The management of fractures in the osteoporotic distal femur fractures presents a significant challenge due to the compromised bone quality inherent in osteoporosis. Employing dual implant stabilization approach, combining an intramedullary nail and an anatomically contoured plate, represents a strategic intervention aimed at enhancing stability and support throughout the healing process.
Dr. Ravi Modi, Department of Orthopaedics, Dr. DY Patil Medical College and Hospital, Mumbai, Maharashtra, India. E-mail: modiravi1997@yahoo.co.in
Introduction: Securing stable internal fixation for fractures in the osteoporotic intra-articular distal femur proves to be a demanding task due to thin cortices, a wide medullary canal, diminished bone stock, and fracture comminution. No singular therapeutic approach has successfully tackled all facets of this injury. Consequently, we now introduce a pioneering fixation method in our report, aiming to offer a holistic solution to the intricate challenges associated with this scenario.
Case Report: A 60-year-old female presented with an intra-articular distal femur fracture, and underwent a combination fixation of distal femur plate and intramedullary interlocking nailing. The patient was rehabilitated with active knee range of motion on post-operative day 7 and has now attained full knee range of motion.
Conclusion: The utilization of anatomical plates with locking mechanisms, in tandem with intramedullary interlocking nailing, holds promise for the secure stabilization and fixation of osteoporotic distal femur fractures, potentially leading to an expedited recovery process.
Keywords: Distal femur fracture, intra-articular fracture, distal femur plating, intramedullary nailing.
Distal femoral fractures account for 3–6% of all femur fractures. Clinically, these fractures are characterized by occurrences within 15 cm from the distal femoral articular surface. The unstable fracture pattern and frequent comminution of these fractures make treatment extremely challenging [1]. Historically, the majority of distal femur fractures were managed without surgery until around 1970 [2,3]. However, the drawbacks associated with prolonged bed rest, the risk of knee motion loss, incongruities in the knee joint, and the potential for angular deformities prompted further exploration into more effective treatment strategies. In the past 50 years, substantial progress in surgical techniques and implant technology has transformed the landscape, making internal fixation the primary approach for treating distal femur fractures[4]. Despite these advancements, achieving stable internal fixation remains a persistent challenge due to factors such as thin cortices, a wide medullary canal, poor bone stock, and fracture comminution [5]. It is noteworthy that no single therapeutic approach has emerged as a comprehensive solution capable of addressing all aspects associated with this complex injury [6,7]. Hence, we now report this case and the fixation method we used to treat this intra-articular osteoporotic distal femur fracture [4].
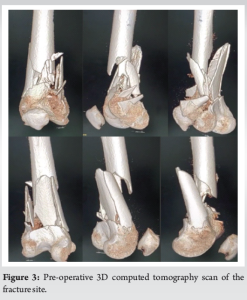
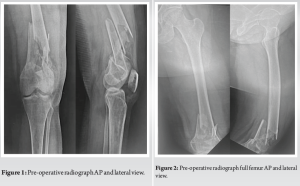
A 60-year-old female patient presented to our emergency ward with pain and swelling in the left knee following a road traffic accident. On physical examination, she was noted to have the knee joint in flexion with severe tenderness and distal pulses were palpable. Radiographs revealed a left-sided intra-articular distal femur fracture (Fig. 1 and 2). The fracture site was promptly immobilized in a long knee brace. Subsequent assessment via a computed tomography scan showed severe comminution at the fracture site (Fig. 3). After careful consideration the patient was scheduled for surgery.
The patient was positioned supine on the operating table under spinal and epidural anesthesia. A roughly 24 cm long incision was made on the anterolateral aspect of the patella, extending up to the proximal femur, following the swashbuckler approach. The fracture site at the intercondylar level was meticulously reduced and secured in place using K-wires. Subsequently, 4 mm cannulated cancellous screws were inserted across the fracture site, and retrograde intramedullary nailing was performed. Distal locking of the nail was achieved under fluoroscopy. Following this, a distal femoral plate was positioned on the lateral surface of the femur. The largest proximal and distal fracture segments were carefully realigned and held in position with bone clamps. The plate was securely fixed to the distal surface and shaft using bicortical purchase while locking screws were employed in the proximal shaft unicortically. The construct was determined to be adequately stabilized. To address the distal comminutions, an allograft made of calcium phosphate (Allogra R bone graft) was inserted. As a precautionary measure, an above knee slab was applied, maintaining a 20° flexion angle after doing immediate post-operative X-rays (Fig. 4 and 5).
The slab was maintained for 3 days after which it was replaced with a long knee brace for the next 4 weeks. Active knee range of motion exercises was initiated on post-operative day 7. Remarkably, by the conclusion of the 4-week period, the patient had achieved 90° of flexion. At the 6-week mark, partial weight-bearing walking with the assistance of a walker was introduced. By the end of 6 months, the patient had regained full range of motion (Fig. 6) and resumed her pre-injury routine without any significant complaints. 6 months follow-up X-rays showed significant bone union (Fig. 7 and 8).


In recent times, there has been a growing trend ‘towards’ utilizing in double construct fixation for distal femoral fractures, especially in cases involving more intricate fractures. This approach, involving both nail and plate fixation, is suggested to provide patients with a more resilient construct capable of supporting early weight bearing [8]. In scenarios marked by severe articular and metaphyseal comminution, osteoporotic bone, medial cortical defect, and very low distal femur fractures, depending on a solitary lateral plate proves insufficient, lacking the necessary support to resist strain. This deficiency in fixation stability, coupled with the risk of early implant failure, non-union, and the potential for varus or valgus collapse, arises from incapacity to counteract the bending tendency induced by the vertical load. Despite incorporating fixed angles, locking systems, enhanced screw purchase in the distal fragment, and cutting-edge biological fixation-powered locking plates, the presence of a medial cortical defect and extensive comminution, particularly in osteoporotic bones with a low fracture line, poses a formidable challenge by concentrating stress predominantly on the lateral side. A multitude of biomechanical studies conducted over time consistently highlight the insufficiency of relying solely on lateral locking plate fixation. Concerns regarding non-union and the potential for metalwork failure have recently gained attention in the context of standalone lateral plate fixation for distal femoral fractures. An alternative approach for addressing these fractures involves the usage of a retrograde intramedullary nail. Historically, plates have been employed to manage fractures when there is inadequate distal bone stock for nail attachment, despite the fact that retrograde intramedullary nail constructs do not exhibit a significant biomechanical advantage over lateral plate constructs. Furthermore, it is important to note that not all distal femoral fractures treated with nailing are authorized for full weight-bearing [9, 10]. The biomechanical attributes of retrograde intramedullary nailing and lateral plates are synergistically combined in nail plate constructions to create a more sturdy fixation. In this construct, the entire load is borne by the plate, making it the primary load-bearing structure. Conversely, the nail serves as a load sharing mechanism, distributing forces through contact between the nail and the cortex, as well as the surrounding cortex. Notably, in a biomechanical study utilizing a synthetic model of distal femur fracture, the nail plate construct demonstrated superior performance in terms of axial strength and torsional stability compared to solitary nails or plates [11, 12]. To enhance the overall stability of the system, Liporace and Yoon recommended connecting the plate and the nail distally. This connection is established using fluoroscopy and the “perfect circle” approach. In instances of severe osteoporosis, these authors advocate for the use of two interconnected screws and typically spanning the entire femur with plate [13].
Much like fractures in the proximal femur, prompt surgical intervention is crucial for osteoporotic distal femoral fractures, aiming for a secure repair that allows early weight-bearing. Treatment options include distal femur replacement, lateral plate, retrograde intramedullary nail, or a combination of implants such as nail plate. Nail plate constructs, merge the load-sharing features of nailing with the load-bearing characteristics of plating, expediting weight bearing and diminishing the risk of non-union and hardware failure. Employing a dual implant fixation approach may particularly benefit obese, osteoporotic, or elderly patients, minimizing non-union risk and facilitating swift mobilization. Factors contributing to non-union risk encompass periprosthetic fractures, fractures with medial comminution, and metaphyseal engagement [14]. While larger randomized controlled trials may eventually establish the superiority of nail and plate fixation, additional research is necessary for definitive conclusions.
Treating fractures in treating osteoporotic distal femur is a challenge due to its weakened bone quality. Combining an intramedullary nail with an anatomically contoured plate offers a strategic solution to enhance stability and support during healing, with the added advantage of earlier mobilization.
References
- 1.Coon MS, Best BJ. Distal femur fractures. In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. [Google Scholar]
- 2.Martinet O, Cordey J, Harder Y, Maier A, Bühler M, Barraud GE. The epidemiology of fractures of the distal femur. Injury 2000;31 (Suppl 3):C62-3. [Google Scholar]
- 3.Elsoe R, Ceccotti AA, Larsen P. Population-based epidemiology and incidence of distal femur fractures. Int Orthop 2018;42:191-6. [Google Scholar]
- 4.Ehlinger M, Ducrot G, Adam P, Bonnomet F. Distal femur fractures. Surgical techniques and a review of the literature. Orthop Traumatol Surg Res 2013;99:353-60. [Google Scholar]
- 5.Higgins TF, Pittman G, Hines J, Bachus KN. Biomechanical analysis of distal femur fracture fixation: Fixed-angle screw-plate construct versus condylar blade plate. J Orthop Trauma 2007;21:43-6. [Google Scholar]
- 6.Kontakis MG, Giannoudis PV. Nail plate combination in fractures of the distal femur in the elderly: A new paradigm for optimum fixation and early mobilization? Injury 2023;54:288-91. [Google Scholar]
- 7.Sanders R, Swiontkowski M, Rosen H, Helfet D. Double-plating of comminuted, unstable fractures of the distal part of the femur. J Bone Jt Surg Am 1991;73:341-6. [Google Scholar]
- 8.Sain A, Sharma V, Farooque K, Muthukumaran V, Pattabiraman K. Dual plating of the distal femur: Indications and surgical techniques. Cureus 2019;11:e6483. [Google Scholar]
- 9.Button G, Wolinsky P, Hak D. Failure of less invasive stabilization system plates in the distal femur. J Orthop Trauma 2004;18:565-70. [Google Scholar]
- 10.Bliemel C, Buecking B, Mueller T, Wack C, Koutras C, Beck T, et al. Distal femoral fractures in the elderly: Biomechanical analysis of a polyaxial angle-stable locking plate versus a retrograde intramedullary nail in a human cadaveric bone model. Arch Orthop Trauma Surg 2014;135:49-58. [Google Scholar]
- 11.Zhao Z, Li Y, Ullah K, Sapkota B, Bi H, Wang Y. The antegrade angle-stable locking intramedullary nail for type-C distal femoral fractures: A thirty four case experience. Int Orthop 2018;42:659-65. [Google Scholar]
- 12.Başci O, Karakaşli A, Kumtepe E, Güran O, Havitçioğlu H. Combination of anatomical locking plate and retrograde intramedullary nail in distal femoral fractures: Comparison of mechanical stability. Eklem Hastalik Cerrahisi 2015;26:21-6. [Google Scholar]
- 13.Liporace FA, Yoon RS. Nail plate combination technique for native and periprosthetic distal femur fractures. J Orthop Trauma 2019;33:E64-8. [Google Scholar]
- 14.Fontenot PB, Diaz M, Stoops K, Barrick B, Santoni B, Mir H. Supplementation of lateral locked plating for distal femur fractures: A biomechanical study. J Orthop Trauma 2019;33:642-8. [Google Scholar]