Patients with pre-existing distal radio ulnar joint malalignment who sustain a radial shaft fracture can have a clinical presentation similar to a Galeazzi fracture. If so, they can be managed successfully in a similar manner to a standard Galeazzi fracture.
Dr. Kenneth A Egol, NYU Langone Orthopedic Hospital, 301 E 17th Street, New York, NY, USA. E-mail: kenneth.egol@nyulangone.org
Introduction: Galeazzi fractures are fractures of the radial shaft accompanied by distal radioulnar joint (DRUJ) instability. They usually occur due to a mechanical fall or direct trauma to the wrist or forearm. Management of this serious injury varies from non-operative treatment with closed reduction and splinting to operative fixation using an external fixator (ex-fix) or open reduction internal fixation with plate and screws.
Case Report: We present a 76-year-old female who presented with a right distal radius fracture after a ground-level fall. Due to fracture displacement after initial conservative management, she was placed in an external fixator for stabilization. After removal of the ex-fix, she sustained a midshaft radius fracture with DRUJ malalignment, consistent with a “Galeazzi-like” fracture.
Conclusion: “Galeazzi-like” fractures with associated DRUJ malalignment can occur from previous external fixator pin sites and are adequately treated with standard operative fixation.
Keywords: Galeazzi-like fracture, ex-fix, distal radioulnar joint instability, nonunion.
Galeazzi fractures are uncommon indirect forearm injuries involving the combination of a fracture of the middle to distal ⅓ of the radial shaft and associated distal radioulnar joint (DRUJ) instability, depending on the distance of the fracture from the articular surface [1]. Approximately 7% of adults and 3% of children presenting with forearm fractures have a Galeazzi-like injury [2,3]. Although children with this injury may heal with nonoperative management such as cast immobilization following a successful closed reduction, adults require surgical intervention, commonly involving internal fixation of the radial fracture and anatomical reduction of the DRUJ with or without fixation [1,3,4]. Prior studies have revealed that, if treated as a simple radius fracture with closed reduction and immobilization, Galeazzi or Galeazzi-like fractures in adults may fail to fully heal and can develop a malunion and lead to long-term pain and reduced functional outcomes [4,5]. Patients with these injuries usually present with deformity, swelling, and pain localized to the fracture site, often following a fall from a height, sports-related injury, or acute trauma such as a motor vehicle accident [4]. The mechanism of injury typically involves a fall onto an outstretched hand with the forearm in pronation, and diagnosis is made based on clinical presentation and radiographic imaging [5]. Despite the complexity of the injury, stability and functional range of wrist and forearm motion may be restored when these fractures are identified early and treated [6]. Complications associated with the injury include DRUJ instability, increased risk of forearm compartment syndrome in high-energy injuries, neurovascular impairment, nonunion or malunion, and refracture [5].
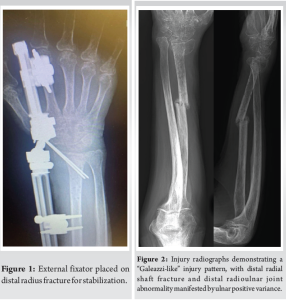
A 76-year-old female who was a former smoker with a history of osteopenia initially presented to the emergency department with right wrist pain after a ground-level fall at home the night before. She had a FRAX score of 11% for major osteoporotic fracture. She denied any history of cancer, radiation, long-term corticosteroid use, and Vitamin D deficiency. She denied loss of consciousness or any other injuries besides her wrist. X-ray of the right wrist taken in the ED revealed a “minimally displaced dorsally angulated fracture of the right distal radius.” She was then placed in a sugar-tong splint after closed reduction of her right wrist and advised to be non-weightbearing in the right upper extremity. After 2 weeks of immobilization, X-rays demonstrated further displacement of her fracture with no cortical bone consolidation. She was indicated for operative fixation of the distal radius fracture. At the time of surgery, the surgeon was unable to achieve adequate fixation with a plate due to poor bone quality and applied an external fixator with a K-wire for stabilization (Fig. 1). At 6-week postoperatively, the external fixator was removed in the office, and she was placed back into a removable splint.
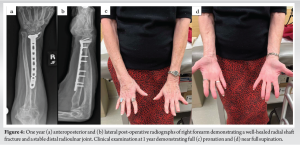
Three weeks later, an X-ray of the right forearm taken in clinic revealed that the distal radius was shortened and dorsally angulated, and there was a new midshaft radius fracture through the previous ex-fix pin site, with malalignment of the DRUJ (Fig. 2). Clinically, the patient was noted to be in full supination with no ability to pronate her wrist at all. The patient initially refused any intervention and was referred to another orthopedic surgeon 6 weeks following development of the “Galeazzi-like” fracture, characterized by misalignment of DRUJ due to her previous injury rather than typical DRUJ dislocation, distinguishing it from a true Galeazzi fracture. She was then indicated for surgery in the form of a right radial shaft nonunion repair with a closed, possible open reduction of the DRUJ. The patient underwent the proposed procedure through a volar approach, and the radius was fixed with a long pre-contoured volar locking plate and screws. An improved reduction of the DRUJ was afforded, despite residual dorsal tilt of the distal radius (Fig. 3). There was full restoration of forearm pronation and supination, and she was splinted in neutral forearm rotation.
Her post-operative course was unremarkable, and she remained neurovascularly intact with no wound dehiscence or further complications. She was followed at 6 weeks, 3 months, 6 months and 1 year postoperatively. Radiographic healing of the radial shaft fracture was completed by 6 months and confirmed 1 year following operative fixation. Full pronation and supination were also maintained at 1-year postoperatively (Fig. 4).
Management of distal radius fractures varies based on patient demographics, injury characteristics, and stability of the DRUJ [6]. However, the majority of low-energy distal radius fractures in the elderly can be managed nonoperatively [7,8]. On the other hand, almost all radial shaft fractures, such as Galeazzi or Galeazzi-like fractures, often require operative management to restore anatomic structure and function [2,4,9]. While these fractures requiring surgical intervention are frequently treated with open reduction and internal fixation, external fixation may be used acutely for fractures that present with significant soft-tissue injuries or compartment syndrome [6,10-14]. The use of external fixation for the treatment of displaced radial fractures involves the insertion of pins close to the fracture site and connected by a bridging bar. Although this method has fallen out of favor with the advent of improved volar locking plate technology, it is still used in certain situations [11-13]. It is an effective stabilization technique that requires minimal incisions and allows for a relatively quick return to normal functional range of motion [11]. However, complications occur in 20–85% of reported cases, involving pin-site infections and transient neuropraxias [4,11,12]. More minor complications, such as stiffness, can also occur with external fixator placement and other surgical treatment methods for distal radial fractures. While rare, cases of fractures through previously vacated ex-fix pin sites have been cited in the literature, more often in the lower extremity. A retrospective study of pediatric femur fractures treated with external fixation found that three patients out of 66 experienced a fracture at an ex-fix pin site; one patient developed a pin-site fracture within 1 week of ex-fix placement, while the other two experienced a fracture following ex-fix removal [11,15]. Refractures at the original fracture site occurred in five patients, two of whom completed strenuous physical therapy within 1 week of ex-fix removal [15]. While the authors were unable to identify specific risk factors associated with the three pin-tract fractures, it is possible that premature mobilization and strengthening may have played a role. The authors suggested that waiting for a longer period of time before ex-fix removal may decrease the incidence of pin-site fractures, particularly among young patients with few risk factor [15]. Another study by Wysocki et al. investigated femoral pin-site fractures in adults following computer-assisted total knee arthroplasty and suggested that the navigation pin placement created a significant defect in cortical bone, leading to a stress riser effect from localization of stress in a region of cortical bone [16]. While there are case reports on ulnar nerve injury and subacute elbow dislocation following Galeazzi fractures, there are no reports of a midshaft radius fracture at a previous ex-fix pin site leading to a “Galeazzi-like” injury in the literature [17-19]. Although a history of osteopenia and smoking can affect bone quality, as in our patient, and may be a risk factor for a secondary fracture at an ex-fix pin site, one study that compared ex-fix placement to stable plating for distal radius fractures in older adults found that an ex-fix was still a suitable treatment option even for patients with osteoporosis [4,6-8,10]. Given the high frequency of wrist external fixator use historically and the relative lack of this complication, one can assume a stress fracture through a previous ex-fix pin hole, leading to this injury pattern is extremely unusual [6,10-14]. While this insufficiency fracture may have been unavoidable secondary to the poor bone quality in this patient, it remains to be seen whether she would have been better served allowing her wrist to heal with a distal radius malunion and the resultant minimal functional deficits seen with that treatment despite a poor radiographic outcome. Ultimately, the use of standardized fixation techniques led to adequate bony healing and restoration of function.
This unusual “Galeazzi-like” fracture developed through an insufficiency fracture at a vacated ex-fix pin site in the setting of an already altered, although not dislocated, DRUJ, differentiating it from a true Galeazzi fracture pattern. Although unusual, fracture repair that re-established the normal radial bow of the forearm led to an excellent result.
Fractures through ex-fix pin sites have been reported in the literature, but none have occurred in the midshaft radius leading to a “Galeazzi-like” injury. This is clinically relevant and extremely unusual as external fixators have been used historically for years to treat fractures of the wrist, and this unique complication has never been encountered.
References
- 1.Alajmi T. Galeazzi fracture dislocations: An illustrated review. Cureus 2020;12:e9367. [Google Scholar]
- 2.Garg R, Mudgal C. Galeazzi injuries. Hand Clin 2020;36:455-62. [Google Scholar]
- 3.Eberl R, Singer G, Schalamon J, Petnehazy T, Hoellwarth ME. Galeazzi lesions in children and adolescents: Treatment and outcome. Clin Orthop Relat Res 2008;466:1705-9. [Google Scholar]
- 4.Giannoulis FS, Sotereanos DG. Galeazzi fractures and dislocations. Hand Clin 2007;23:153-63. [Google Scholar]
- 5.Rettig ME, Raskin KB. Galeazzi fracture-dislocation: A new treatment-oriented classification. J Hand Surg Am 2001;26:228-35. [Google Scholar]
- 6.Biz C, Cerchiaro M, Belluzzi E, Bortolato E, Rossin A, Berizzi A, et al. Treatment of distal radius fractures with bridging external fixator with optional percutaneous K-wires: What are the right indications for patient age, gender, dominant limb and injury pattern? J Pers Med 2022;12:1532. [Google Scholar]
- 7.Cooper AM, Wood TR, Scholten Ii DJ, Carroll EA. Nonsurgical management of distal radius fractures in the elderly: Approaches, risks and limitations. Orthop Res Rev 2022;14:287-92. [Google Scholar]
- 8.Luokkala T, Laitinen MK, Hevonkorpi TP, Raittio L, Mattila VM, Launonen AP. Distal radius fractures in the elderly population. EFORT Open Rev 2020;5:361-70. [Google Scholar]
- 9.Takemoto R, Sugi M, Immerman I, Tejwani N, Egol KA. Ulnar variance as a predictor of persistent instability following Galeazzi fracture-dislocations. J Orthop Traumatol 2014;15:41-6. [Google Scholar]
- 10.Gausepohl T, Worner S, Pennig D, Koebke J. Extraarticular external fixation in distal radius fractures pinplacement in osteoporotic bone. Injury 2001;32:SD79-85. [Google Scholar]
- 11.Capo JT, Swan KG Jr., Tan V. External fixation techniques for distal radius fractures. Clin Orthop Relat Res 2006;445:30-41. [Google Scholar]
- 12.Gradl G, Gradl G, Wendt M, Mittlmeier T, Kundt G, Jupiter JB. Non-bridging external fixation employing multiplanar K-wires versus volar locked plating for dorsally displaced fractures of the distal radius. Arch Orthop Trauma Surg 2013;133:595-602. [Google Scholar]
- 13.Krukhaug Y, Ugland S, Lie SA, Hove LM. External fixation of fractures of the distal radius: A randomized comparison of the Hoffman compact II non-bridging fixator and the Dynawrist fixator in 75 patients followed for 1 year. Acta Orthop 2009;80:104-8. [Google Scholar]
- 14.Konrads C, Schewior T. Delayed treatment of a Galeazzi fracture using an external ring fixator. J Orthop Case Rep 2020;10:47-9. [Google Scholar]
- 15.Skaggs DL, Leet AI, Money MD, Shaw BA, Hale JM, Tolo VT. Secondary fractures associated with external fixation in pediatric femur fractures. J Pediatr Orthop 1999;19:582-6. [Google Scholar]
- 16.Wysocki RW, Sheinkop MB, Virkus WW, Della Valle CJ. Femoral fracture through a previous pin site after computer-assisted total knee arthroplasty. J Arthroplasty 2008;23:462-5. [Google Scholar]
- 17.Asadollahi S, Shepherd D, Hau RC. Elbow fracture-dislocation combined with Galeazzi fracture in adult: A case report and literature review. Int J Surg Case Rep 2013;4:748-52. [Google Scholar]
- 18.Rajeev A, Senevirathna S, Harrison J. Subacute dislocation of the elbow following Galeazzi fracture-dislocation of the radius: A case report. J Med Case Rep 2011;5:589. [Google Scholar]
- 19.Roettges P, Turker T. Ulnar nerve injury as a result of Galeazzi fracture: A case report and literature review. Hand (N Y) 2017;12:NP162-5. [Google Scholar]