Glomus tumors are rarely found in the foot and even less so in the lesser toes; thus, diagnostic suspicion and careful review of imaging is paramount to reduce missing this diagnosis
Dr. Shaun Wei Kang Koo, Barts and The London School of Medicine and Dentistry, Queen Mary University of London, Garrod Building, Turner St, London E1 2AD. E-mail: shaun.koowk@gmail.com
Introduction: Glomus tumors are rare, benign neoplasms that originate from glomus bodies. While usually occurring in the subungual regions of the fingers, glomus tumors are seldom found in the foot, although rare reports have been made of glomus tumors in the hallux and even fewer in the lesser toes. We describe a reported case of a glomus tumor occurring in the distal phalanx of the left second toe that was initially missed on imaging studies, resulting in delayed diagnosis and surgical treatment. To the best of our knowledge, this represents one of the first few cases of glomus tumor reported in the lesser toes.
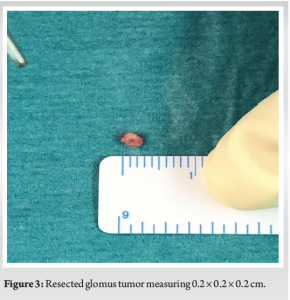
Case Report: A 34-year-old Chinese female presented with pain in the left second toe occurring for several years. Initial assessment and radiological investigations came back negative for abnormalities, resulting in delayed treatment. Upon second opinion of the MRI scans, a 0.2 × 0.2 × 0.2 cm well-defined round enhancing high T2-weighted signal focus within the germinal matrix of the left second toe subungual region was found, suggestive of a glomus tumor. Surgical exploration was offered, which found a skin-colored lesion, which was resected using a transungual approach. The final histology of the excised mass showed perivascular proliferation of uniform cells which contained round to ovoid nucleus with small nucleolus and pale eosinophilic cytoplasm, confirming glomus tumor.
Conclusion: Glomus tumors are rarely found in the foot, with even fewer reports in the lesser toes. Their rare occurrence in these regions reduces diagnostic suspicion for these tumors, delaying diagnosis and treatment for patients. This case report highlights the difficulty in diagnosing glomus tumors, even with adequate radiological investigations, and showcases the need for careful scrutinization of imaging. As this presentation is extremely uncommon, we hope that this case report increases suspicion of glomus tumors as a differential diagnosis for toe pain to ensure early treatment and alleviation of symptoms for patients.
Keywords: Glomus tumor, toe pain, subungual
A glomus tumor is a rare, usually benign neoplasm that originates from glomus bodies, specialized arteriovenous structures in the dermis responsible for thermoregulation by shunting blood to and from the skin [1]. They consist of an afferent arteriole, a venule, and an anastomotic vessel lined by actin-containing glomus cells [2]. The high concentration of glomus bodies in the digits, particularly in the fingertips and subungual areas, explains the anatomical tendency for glomus tumors to be found at the distal regions of the digits [3]. This type of tumor can be found anywhere in the body, with the subungual regions of the hand being the most common site of presentation [4]. Considering the anatomical similarities between the toes and the fingers, it is surprising that glomus tumors do not usually occur in the foot. There have only been a few reports of glomus tumors occurring in the hallux [3, 5-8], with even fewer reports in the lesser toes [9-12]. Recently, there has even been a report of simultaneous glomus tumors in the third and fourth toes [10]. This case report follows a 34-year-old Chinese female who was diagnosed with a glomus tumor found in the subungual area of the left second toe that was initially missed on radiological imaging. Due to its uncommon presentation in this region, it could be of value to share these findings. We hope that this case report adds to a growing body of evidence to increase suspicion for glomus tumors in the lesser toes, in turn promoting careful review of imaging and increasing diagnostic yield.
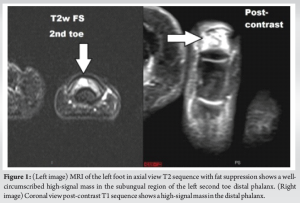
This case report follows a 34-year-old Chinese female who presented with pain in the left second toe that started a few years ago. The patient reported experiencing “throbbing” in the affected toe several times a day, as well as during the nighttime, which was occurring for a few months. On clinical examination, there was exquisite point tenderness on palpation of the left second toe distal phalanx. There was no intermetatarsal space tenderness or Mulder’s click. The patient had seen a neurologist prior for her symptoms. The X-rays and MRI scans of the foot done then were reported as normal. However, on consultation with our senior author, he noted a signal-enhancing lesion in the distal phalanx of the left second toe from the MRI T2 sequences, which was missed on initial review. Following this, the MRI films were sent for a second opinion by a musculoskeletal radiologist (Fig. 1).
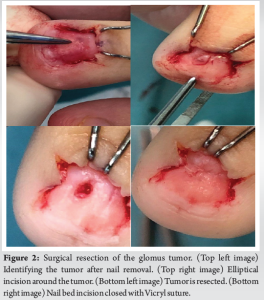
The MRI of the left foot was taken in the axial, sagittal, and coronal planes with T1-weighted and T2-weighted images with fat suppression acquired. Contrast sequences were also taken. The MRI reported back a 0.2 × 0.2 × 0.2 cm well-defined round enhancing high T2-weighted signal focus within the central portion of the germinal matrix in the left second toe subungual region. No bony scalloping or edema was noted in the adjacent distal phalanx. From the second report, in the context of the clinical findings, the imaging findings were suspicious for a glomus tumor. Suspecting a glomus tumor as the diagnosis, surgical resection was offered to the patient. The risks of the surgery were explained to the patient, including the risk of nail dystrophy, failure of nail growth, and soft-tissue defects needing further resurfacing. We proceeded with surgical excision, using a trans-ungual approach to access the tumor. Through this approach, the entire nail plate of the second toe was removed to expose the underlying nail bed, which showed a skin-colored lesion centrally located in the nail bed. We were able to successfully remove the entire mass (Fig. 2).
Surgery was performed under local anesthesia with the use of a rubber band tourniquet. The nail was removed to expose the nail bed. The mass within the nail bed at the junction of the sterile and germinal matrix was then excised in an elliptical fashion for histopathological examination. The nail bed incision was then repaired with an absorbable 6.0 Vicryl suture to reduce the risk of nail dystrophy. After a copious wash of the nail bed region, the nail was reinserted on the nail bed as a protecting layer (Fig. 3).
Histopathology results confirmed the diagnosis of glomus tumor. The specimen on microscopy revealed composition of a perivascular proliferation of uniform cells which contained round to ovoid nucleus with small nucleolus and pale eosinophilic cytoplasm. The surrounding stroma showed myxoid change. No cytological atypia, mitosis, or necrosis was seen. The patient was followed up at 1-week, 2-week, 6-week, 3-month, and 1-year post-surgery. At 1-week post-operation, the wound was found to be clean and dry. At 2-weeks, the patient still reported experiencing mild throbbing pain, but was otherwise well. On examination, the wound had healed, and the nail was no longer tender, 6-week post-surgery, the patient was no longer experiencing any throbbing pain and informed us that the nail had fallen off a week prior. Further inspection showed that the nail bed had healed with a dry scab. A toe sock was provided from podiatry to alleviate any discomfort. After 3-month post-operation, the nail had regrown and at 1-year post-surgery, there was no recurrence of pain or discomfort. No nail dystrophy was seen.
Glomus tumors, first described by Wood in 1812 as “painful subcutaneous tubercles”, are rare benign neoplasms arising from subcutaneous glomus bodies characterized by pain and temperature sensitivity [13]. With their role in thermoregulation, glomus bodies are usually found in the reticular stratum of the dermis throughout the body [3]. Glomus bodies comprise neuromyoarterial components – namely, an afferent arteriole, efferent venule, and an anastomotic Sucquet-Hoyer canal joining the two, which are lined by modified smooth muscle cells from which glomus tumors can arise [2]. They are more prevalent in the subungual regions of the extremities. Glomus tumors are uncommon and represent around 1.5% of all benign soft-tissue neoplasms in the upper and lower extremities [14]. Patients found with glomus tumors usually average between 30 and 50 years of age, with the majority of patients being women [14]. The highest incidence (75%) of glomus tumors arise in the hands, especially in the subungual areas and fingertips, although they can be found in almost any site of the body including rare reports in the subungual regions of the toes and the plantar surface of the heel, arch and forefoot [5, 15]. Glomus tumors also account for an estimated 1-5% of all hand tumors [9]. Furthermore, they can be classified into two clinical presentations, solitary and multiple. Solitary glomus tumor makes up 90% of cases and occurs spontaneously in older individuals, usually women [16]. On the other hand, multiple glomus tumor syndrome is rarer and transmits in an autosomal dominant pattern, presenting more commonly in younger patients. This form occurs more frequently in men and has been reportedly painless in general [17]. This type of tumor is relatively uncommon in the subungual regions of the toes, although there have been several reports of occurrence in the hallux [3, 5-8]. There are even fewer reports in the lesser toes, with Tadashi et al. recently reporting a very unusual presentation of simultaneous glomus tumors in the third and fourth toes [9-12]. Due to its rare presentation, this type of tumor often leads to diagnostic uncertainty, resulting in late detection and resolution of the tumor. Jamari Sapuan et al. described a case of glomus tumor in the second toe in a 56-year-old female with a delayed diagnosis of approximately 18 years as various general practitioners were unaware of this rare presentation of glomus tumor in the toes [11]. The patient, who had experienced pain in her second toe for 15 years, was eventually treated with surgical excision of the tumor and described the disappearance of symptomatic pain as quickly as 3-days post-surgery [11]. Hence, glomus tumors are very treatable and with greater awareness of this rare condition, even when presenting in abnormal sites, can lead to early detection and a timelier resolution of symptoms for patients. Diagnosis of glomus tumors is established clinically through the history and examination features of the patients. Glomus tumors typically present with a classical triad of symptoms – cold hypersensitivity, point tenderness, and severe paroxysmal pain, although not all three are present in every case. Each of the classical triad of symptoms can be demonstrated via three main clinical tests [18]. Love’s test aims to localize the tenderness of the affected area. The head of a pin, toothpick, or any other pinpoint instrument is pressed over the affected region, and eliciting severe pain is indicative of a positive test [19]. Second, Hildreth’s test can also be reliably used to diagnose glomus tumors. The test is executed by elevating the patients’ limb to exsanguinate it, followed by inflating a tourniquet to 250 mm Hg. If the test is positive, there will be reduction in pain and tenderness. The converse will also occur when the cuff is released, causing a sudden onset of pain and tenderness around the tumor [20]. Finally, a cold sensitivity test using an ice cube can be performed to demonstrate increased pain when the digit is exposed to cold [6]. All three tests should be synergized to maximize diagnostic accuracy. Even though glomus tumors can be clinically diagnosed, radiological evidence is indispensable in further isolating the location of the tumor pre-operatively and assessing its size. Simple X-ray testing is an inexpensive and simple test to do, although they have been reported to be helpful in only 22% of cases, with many cases showing no abnormality on X-ray [19]. While plain radiographs may not be able to directly image the tumor, they may show bony erosive changes in the phalanges secondary to the tumor and can be of value. Tumors that are too small to be picked up through plain radiographs can be further imaged via MRI, which might demonstrate masses as a hypointense region on T1-weighted images and with hyperintensity on T2-weighted images [6]. Ultrasound can be a cheaper alternative, although its limitation lies in the difficulty of differentiating glomus tumors from other hypoechoic masses and its underestimation of the size of the tumor [21, 22]. Ultrasound findings should therefore be used in conjunction with clinical findings. In our patient, X-ray and MRI results were initially interpreted as normal, with the glomus tumor only detected upon second opinion, which illustrates that detecting glomus tumors from imaging can be difficult in the unsuspecting clinician. Histology should be used to confirm the diagnosis of glomus tumors, which usually comprise three components: glomus cells, vasculature, and smooth muscle cells. Hyperplasia of any of these three cell types will result in a glomus tumor, giving rise to the three main types of glomus tumors that are solid glomus tumor (75%), glomangioma (20%), and glomangiomyoma (5%) [2]. Finally, there are other variants that are exceedingly rare, including the malignant glomus tumors which make up <1% of all glomus tumor cases [6, 12]. Criteria have been formulated by several authors to Folpe et al. to raise suspicion of the malignant form of glomus tumors: Tumors with a deep location and a size of more than 2 cm, or atypical mitotic figures, or moderate-to-high nuclear grade and five or more mitotic figures per 50 high power field [23]. Complete surgical removal is the treatment of choice for subungual glomus tumors, as it can provide a definitive cure and prevent recurrence in most cases [24]. The recovery period is usually between 2 and 4 weeks; however, it is normal for the pain to take months to subside [21]. Following the surgical approach, the two main complications are recurrence and nail dystrophy. Recurrence rates are still being debated but can occur between 1-50% of cases, usually presenting as a recurrence of pain after weeks and sometimes, even years [21, 25]. An earlier recurrence of pain is likely due to an incomplete removal of the tumor, while a later recurrence is usually indicative of the growth of a second tumor. It has been noted that skin-colored tumors and tumors that grow in the nail matrix precipitate a higher rate of recurrence, as they tend to be harder to delineate during surgery leading to incomplete removal of the tumor [25]. Nail dystrophy also can occur post-surgery, due to the irregularity of the nail bed following surgery and adherence of the eponychium to the nail matrix [26]. This complication tends to occur more often with the transungual method, but different solutions have recently been developed to avoid this complication [21, 26]. Using MRI and ultrasound to more accurately determine the site and extent of the tumor can be helpful in promoting complete excision of the tumor and reducing the iatrogenic induction of nail dystrophy [25]. Several different surgical approaches to accessing subungual glomus tumors have been reported, namely, a transungual and a periungual approach. A general rule of thumb is that the transungual approach is usually applied to glomus tumors that are centrally located in the nail bed, while a periungual approach is utilized when the tumors are situated more peripherally [26]. The transungual approach, which has traditionally been the method used most frequently, involves removing either a small window in the nail table overlying the tumor or by removing the entire nail table to access the tumor [14, 27]. The benefit of this approach is that it enables complete visualization of the underlying nail bed, especially in situations where imaging studies have not been adequate to visualize the lesion [6]. This reduces the chance of incomplete excision of the tumor, which could give rise to recurrence of the tumor. However, the main drawback of this method is that it is associated with high rates of nail dystrophy between 3 and 26% [4, 18], although these findings were not found in several other studies [28,29]. It has been proposed that with careful handling of the nail tissues and meticulous repair of the nail bed after excision, the risk of nail dystrophy can be reduced [30]. Specifically, the incisions made with this technique should be longitudinal and centered over the tumor; the nail bed repaired with inverted interrupted points with absorbable sutures; followed then by restoring the previously resected nail plate to its original position after perforating it to allow for hematoma drainage [24, 31]. A periungual approach is deemed more effective in cases where the tumor is located peripherally, as well as to reduce the risk of nail dystrophy that may lead to a less aesthetic outcome for the patient [12]. This technique involves making a lateral incision that is continued down to the distal phalanx, after which a dorsal flap containing the skin, nail bed, and matrix is elevated to access the tumor. After visualization and excision, the flap is replaced in its original position [31]. Such an approach, however, has lower exposure of the tumor and increases the risk of incomplete tumor resection. Literature has reported that the average recovery period takes between 2 and 4 weeks, although in some cases takes months for the pain to completely subside [5]. In our patient, the transungual approach was employed due to the central location of the tumor, with much success. To reduce nail dystrophy, the nail bed incision was repaired with absorbable sutures and the entire nail was replaced over the nail bed as a protective covering post-excision. The pain subsided within 6 weeks and there was no recurrence or nail dystrophy after 1-year post-operation. From this case study, we hope that we have highlighted the diagnostic difficulty of glomus tumors in the subungual region of the lesser toes. Due to its rare presentation in this location, this diagnosis may not be suspected and can even be challenging to detect on X-ray and MRI imaging. Selection between transungual or periungual approaches should consider the location of the tumor on the nail bed and we recommend exercising caution and frequent monitoring for nail dystrophy.
From this case report, we add to a growing body of case reports showing the rare occurrence of glomus tumors in the foot, and the even rarer presentation in the lesser toes. Following this experience, we have seen that glomus tumors are difficult to diagnose even after thorough radiological investigation. This concurs with other case reports of glomus tumors of their diagnostic difficulty. This is very unfortunate, as glomus tumors are very easily treated and surgical resection can give symptom relief very quickly for patients, with minimal risk. As such, we hope to echo the sentiment of the need for clinicians to raise their suspicion for glomus tumors in cases of toe pain. In turn, this should reduce the long delay to diagnosis and treatment.
Glomus tumors rarely occur in the foot as a cause for toe pain, with very few reports of glomus tumors in the lesser toes. We report a case of glomus tumor in the left second toe distal phalanx that was initially missed on X-ray and MRI radiology. The diagnosis of glomus tumors was only made on second review of the imaging, highlighting the difficulty in identification. This is very unfortunate, considering that glomus tumors are easily treatable and surgical excision provides rapid relief of symptoms for patients. We hope that we have enhanced suspicion for glomus tumors as an important differential for toe pain and emphasized the need for a thorough review of the imaging to not miss this as the diagnosis.
References
- 1.Chou T, Pan SC, Shieh SJ, Lee JW, Chiu HY, Ho CL. Glomus tumor: Twenty-year experience and literature review. Ann Plast Surg 2016;76 Suppl 1:S35-40. [Google Scholar]
- 2.Sethu C, Sethu AU. Glomus tumour. Ann R Coll Surg Engl 2016;98:e1-2. [Google Scholar]
- 3.Lui TH, Mak SM. Glomus tumor of the great toe. J Foot Ankle Surg 2014;53:360-3. [Google Scholar]
- 4.Van Geertruyden J, Lorea P, Goldschmidt D, de Fontaine S, Schuind F, Kinnen L, et al. Glomus tumours of the hand. A retrospective study of 51 cases. J Hand Surg Br 1996;21:257-60. [Google Scholar]
- 5.Pater TJ, Marks RM. Glomus tumor of the hallux: Case presentation and review of the literature. Foot Ankle Int 2004;25:434-7. [Google Scholar]
- 6.Polo C, Borda D, Poggio D, Asunción J, Peidro L. Glomus tumor of the hallux. Review of the literature and report of two cases. Foot Ankle Surg 2012;18:89-93. [Google Scholar]
- 7.Seo JH, Lee HS, Kim SW, Jeong JJ, Choi YR. Subungual glomus cell proliferation in the toe: A case report. J Foot Ankle Surg 2014;53:628-30. [Google Scholar]
- 8.Trehan SK, Soukup DS, Mintz DN, Perino G, Ellis SJ. Glomus tumors in the foot: Case series. Foot Ankle Spec 2015;8:460-5. [Google Scholar]
- 9.Hwang J, McDowell S, Cole B, Huber A, Reyes MC. Cytologic analysis of a glomus tumor in the left second toe: Case report. Diagn Cytopathol 2022;50:E170-3. [Google Scholar]
- 10.Kimura T, Kubota M, Hattori H, Saito M. Simultaneous glomus tumors of the third and fourth toes: A case report. JBJS Case Connect 2022;12:e21.00780. [Google Scholar]
- 11.Sapuan J, Paul AG, Abdullah A. Glomus tumor in the second toe: A clinical insight. J Foot Ankle Surg 2008;47:483-6. [Google Scholar]
- 12.Romanos E, Al Delfi F, Hubballah M, Farah C. Glomus tumour of the fourth toe: Case discussion and review of literature. BMJ Case Rep 2019;12:e231100. [Google Scholar]
- 13.Wood W. On painful subcutaneous tubercle. Edinburgh Med Surg J 1812;8:283-91. [Google Scholar]
- 14.Carroll RE, Berman AT. Glomus tumors of the hand: Review of the literature and report on twenty-eight cases. J Bone Joint Surg Am 1972;54:691-703. [Google Scholar]
- 15.Rettig AC, Strickland JW. Glomus tumor of the digits. J Hand Surg 1977;2:261-5. [Google Scholar]
- 16.Dwidmuthe S, Nemade A, Rai S. Glomus tumor of thumb occurring at unusual location. J Surg Tech Case Rep 2013;5:92-4. [Google Scholar]
- 17.Beasley SW, Mel J, Chow CW, Jones PG. Hereditary multiple glomus tumours. Arch Dis Child 1986;61:801-2. [Google Scholar]
- 18.Vasisht B, Watson HK, Joseph E, Lionelli GT. Digital glomus tumors: A 29-year experience with a lateral subperiosteal approach. Plast Reconstr Surg 2004;114:1486-9. [Google Scholar]
- 19.Bhaskaranand K, Navadgi BC. Glomus tumour of the hand. J Hand Surg Br 2002;27:229-31. [Google Scholar]
- 20.Giele H. Hildreth’s test is a reliable clinical sign for the diagnosis of glomus tumours. J Hand Surg Br 2002;27:157-8. [Google Scholar]
- 21.Chen SH, Chen YL, Cheng MH, Yeow KM, Chen HC, Wei FC. The use of ultrasonography in preoperative localization of digital glomus tumors. Plast Reconstr Surg 2003;112:115-9. [Google Scholar]
- 22.Tomak Y, Akcay I, Dabak N, Eroglu L. Subungual glomus tumours of the hand: Diagnosis and treatment of 14 cases. Scand J Plast Reconstructive Surg Hand Surg 2003;37:121-4. [Google Scholar]
- 23.Folpe AL, Fanburg-Smith JC, Miettinen M, Weiss SW. Atypical and malignant glomus tumors: Analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol 2001;25:1-12. [Google Scholar]
- 24.Lin YC, Hsiao PF, Wu YH, Sun FJ, Scher RK. Recurrent digital glomus tumor: Analysis of 75 cases. Dermatol Surg 2010;36:1396-400. [Google Scholar]
- 25.Tada H, Hirayma T, Takemitsu Y. Prevention of postoperative nail deformity after subungual glomus resection. J Hand Surg 1994;19:500-3. [Google Scholar]
- 26.Takata H, Ikuta Y, Ishida O, Kimori K. Treatment of subungual glomus tumour. Hand Surg 2001;6:25-7. [Google Scholar]
- 27.Samaniego E, Crespo A, Sanz A. Key diagnostic features and treatment of subungual glomus tumor. Actas Dermosifiliogr 2009;100:875-82. [Google Scholar]
- 28.Jawalkar H, Maryada VR, Brahmajoshyula V, Kotha GK. Subungual glomus tumors of the hand: Treated by transungual excision. Indian J Orthop 2015;49:403-7. [Google Scholar]
- 29.Lee IJ, Park DH, Park MC, Pae NS. Subungual glomus tumours of the hand: Diagnosis and outcome of the transungual approach. J Hand Surg Eur Vol 2009;34:685-8. [Google Scholar]
- 30.Grover C, Khurana A, Jain R, Rathi V. Transungual surgical excision of subungual glomus tumour. J Cutan Aesthet Surg 2013;6:196-203. [Google Scholar]
- 31.Madhar M, Bouslous J, Saidi H, Fikry T, Schuind F. Which approach is best for subungual glomus tumors? Transungual with microsurgical dissection of the nail bed or periungual? Chir Main 2015;34:39-43. [Google Scholar]