Posterior interosseous nerve palsies can occur in the presence of an anterior congenital radial head dislocation in an adult.
Dr. Keiichi Muramatsu, Department of Orthopedic Surgery, Nagato General Hospital, Yamaguchi, Japan. E-mail: kemuramatsu@outlook.jp
Introduction: Anterior congenital radial head dislocation (CRHD) is a rare abnormality that is less commonly seen in the adult population. Most of the time, adult-onset symptoms are due to the prolonged dislocation of the radiocapitellar joint that has been present since birth. One of the possible complications of having a prolonged radial head dislocation is the presence of neuropathies such as posterior interosseous nerve (PIN) palsy. There has been, however, no literature published regarding the relationship of CRHD with PIN palsy.
Case Report: We here report a 66-year-old male incidentally diagnosed with anterior CRHD with concomitant PIN palsy after acquiring a fracture of the lateral humeral condyle. Open reduction internal fixation of the lateral condyle was done along with decompression of the said nerve. PIN palsy was completely recovered 2 months after surgery.
Conclusion: Surgeons must be aware that PIN palsies can occur in the presence of a chronic radial head dislocation, even if asymptomatic. Prompt nerve decompression as well as removal of the mechanical block is pertinent to avoid the perilous effects of an irreversible PIN palsy.
Keywords: Congenital radial head dislocation, posterior interosseous nerve palsy, neurolysis, fracture.
Congenital radial head dislocation (CRHD) is very rare, but it remains to be the most common abnormality of the elbow [1, 2]. CRHD patients are frequently asymptomatic in the early years and are only diagnosed once children have complaints of pain or limited elbow motion [2]. Since most often these dislocations arise in childhood, adult-onset CRHD symptoms are less common. It is believed that adult-onset symptoms can be attributed to a chronic radiocapitellar dislocation [2]. Sequelae of a prolonged radiocapitellar dislocation may include elbow instability, osteoarthritis, or neuropathy by affecting its surrounding structures. As the radial head can be seen in proximity with the posterior interosseous nerve (PIN), nerve injury may occur once a dislocated radial head impinges the nerve along the tough fibers of the supinator arch found anterior to the PIN [2-4]. At present, there is no literature available with regard to the association of CRHD to PIN palsy. In this paper, we will discuss a case of an anterior CRHD with the possibility of having a concomitant PIN palsy.
This is a case of a 66-year-old male presenting with a 3-day history of falls on an outstretched right hand. The patient reported progressive worsening of pain in his right elbow accompanied by the difficulty in finger extension. Before this, the patient had no complaints regarding his right elbow and could even do difficult manual labor. He had no relevant familial history or other congenital abnormalities. On physical examination, there was swelling and tenderness on the lateral aspect of the right elbow around the lateral condyle. Flexion and extension of the right elbow were limited to 90° and −20°, respectively. On the other hand, the contralateral elbow had a flexion and extension of 130° and −10°, respectively. The patient had full pronosupination in both extremities and had no sensory deficits. Manual muscle testing (MMT) for the right wrist dorsiflexion was at 5/5, while the extensor pollicis longus (EPL), extensor indicis proprius (EIP), extensor digitorum communis (EDC) and extensor digiti minimi (EDM) had an MMT score of 0/5 (Fig. 1a).
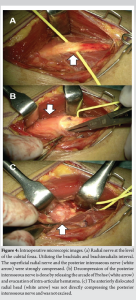
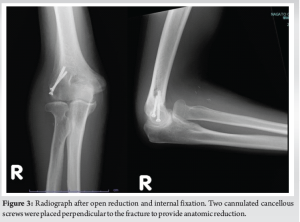
Radiographs for both elbows were taken and revealed a 2 mm fracture line over the right lateral condyle (Fig. 2). Incidentally, images revealed bilateral dome-shaped radial heads with subsequent anterior displacement, suggesting a congenital origin (Fig. 2) [5, 6]. The patient was diagnosed with a lateral condylar fracture with intra-articular hematoma, anterior CRHD, and PIN palsy of the right probably secondary to the radial head dislocation. Open reduction internal fixation for the lateral condyle fracture, nerve decompression, and possible radial head excision were proposed for this case to improve the patient’s symptomatology. A small linear incision was made over the lateral epicondyle and the triceps was lifted subperiosteally to identify the fracture line. Two cannulated cancellous screws were then placed perpendicular to the fracture to provide anatomic reduction (Fig. 3). Another incision was created distal to the cubital fossa through the brachialis and brachioradialis muscle interval. Under microscope visualization, the radial nerve was carefully identified and dissected until it bifurcated into the superficial radial nerve and the PIN (Fig. 4a). A large hematoma was found intra-articularly. After sufficient evacuation of the hematoma, PIN decompression was done by releasing the arcade of Frohse and dividing it until the origins of the extensor carpi radialis brevis muscle (Fig. 4b). Intra-operative re-evaluation noted that the radial head was not compressing the PIN, hence, the decision to do the radial head excision was abandoned (Fig. 4c).
One week post-surgery, the EDC, EIP, and EDM have recovered with an MMT score of 2/5; however, the EPL remained to have a 0/5 score. MMTs 1-month post-surgery were the following: EPL 2/5, EIP 3/5, EDC 4/5, and EDM 3/5. At 2 months post-surgery, MMTs for all finger extensors recovered to 5/5, except for the EIP which still had an MMT of 4/5. Moreover, at 4-months post-surgery, the MMT of the EIP was 5/5 (Fig. 1b). The patient had no other complaints and the elbow range of motion was comparable to the contralateral side.
CRHD
Even with a low incidence of 0.06–0.16%, CRHD is still believed to be one of the most common causes of elbow abnormalities. CRHDs usually go undetected and are only diagnosed once symptoms such as pain or limited elbow motion occur in a child [2]. Since CRHDs are considered rare occurrences, a set of criteria has been established to help diagnose such conditions. The criteria, as proposed by Mardam–Bey and Ger, include the following: (1) bilateral involvement, (2) associated congenital anomalies, (3) familial occurrence, (4) no history of trauma, (5) irreducibility by closed maneuver, and (6) dislocation present at birth [5]. There seems to be a paucity of cases published about CRHDs diagnosed in adults. In a literature review done by Gao et al. [2], only nine cases of CRHD were reported worldwide. Reasons for such rarity may be due to the conditions delayed or non-diagnosis, because of its relative tolerability and unimpaired patient function due to minimal loss of motion or the compensatory wrist and shoulder motion [5, 7]. The chronicity of the dislocation since childhood can then make the radioulnar joint unstable leading to osteoarthritis or other neuropathies.
PIN palsy and CRHD
The radial nerve terminates and branches off as the superficial radial nerve and PIN after passing through the taut fibers formed by the Arcade of Frohse [8]. This structure is considered a tough connective tissue spanning from the tip of the lateral epicondyle to the medial aspect of the lateral epicondyle, just lateral to the articular surface of the capitellum [6]. As this nerve passes through this tough connective tissue, it moves distally in between to two heads of the supinator muscle and then wraps around the radial neck posteriorly [8, 9]. Until now, there has been no case reports of CRHD associated with PIN palsy, or intra-articular elbow hematoma causing the said paralysis. The researchers hypothesized that this could have occurred mainly due to the close relationship of PIN to the radial head and its surrounding structures [3]. CHRD pathogenesis may be similar to chronic radial head dislocation from an undiagnosed Monteggia fracture during childhood. The chronic radiocapitellar dislocation stretches the PIN causing compression overtime inside the arcade of Frohse [10]. Furthermore, the excessive repeated motion with loss of elasticity of the surrounding tissues because of long-term dislocation of the radial head may cause delayed PIN palsy [11]. Nerve injuries may occur even without an apparent transection. A compression of a nerve may cause it to undergo ischemia that could show similar clinical findings [8]. Especially in PIN palsies, compression along the thickened Arcade of Frohse can present with symptoms of weakness in finger extensors [9]. In our case, the presence of an intra-articular elbow hematoma on top of a chronic anteriorly displaced radial head could have further compressed PIN leading to the patient’s symptomatology.
Treatment options for our unique case
At present, there is no consensus on the treatment of CRHD. The spectrum ranges from observation to surgical interventions. However, the patient’s symptomatology serves as a guiding principle toward proper management [12]. Surgery is indicated when a patient has any pain, loss of elbow motion, neuropathies, or it is not cosmetically acceptable. Surgical options include radial head excision or osteotomies to contain the radiocapitellar joint [12]. Close observation for a total of 6 weeks may be done initially if there seems to be no apparent cause, leading to nerve compression [1,8]. During this time, patients may undergo physiotherapy, activity modifications, or wearing of orthotic braces to hasten the nerve’s recovery [13]. However, when a mechanical compression of the nerve is considered, or if 6 weeks of observation yielded no improvement, nerve exploration and neurolysis should be considered. Urgent decompression of the nerve is warranted to prevent the irreversible effects of the space-occupying lesion on the nerve. In the case presented above, radial head excision was no longer done since sufficient hematoma evacuation, as well as neurolysis, adequately decompressed the PIN. Moreover, at 4-month follow-up, the patient had full motor recovery of his finger extensors further supporting the decision to forgo additional surgical interventions. This also spared the patient of the possible complications of radial head excision such as proximal radial migration, synostosis instability, valgus deformity, and weakness [1, 2, 12].
Until now, there has been no literature available on CRHD is associated with PIN palsy. This paper is the first case report to show that CRHD can cause PIN palsy. Early neurolysis is recommended to resolve PIN palsy.
Surgeons must be aware that PIN palsies can occur in the presence of a CRHD, even if asymptomatic. Prompt nerve decompression as well as removal of the mechanical block are pertinent to avoid the perilous effects of an irreversible PIN palsy.
References
- 1.Kaas L, Struijs PA. Congenital radial head dislocation with a progressive cubitus valgus: A case report. Strategies Trauma Limb Reconstr 2012;7:39-44. [Google Scholar]
- 2.Gao J, Tang J, Li M, Li H, Peng Y, Wang C, et al. Bilateral anterior congenital radial head dislocation in adults: A case report and literature review. Front Surg 2023;10 1155461. [Google Scholar]
- 3.Tubbs RS, Griessenauer C, Rizk E, Shoja MM, Pehler SF, Wellons JC, et al. Posterior Interosseous nerve palsy in a child associated with recurrent dislocation of the head of the radius. J Neurosurg Pediatr 2013;11:389-91. [Google Scholar]
- 4.Holst-Nielsen F, Jensen V. Tardy posterior interosseous nerve palsy as a result of an unreduced radial head dislocation in Monteggia fractures: A report of two cases. J Hand Surg Am 1984;9:572-5. [Google Scholar]
- 5.Mardam-Bey T, Ger E. Congenital radial head dislocation. J Hand Surg Am 1979;4:316-20. [Google Scholar]
- 6.Kim HT, Conjares JN, Suh JT, Yoo CI. Chronic radial head dislocation in children, part 1: pathologic changes preventing stable reduction and surgical correction. J Pediatr Orthop 2022;22:583-90. [Google Scholar]
- 7.Kelly DW. Congenital dislocation of the radial head: Spectrum and natural history. J Pediatr Orthop 1981;1:295-8. [Google Scholar]
- 8.Sigamoney KV, Rashid A, Ng CY. Management of atraumatic posterior interosseous nerve palsy. J Hand Surg Am 2017;42:826-30. [Google Scholar]
- 9.Spinner M. The arcade of Frohse and its relationship to posterior interosseous nerve paralysis. J Bone Joint Surg Br 1968;50:809-12. [Google Scholar]
- 10.Martinelli F, Celli A, Celli L. Belated posterior interosseous nerve palsy with chronic radial head dislocation: A case report. JSES Rev Rep Techn 2024;4:324-7. [Google Scholar]
- 11.Cho C, Lee K, Min B. Tardy posterior interosseous nerve palsy resulting from residual dislocation of the radial head in a Monteggia fracture. J Med Case Rep 2009;3:9300. [Google Scholar]
- 12.Bengard MJ, Calfee RP, Steffen JA, Goldfarb CA. Intermediate-term to long-term outcome of surgically and nonsurgically treatment congenital, isolated radial head dislocation. J Hand Surg Am 2012;37:2495-501. [Google Scholar]
- 13.Cravens G, Kline D. Posterior interosseous nerve palsies. Neurosurgery 1990;27:397-402. [Google Scholar]