Debridement, sequestrectomy, and antibiotics are considered standard treatments for chronic osteomyelitis, but they may not be sufficient in some cases, especially in rare instances of rib osteomyelitis. Resection of ribs can be considered a definitive surgical option in such situations, as it would not hamper the function of the rib cage, unlike resection of long bones, which would affect limb function.
Dr. Abhishek Kothari, Department of Orthopaedics, Sancheti Institute for Orthopaedics and Rehabilitation, Pune, Maharashtra, India. E-mail: dr.abhishekkothari@gmail.com
Introduction: Chronic osteomyelitis of the ribs in adolescents and adults is a rare condition. Current understanding of its diagnosis and management is primarily derived from case reports and small series studies. Here, we present a case of chronic rib osteomyelitis initially managed conservatively with antibiotics, followed by debridement, sequestrectomy, and continued antibiotic therapy. However, due to recurrence, rib excision was ultimately chosen as the definitive management approach.
Case Report: A 18-year-old male presents with a discharging sinus from the chest persisting for 6 months, with no history of fever, shivering, or weight loss. He sustained a blunt injury to the chest with a bamboo stick 9 months ago. Initially, the patient was treated with antibiotics, but there was no relief. He was later operated on with debridement, sequestrectomy, and antibiotics. Six weeks later, he again presented to us with a discharging sinus. Due to recurrence, he underwent re-operation with partial resection of the 6th rib. At the 1-year follow-up after rib excision, the patient is doing well, with all blood parameters within the normal range and without any systemic or local complications.
Conclusion: Rib osteomyelitis is a rare complication of blunt chest trauma. Surgical management is indicated in cases of persistent infection. Sequestrectomy and antibiotics, though standard procedures in chronic osteomyelitis, may encounter failure due to various factors. Moreover, due to limited literature on chronic osteomyelitis of ribs, the standard approach to its management is not available. Partial excision of the rib with appropriate antibiotics in our case provided complete cure for the patient.
Keywords: Recurrent osteomyelitis, ribs, bamboo stick injury, blunt trauma, rib excision.
Chronic osteomyelitis is less common compared to acute osteomyelitis [1]. Moreover, chronic osteomyelitis of the ribs is an even rarer entity. Dich et al., reviewed 163 cases of osteomyelitis in children over a span of 15 years and found that chronic osteomyelitis occurred in only 19% of the cases, with only a single case (0.6%) affecting the ribs [2]. Thus, historical data on rib osteomyelitis in young adults are limited due to its infrequent occurrence. Ongoing research is crucial to refine our understanding of the epidemiology, etiology, and management of this rare condition among young adults. We report a case of an 18-year-old male with recurrent chronic pyogenic osteomyelitis of the ribs due to a bamboo stick injury, which was treated with partial resection of the rib as definitive surgical management. In this unique case report, we aim to contribute valuable insights to the medical community about rib osteomyelitis and enhance our ability to diagnose and treat such cases effectively.
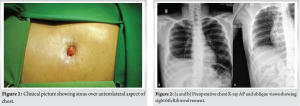
An 18-year-old male presented with swelling and a discharging sinus since 6 months from the anterolateral aspect of the right chest wall (Fig. 1). The patient had a history of trauma involving a bamboo stick to the right chest 9 months prior, which was initially managed conservatively at a local hospital. Since then, the patient experienced intermittent chest pain, followed by the onset of wound discharge. There were no reported major medical illnesses or significant weight loss.
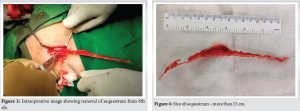
On examination, swelling and redness were observed on the anterolateral aspect of the right chest around the level of the 6th rib, accompanied by a discharging sinus with granulated margins. Regional lymph nodes were not enlarged, and there were no positive findings on respiratory and cardiovascular examination. Blood investigations revealed a total leukocyte count of 11,020/Cumm, an erythrocyte sedimentation rate (ESR) of 2 mm/h, and a C-reactive protein level (CRP) of 2.24 mg/L. Despite the blood parameters being within normal limits, a diagnostic dilemma arose. X-rays of the chest in PA and oblique views (Fig. 2) revealed a lytic lesion in the right 6th rib with irregular sclerotic bone surrounded by a radiolucent rim. A computed tomography (CT) scan of chest suggested sclerosis with erosion of the anterior end of the right 6th rib with minimal associated adjacent right pleural thickening. The patient underwent surgery. Under a supine position, a 3 cm linear incision was made over the 6th rib. An unusually long sequestrum measuring more than 15 cm (Fig. 3 and 4) was removed, along with debridement and excision of the sinus tract. Intraoperative tissue samples were sent for further evaluation. Gram stain showed occasional neutrophils but no organisms were seen. Acid-fast bacilli were not detected on ZN stain. Tissue culture revealed growth of Methicillin Resistant Staphylococcus aureus. The histopathology report suggested acute on chronic inflammatory granulation tissue. Postoperatively, oral Tab. Linezolid 600 mg twice a day was initiated and continued for 6 weeks as per the drug sensitivity. Sutures were removed after 15 days and the wound was found to be healthy.
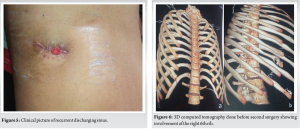
On the 6-week follow-up visit, the patient again presented with discharge from wound. It was managed with oral antibiotics on an outpatient basis for the next month. The patient continued to experience intermittent discharge from the wound thereafter (Fig. 5).
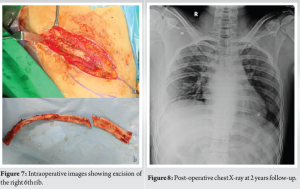
After 8 months from the primary surgery, a 3D CT scan was performed, revealing persistent bony sclerosis with erosion involving the right 6th rib (Fig. 6). Definitive surgery was planned. This time, a longer incision of approximately 12 cm was made over the right 6th rib. Partial resection of the right 6th rib was performed (Fig. 7) to eliminate any foci of infection. Intraoperative samples were sent for further investigations. Methicillin-sensitive S. aureus was detected on tissue culture and sensitivity testing. Accordingly, oral Linezolid 600 mg and Cefuroxime axetil 500 mg were initiated and continued for 6 weeks. Sutures were removed after 3 weeks, and the wound appeared healthy. There were no complaints of discharge or any other issues during regular follow-ups. Inflammatory markers (white blood cell count, ESR, and CRP) remained within normal limits.
At the end of 2 years, follow-up X-rays showed no evidence of recurrence (Fig. 8), and there was a well-healed scar (Fig. 9) with no signs of disease recurrence or any local and systemic complaints.
Although chronic osteomyelitis of the ribs is rare, it has been described in association with tuberculosis (TB), through hematogenous spread [3, 4]. Osinowo et al. reported 16 patients with rib osteomyelitis and found that blunt chest trauma was responsible for only 3 out of 16 reported cases. The most common cause was empyema thoracis (9 out of 16 patients) due to the use of wide and stiff intercoastal drainage chest tubes in their cardio-thoracic unit. The mean age was 9.32 years, with only 3 out of 16 patients being adults over 18 years of age [5]. Thus, chronic rib osteomyelitis is a rare disease, with its occurrence in young adults around 18 years of age being the least common. Further review of the literature reveals that rib osteomyelitis is more common in children, whereas our patient was a young adult. The usual clinical presentation in rib osteomyelitis includes fever associated with chest pain, discharging sinus, and raised inflammatory markers. In contrast, our patient presented with only a chronic discharging sinus, without fever, raised inflammatory markers, or any other pulmonary symptoms. Common causes of rib osteomyelitis include contiguous infection (e.g., pneumonia or empyema thoracis), hematogenous spread from distant infection foci, chest trauma (penetrating or blunt), and iatrogenic procedures. A possible explanation for the development of rib osteomyelitis in our case may be antecedent blunt chest injury from a bamboo stick, leading to hematoma formation that became infected, subsequently leading to infection and the development of osteomyelitis. Osteomyelitis due to hematogenous spread occurs in areas with a rich blood supply where bone is metabolically more active. Such metabolically active sites in the rib include the costochondral junction anteriorly (76%) and the costovertebral angle posteriorly [6]. In our case, the site of infection was the anterolateral part of the 6th rib, which is again an unusual site of disease involvement, reducing the likelihood of hematogenous spread from any probable distant foci. Due to the unusual site of presentation and normal inflammatory markers, a differential diagnosis becomes more important in such cases. There should be a high degree of suspicion for TB, considering the patient is from an endemic region. Other differential diagnoses to consider in such situations are chronic nonspecific osteomyelitis of the rib, rib involvement following empyema necessitans, eosinophilic granuloma, syphilis, and tumors (benign and malignant). Benign tumors affecting the ribs include chondroma (the most common), osteochondroma, fibrous dysplasia, and lipoid granuloma. Malignant conditions include chondrosarcoma, multiple myeloma, and secondary metastases from lung, breast, liver, and kidney [7]. In this case, the patient was a young adult with a history of blunt trauma leading to chronic osteomyelitis, with recurrence even after surgical management. Since the standard treatment, involving removal of necrotic bone (sequestrectomy), incision and drainage of the abscess, with bone curettage and debridement [8, 9], was already performed, there was a dilemma about the way ahead. As mentioned before, due to the rarity of the disease, the standard management protocol of chronic rib osteomyelitis is not available.
After a review of the literature, one or more of the following factors could be responsible for recurrence in this case:
- Inadequate debridement
- Reinfection at the same site, rather than a relapse of infection
- Inadequate antibiotic therapy
- Multi-drug-resistant nature of the organism isolated after the first surgery
- Failure to involve an infectious disease specialist opinion, even in cases of multi-drug resistance.
Due to the close proximity to vital parts such as the pleura, neurovascular bundles, lung parenchyma, etc., it is difficult to be aggressive while doing the debridement of ribs. Moreover, constant movement of ribs due to respiration hinders the healing process. Hence, the more extensive debridement during the first surgery could have been more beneficial. Uçkay et al. [10], in their study, suggested the possibility of re-infection with different strains, rather than reactivation of dormant infection. They suggested that the bone once infected becomes a vulnerable area for bacterial adhesion and when transient bacteremia occurs due to any reason, it can lead to re-infection at the same site. This theory strongly resembles the established relationship of altered valvular surfaces and infectious endocarditis, adding to the popular belief that once bone is infected, it remains infected forever. Here, we need to understand this basic difference between the term “relapse,” which means recurrence with the same organism, whereas the term “re-infection” means recurrence with a different or additional strain of organisms. As mentioned above, after the first debridement, mono-drug therapy with only linezolid was advised to the patient. As linezolid is mostly a bacteriostatic drug, its adequacy to treat chronic infections as a single drug is questioned. After the second surgery, we adopted two-drug therapy (linezolid and cefuroxime), which gave us a good outcome. Subramanyam et al. [11] compared 20 studies on chronic osteomyelitis reporting the recurrence rate after surgical debridement. They found out that systemic antibiotics along with local antibiotics significantly reduce the recurrence of infection. This newer technique of using antibiotics loaded calcium sulfate pellets could have been thought about at the time of the first surgical debridement for a better outcome. Arias et al. conducted an interesting study on 129 patients with chronic osteomyelitis and concluded that patients treated by an orthopedist alone had a higher recurrence rate, whereas multidisciplinary management with the involvement of an infectious disease specialist along with an orthopedist increases the cure rates and decreases the likelihood of relapses [12].
Rib osteomyelitis is a rare complication of blunt chest trauma. Surgical intervention is indicated in cases of persistent infection. Sequestrectomy and antibiotics, though standard procedures in chronic osteomyelitis, may encounter failure due to various factors. Moreover, due to limited literature on chronic osteomyelitis of ribs, the standard approach to its management is not available. Partial excision of the rib with appropriate antibiotics in this case provided a complete cure to the patient.
All bone infections, especially chronic rib osteomyelitis cases, should be treated with a holistic approach, as the widely practiced protocol of sequestrectomy and debridement may not be sufficient. Involvement of specialists from allied branches and the use of newer techniques like antibiotic-loaded calcium sulfate beads can result in a better outcome.
References
- 1.Auh JS, Binns HJ, Katz BZ. Retrospective assessment of subacute or chronic osteomyelitis in children and young adults. Clin Pediatr (Phila) 2004;43:549-55. [Google Scholar]
- 2.Dich VQ, Nelson JD, Haltalin KC. Osteomyelitis in infants and children. A review of 163 cases. Am J Dis Child 1960 1975;129:1273-8. [Google Scholar]
- 3.Nibley PD, Kraus CK. Rib osteomyelitis in a pediatric patient: Case report and review of the literature. Clin Pract Cases Emerg Med 2018;2:294-6. [Google Scholar]
- 4.Bishara J, Gartman-Israel D, Weinberger M, Maimon S, Tamir G, Pitlik S. Osteomyelitis of the ribs in the antibiotic era. Scand J Infect Dis 2000;32:223-7. [Google Scholar]
- 5.Osinowo O, Adebo OA, Okubanjo AO. Osteomyelitis of the ribs in Ibadan. Thorax 1986;41:58-60. [Google Scholar]
- 6.Nascimento M, Oliveira E, Soares S, Almeida R, Espada F. Rib osteomyelitis in a pediatric patient case report and literature review. Pediatr Infect Dis J 2012;31:1190-4. [Google Scholar]
- 7.Agrawal V, Joshi MK, Jain BK, Mohanty D, Gupta A. Tuberculotic osteomyelitis of rib--a surgical entity. Interact Cardiovasc Thorac Surg 2008;7:1028-30. [Google Scholar]
- 8.Urish KL, Cassat JE. Staphylococcus aureus osteomyelitis: Bone, bugs, and surgery. Infect Immun 2020;88:e00932-19. [Google Scholar]
- 9.Mboutol-Mandavo C, Monka M, Moyikoua RF, Ondima IP, Miéret JC. Osteomyelitis of flat bones: A report of 20 cases and review of the literature. J Clin Orthop Trauma 2019;10:1116-20. [Google Scholar]
- 10.Uçkay I, Assal M, Legout L, Rohner P, Stern R, Lew D, et al. Recurrent osteomyelitis caused by infection with different bacterial strains without obvious source of reinfection. J Clin Microbiol 2006;44:1194-6. [Google Scholar]
- 11.Subramanyam KN, Mundargi AV, Prabhu MV, Gopakumar KU, Gowda DS, Reddy DR. Surgical management of chronic osteomyelitis: Organisms, recurrence and treatment outcome. Chin J Traumatol 2023;26:228-35. [Google Scholar]
- 12.Arias CA, Betancur MC, Pinzón MA, Arango DC, Taffur CA, Prada EC. Differences in the clinical outcome of osteomyelitis by treating specialty: Orthopedics or infectology. PLoS One 2015;10:e0144736. [Google Scholar]