The management of spondylodiscitis in patients with chronic kidney disease warrants the importance of interdisciplinary collaboration and early diagnosis before irreversible neurological damage can take place.
Dr. Jenil Patel, Department of Orthopaedics, Bombay Hospital and Medical Research Institute, A/25, Sardar Smriti Bldg., S V Road, Near Chamunda Circle, Borivali West, Mumbai 400092, Maharashtra, India. E-mail: jenilpatel.jp23@gmail.com
Introduction: Infective spondylodiscitis, resulting from bacterial or fungal infections in intervertebral discs and adjacent vertebral bodies, poses diagnostic dilemmas due to its rare occurrence and subtle symptomatology. This report underscores the importance of a multidisciplinary approach in navigating the complexities of infective spondylodiscitis, particularly in patients with concomitant chronic kidney disease (CKD).
Case Report: A 53-year-old male, 5 years into renal dialysis for CKD, presented with a 3-month history of severe neck pain radiating to both arms, accompanied by tingling sensations. Neurological evaluation revealed weakness and gait imbalance. Laboratory findings indicated elevated serum creatinine, erythrocyte sedimentation rate, and C-reactive protein. Imaging confirmed vertebral destruction, necessitating a staged treatment plan involving surgical intervention, corpectomy, mesh placement, and fusion. Intraoperative cultures yielded negative results, prompting continued broad-spectrum antibiotic therapy intravenously for 2 weeks, followed by an additional 4 weeks orally.
Discussion: The case discussion explores common risk factors for infective spondylodiscitis, emphasizing the need for a comprehensive diagnostic approach in patients with immunocompromised conditions, such as CKD. Despite negative cultures, the patient's favorable clinical response and neurological recovery underscore the intricate nature of infectious processes, especially in individuals with underlying health concerns.
Conclusion: This case report serves as a poignant reminder of the challenges associated with infective spondylodiscitis in CKD patients on hemodialysis. The classic triad of pain, fever, and neurological deficits should trigger a thorough diagnostic investigation, leveraging advanced imaging techniques for accurate diagnosis. A multidisciplinary approach and regular follow-ups are essential in managing such complex cases, contributing to improved patient outcomes and overall healthcare quality.
Keywords: Infective spondylodiscitis, chronic kidney disease, unknown origin, hemodialysis, corpectomy, anterior cervical discectomy with fusion, fusion.
Infective spondylodiscitis is a challenging condition that results from bacterial or fungal infection of the intervertebral disk and adjacent vertebral bodies [1]. The usual manifestation includes pain, elevated body temperature, and neurological symptoms. Due to the disease’s infrequency and insidious manifestation of symptoms, the identification of the condition may become delayed. Hence, significant concerns such as the occurrence of an abscess in adjacent tissue, irreversible permanent neurological abnormalities, or even mortality may arise before the identification of a diagnosis. Although there have been advancements in prolonging the lives of patients undergoing hemodialysis for end-stage renal disease, the mortality rate for those who develop bacteremia or sepsis due to repeated vascular access, medically induced immunosuppression, and urinary tract infections remains elevated at 9.7% [2, 3]. This report describes the case of a 53-year-old male with infective spondylodiscitis complicated by chronic kidney disease (CKD), highlighting the importance of a multidisciplinary approach in managing such complex cases.
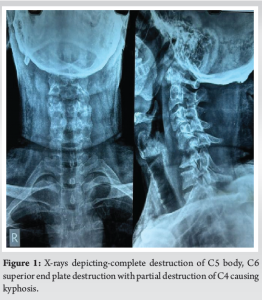
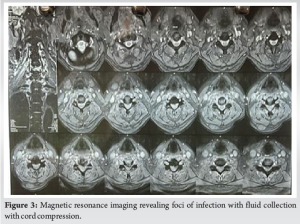
A 53-year-old male presented to the outpatient department of our institution with complaints of significant neck pain affecting his daily activities for the past 3 months. Pain has since been radiating to both arms (left > right), which was associated with a tingling sensation. On evaluating the neurology, the Medical Research Council grade of both upper limbs was found to be 4/5 with finger grip weakness observed as more pronounced on the left side. The patient also had increasing gait imbalance while walking contributing to significant problems at the workplace. There was no history of falls, trauma, or any significant strain on the cervical spine. On analysis of history, revealed to be a known case of CKD and was on renal dialysis, for the past 5 years. The patient’s blood reports had an evident finding of raised serum creatinine (7.1) and borderline elevated serum erythrocyte sedimentation rate and C-reactive protein. Other blood parameters were within normal limits. Pre-operative x-ray showed reduced disk space in C5-C6 with partial destruction of C4 and C5 vertebral body following collapse of the vertebrae (Fig. 1). MRI revealed foci of infection in C5-C6 disc space with fluid collection with cord compression.
Treatment
The patient has planned a staged treatment protocol, in which the first was surgical intervention followed by intravenous antibiotics treatment. After medical optimization was completed and fitness was received a standard Southwick-Robinson approach was taken following which meticulous dissection was carried out. After exposure, C4-C5 and C5-C6 junction was identified and confirmed under fluoroscopy. Suspected infective tissue along with disc and bone samples was collected in a sterile container for investigation. After thorough debridement and washing end plates were prepared, and dead necrotic tissue was removed followed by a C5 corpectomy. Mesh cage was placed with anterior cervical discectomy with fusion at C6-C7 vertebral bodies supplemented with anterior plate were fixed from C4 to C7 vertebra. A thorough wash was given and closure was done in layers. Post-operative, we administered the intravenous broad-spectrum antibiotic Cefoperazone-Sulbalctam intravenous for 2 weeks. He underwent heparin-free dialysis post-surgery and was hemodynamically stable after which he was discharged. The peculiar characteristic in this case was the intraoperative culture reports were negative for Mycobacterium tuberculosis or any other bacteria. Hence, the continuation of the broad spectrum was given IV for 2 weeks and then followed up by oral antibiotics for duration of 4 weeks (Fig. 2, 3, 4).

According to a study of the literature, intravenous drug use, poorly managed or uncontrolled diabetes mellitus, catheter-associated infection problems, infective endocarditis, history of spine surgery, and immunocompromised condition are common risk factors for infective spondylodiscitis [4]. Prior research on dialysis patients and the general public on infectious spondylodiscitis revealed that the majority of infections occurred in the lumbar spine (58–68%), thoracic spine (27–30%), and cervical spine (5–81%) [5]. According to previous research on spinal osteomyelitis, 85% of the organisms found in blood cultures were also found in biopsy specimens. Consequently, it can be recommended that, wherever possible, all patients with suspected infective spondylodiscitis have their blood and tissue cultures taken. In this case, the samples that were sent were negative for any kind of bacterial or fungal infection. M. tuberculosis was not isolated from the specimen of an isolated disc or vertebral bone [6]. The patient was followed up regularly in the outpatient department after 2 weeks, 1 month, and 2 months. Upon neurological assessment, his finger grip had improved which was found to be 5/5. In people with end-stage renal disease (ESRD), a number of risk factors contribute to the illness’s development and antibiotic failure. Difficult-to-diagnose conditions include imprecise initial symptoms, concurrent destructive spondyloarthropathy, weakened immune system, persistently elevated inflammatory markers, and recurrent bacteremia. Permanent brain abnormalities are more likely to result from infectious processes than from temporary ones [7, 8]. Even in situations of severe destructive osteomyelitis, fever may not be the first symptom to appear, and it occasionally manifests as a latent infection. Therefore, even in patients who do not have a fever when they present with ESRD, a spinal infection should be considered as a potential cause of back pain, and an MRI should be done to make an early diagnosis. In all cases of spondylodiscitis, surgical intervention with debridement and posterior instrumentation should be taken into consideration as a modality of treatment. This approach has better clinical outcomes in terms of functionality, disability, and rehabilitation, as well as acceptable perioperative complication rates that can be tailored to the specifics of each case [9]. Despite the instrumented group having a greater degree of neurological deficit, more involved levels, and an increased kyphotic angle, the results of instrumented surgery for hemodialyzed patients with pyogenic spondylodiscitis were comparable to those of non-instrumented surgery, including recurrence and mortality [10].
This case study is a testament that patients who receive long-term hemodialysis or are in hospital-based environments for longer periods, it is crucial to identify spondylodiscitis in such patients. Classical features should be looked for: the classic triad of pain, fever, and neurological deficits. Optimal use of enhanced MR scans in patients presenting with significant neck pain can help establish the diagnosis, which can then guide the best course of treatment.
This case report emphasizes the critical need for a multidisciplinary approach in diagnosing and managing infective spondylodiscitis, especially in patients with chronic kidney disease (CKD) on hemodialysis. The classic triad of pain, fever, and neurological deficits should prompt thorough diagnostic investigations, including advanced imaging techniques. Early detection and treatment are paramount to prevent irreversible neurological damage. Despite the diagnostic challenge posed by negative culture results, continued broad-spectrum antibiotic therapy and surgical intervention can lead to favorable clinical outcomes. Regular follow-ups and coordinated care among specialties are essential in improving patient prognosis and overall healthcare quality.
References
- 1.Lu YA, Hsu HH, Kao HK, Lee CH, Lee SY, Chen GH, et al. Infective spondylodiscitis in patients on maintenance hemodialysis: A case series. Ren Fail 2017;39:179-86. [Google Scholar]
- 2.Cassó-Troche LR, Echavarría-Uceta JA, Quiñones-Robles J, Haché-Pagan C, Herrera I, Encarnación J, et al. Infective spondylodiscitis in hemodialysis patients. Surg Neurol Int 2022;13:549. [Google Scholar]
- 3.Chen LH, Fu TS, Kao YH, Tsai TT, Lai PL, Niu CC, et al. Surgical treatment of infectious spondylitis in patients undergoing hemodialysis therapy. Eur Spine J 2010;19:2223-8. [Google Scholar]
- 4.Kapsalaki E, Gatselis N, Stefos A, Makaritsis K, Vassiou A, Fezoulidis I, et al. Spontaneous spondylodiscitis: Presentation, risk factors, diagnosis, management, and outcome. Int J Infect Dis 2009;13:564-9. [Google Scholar]
- 5.Saran R, Li Y, Robinson B, Abbott KC, Agodoa LY, Ayanian J, et al. US renal data system 2015 annual data report: Epidemiology of kidney disease in the United States. Am J Kidney Dis 2016;67 3 Suppl 1:S7, S1-305. [Google Scholar]
- 6.Afshar M, Reilly RF. Spondylodiscitis in a patient on chronic hemodialysis. Nat Rev Nephrol 2011;7:599-604. [Google Scholar]
- 7.Faria B, Canto Moreira N, Sousa TC, Pêgo C, Vidinha J, Garrido J, et al. Spondylodiscitis in hemodialysis patients: A case series. Clin Nephrol 2011;76:380-7. [Google Scholar]
- 8.Madhavan K, Chieng LO, Armstrong VL, Wang MY. Spondylodiscitis in end-stage renal disease: A systematic review. J Neurosurg Spine 2019;30:674-82. [Google Scholar]
- 9.Vinay Jain K, Ravikumar TV. Surgical management of thoracolumbar spondylodiscitis in end-stage renal disease. Indian J Orthop 2020;55 Suppl 1:176-81. [Google Scholar]
- 10.Kim J, Lee SY, Jung JH, Kim SW, Oh JK, Park MS, et al. The outcome following spinal instrumentation in haemodialyzed patients with pyogenic spondylodiscitis. Bone Joint J 2019;101-B:75-82. [Google Scholar]