Komfo Anokye Teaching Hospital, Kumasi, Ghana/ Department of Surgery, School of Medical Sciences, Kwame Nkrumah University of Science and Technology, Kumasi, Ghana. E-mail: domiyk@yahoo.com
Introduction: Osteosarcoma is a malignant mesenchymal neoplasm in which the tumor cells produce defective and immature bone (osteoid). The risk factors for developing the disease include: Patients with hereditary retinoblastoma and germline mutations of the p53 tumor suppressor gene.
Case Report: A 32-year old male presented with pain and swelling of the left thigh of 9 months duration. The pain was progressive, excruciating, worse at night, and unresponsive to paracetamol with moderate weight loss. He had sought treatment from a traditional bonesetter 6 months before presentation and had no improvement of the symptoms.
Conclusion: In medullary osteosarcoma of the femur, where there is extracomparmental disease with no distant metastasis, clinically and radiologically, radical tumor resection with a free oncological margin increases survival of the patient up to 7 years.
Keywords: Medullary osteosarcoma, malignant tumor, metastasis, extracompartmental
Osteosarcoma is a malignant mesenchymal neoplasm in which the tumor cells produce defective and immature bone (osteoid). The risk factors for developing the disease include: Patients with hereditary retinoblastoma and germline mutations of the p53 tumor suppressor gene which are more frequently seen in sporadic osteosarcoma [1,2]. It has a male-to-female ratio of between 1.5:1 and 2:1. The metaphysis of long tubular bones is most frequently affected, especially the distal femur [1]. It is an aggressive tumor and the most common malignant primary neoplasm of bone; and the most common sarcoma, affecting about 560 children and adolescents annually in the US [1]. Conflicting findings have been reported on the survival and functional recovery in osteosarcoma patients following amputation [3]. Twenty percent of patients have clinically detectable metastasis at the time of hospital presentation. Micrometastases are presumed to be present in many of the remaining patients [4]. The classification of the disease is complex and more than 12 different subtypes have been described. The World Health Organization classification of osteosarcoma recognizes three major sub-types of high-grade intramedullary osteosarcoma: Osteoblastic, chondroblastic, and fibroblastic, based on the predominant type of matrix within the tumor. Other histological variants include: Low-grade intramedullary osteosarcoma, parosteal osteosarcoma, and periosteal osteosarcoma [5,6]. The disease has also been classified as: High-grade surface osteosarcoma, telangiectatic osteosarcoma, small cell osteosarcoma, and secondary osteosarcoma which may occur in Paget’s disease [6]. Metastatic disease occurs in up to 30% of patients diagnosed with osteosarcoma [4]. The common metastatic sites are the lungs, bones, regional lymph nodes, and visceral organs (heart, liver, pancreas, and small bowel) [7]. Peritoneal, skeletal muscles, subcutaneous fat, and cutaneous metastases are very rare [8]. In low- and middle-income countries, most patients with the disease present late and the outcomes are generally poor. Osteosarcoma is an aggressive skeletal neoplasm and about 40–50% of patients develop pulmonary metastasis. It is the most common sarcoma, affecting about 560 children and adolescents annually in the US. It has a male-to-female ratio of between 1.5:1 and 2:1. The metaphysis of long tubular bones is most frequently affected, especially along the distal femur [4,7]. Twenty percentages of patients have clinically detectable metastasis at the time of hospital presentation. Micrometastases are presumed to be present in many of the remaining patients [9,10]. Medullary osteosarcoma has a poor prognosis with a long-term survival rate of 10–30%. Conflicting findings have been reported on the survival and functional recovery in osteosarcoma patients following amputation [3].
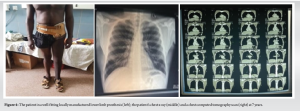
We report our experience in the management of a 32-year old male, mechanic, who presented to us with pain and swelling of the left thigh of 9 months duration. The pain was progressive, excruciating, worse at night, and unresponsive to paracetamol. There was no antecedent trauma to the affected thigh. There was a history of moderate weight loss. He had sought treatment from a traditional bonesetter 6 months before presentation, who massaged the thigh swelling with herbs and tied the affected thigh with sticks. He had received three sessions of treatment from the bonesetter over 6 months and had no improvement of the symptoms and, hence, decided to seek hospital care. He was the first of three siblings, the rest of whom were alive and well and a mechanic by profession. A radiograph showed a large lytic lesion in the intertrochanteric region of the left femur with multiple small ones in the medullary canal with endosteal scalloping. A core-needle biopsy of the lesion revealed a high-grade sarcoma. A diagnosis of extracompartmental intramedullary osteosarcoma of the left femur, Enneking stage IIB, was made following a computerized tomography (CT) scan and magnetic resonance imaging (MRI) of the left thigh. The patient was counseled for and underwent radical tumor resection-left hip disarticulation through the anterior approach to the left hip joint. During the surgery, a flap of the gluteus maximus muscle, which was clinically and radiologically free of tumor, was raised to fashion a stump. The 5-h surgery was performed in April 2016, under spinal anesthesia, through grossly normal tissues. At surgery, hydrogen peroxide was instilled to “sterilize” the tumor bed. He was transfused three units of whole blood intraoperatively. The entire resected limb was sent for histopathology. The histopathologist reported an adequately free resection margin. Oncologist declined adjuvant treatment, citing poor tumor response rate. He mobilized with the aid of a pair of axillary crutches on post-operative day (POD) 1, full weight-bearing on the contralateral limb. The operative wound healed uneventfully and skin sutures were removed on POD 14. He was discharged home on POD 14 and referred for prosthesis fitting and gait training. At 7 years following surgery, the patient has no symptoms. Repeat CT scan and MRI of the stump and chest show no tumor. The patient currently attends a shop and boards public transport and is able to sit on a water closet. He had a locally manufactured prosthesis fitted at 1 year after surgery and has been in it for 6 years. The amputation stump has a healthy looking skin; it is stable and well-padded. The x-ray of the tumor and the computed tomography (CT) scan of the chest at the time of diagnosis is shown in Fig. 1. The magnetic resonance imaging of the affected thigh and the surgical incision markings are depicted in Fig. 2. The appearance of the hip disarticulation stump and an x-ray of the pelvis at 7 years is shown in Fig. 3. The left lower limb prosthesis, chest x-ray and chest CT scan of the patient at 7 years are depicted in Fig. 4.



Our patient had a locally advanced tumor and had no evidence of pulmonary metastasis at the time of diagnosis and is clinically and radiologically disease-free at 7 years following surgery. On the contrary, several studies have reported that in medullary osteosarcoma, metastatic disease occurs in up to 30% of patients at the time of diagnosis and micrometastases are presumed to be present in many of the remaining patients [1,8,11,12]. Distant spread to the lungs accounts for 80% of metastatic cases [13]. In addition, 7 years post-radical tumor resection, there is no evidence of local or pulmonary metastasis in our patient. This finding supports the report by many authors that there are higher rates of local recurrence following limb salvage compared to a radical amputation or disarticulation [13,14]. The radical resection in the patient of our report with the achievement of free oncological margins could explain the 7-year disease-free survival. It has been shown in other studies that after tumor resection, patients should be followed up for at least 5 years for tumor recurrence, with annual clinical assessment, examination, and radiography of the chest and of the primary site of the disease [4,15]. We have followed our patient for 7 years after surgery and he does not have clinical and radiological evidence of local tumor recurrence or pulmonary metastasis. Our patient had extracompartmental sarcoma; Enneking stage IIB and hip disarticulation was performed. This corroborates the observation that limb salvage is contraindicated if there is pancompartmental disease and that ablative surgery in the form of amputation or disarticulation is indicated [13,15].
In medullary osteosarcoma of the femur, where there is extracomparmental disease with no distant metastasis, clinically and radiologically, radical tumor resection with a free oncological margin increases survival of the patient up to 7 years. Moreover, removal of the tumor with adequate free margins should be the primary consideration, as this has a positive effect on reducing the risk of local recurrence in medullary osteosarcoma of the femur. Furthermore, early radical surgery could be safe and effective in patients with medullary osteosarcoma of the femur.
In medullary osteosarcoma of the femur, removal of the tumor with adequate oncological margins should be the primary consideration and could improve survival.
References
- 1.Chen Z, Guo J, Zhang K, Guo Y. TP53 mutations and survival in osteosarcoma patients: A meta-analysis of published data. Dis Markers 2016;2016:4639575. [Google Scholar]
- 2.Gokgoz N, Wunder JS, Mousses S, Eskandarian S, Bell RS, Andrulis IL. Comparison of p53 mutations in patients with localized osteosarcoma and metastatic osteosarcoma. Cancer 2001;92:2181-9. [Google Scholar]
- 3.Li X, Zhang Y, Wan S, Li H, Li D, Xia J, et al. A comparative study between limb-salvage and amputation for treating osteosarcoma. J Bone Oncol 2016;5:15-21. [Google Scholar]
- 4.Messerschmitt PJ, Garcia RM, Abdul-Karim FW, Greenfield EM, Getty PJ. Osteosarcoma. J Am Acad Orthop Surg 2009;17:515-27. [Google Scholar]
- 5.Choi JH, Ro JY. The 2020 WHO classification of tumors of bone: An updated review. Adv Anat Pathol 2021;28:119-38. [Google Scholar]
- 6.Doyle LA. Sarcoma classification: An update based on the 2013 World Health Organization classification of tumors of soft tissue and bone. Cancer 2014;120:1763-74. [Google Scholar]
- 7.Sheng G, Gao Y, Yang Y, Wu H. Osteosarcoma and metastasis. Front Oncol 2021;11:780264. [Google Scholar]
- 8.Marko TA, Diessner BJ, Spector LG. Prevalence of metastasis at diagnosis of osteosarcoma: An international comparison. Pediatr Blood Cancer 2016;63:1006-11. [Google Scholar]
- 9.Li W, Xie P, Ruan WH. Overexpression of lncRNA UCA1 promotes osteosarcoma progression and correlates with poor prognosis. J Bone Oncol 2016;5:80-5. [Google Scholar]
- 10.Chen HJ, Lin CM, Lee CY, Shih NC, Peng SF, Tsuzuki M, et al. Kaempferol suppresses cell metastasis via inhibition of the ERK-p38-JNK and AP-1 signaling pathways in U-2 OS human osteosarcoma cells. Oncol Rep 2013;30:925-32. [Google Scholar]
- 11.Kager L, Zoubek A, Kastner U, Kempf-Bielack B, Potratz J, Kotz R, et al. Skip metastases in osteosarcoma: Experience of the Cooperative Osteosarcoma Study Group. J Clin Oncol 2006;24:1535-41. [Google Scholar]
- 12.Huang X, Zhao J, Bai J, Shen H, Zhang B, Deng L, et al. Risk and clinicopathological features of osteosarcoma metastasis to the lung: A population-based study. J Bone Oncol 2019;16:100230. [Google Scholar]
- 13.Tiwari A. Current concepts in surgical treatment of osteosarcoma. J Clin Orthop Trauma 2012;3:4-9. [Google Scholar]
- 14.Yang C, Tian Y, Zhao F, Chen Z, Su P, Li Y, et al. Bone microenvironment and osteosarcoma metastasis. Int J Mol Sci 2020;21:6985. [Google Scholar]
- 15.Hatori M, Hosaka M, Watanabe M, Moriya T, Sasano H, Kokubun S. Osteosarcoma in a patient with neurofibromatosis type 1: A case report and review of the literature. Tohoku J Exp Med 2006;208:343-8. [Google Scholar]