Consider periodical radiographic surveillance of ballistic fragments to document movement.
Dr. Olumide Danisa, Department of Orthopaedic Surgery, Loma Linda University Medical Center, Loma Linda, California, USA. E-mail: odanisa@yahoo.com
Introduction: Literature showcases conflicting findings regarding the outcomes of ballistic fragment removal from the spine in gunshot wounds (GSW) patients. Further research in this area is needed to better comprehend the nuances of risks and benefits surrounding ballistic fragment removal from the spine in GSW patients. In this case report, we discuss the late-onset cervical prevertebral abscess which developed when a previously embedded bullet fragment migrated into the retropharyngeal space 11 years after an initial GSW.
Case Report: A 29-year-old male sustained a gunshot wound to the face in 2011. He was stabilized with a posterior C3-C6 lateral mass instrumentation and fusion. There were no attempts to remove the bullet fragments. In 2023, the patient returned with worsening neck pain. Imaging demonstrated a retropharyngeal abscess with interval rotation of the ballistic fragment by 90°. An abscess was noted anterior to the cervical vertebrae with a freely mobile ballistic fragment within.
Conclusion: This case highlights several questions: What is the criteria for radiographic surveillance of retained hardware? If there is documented movement, should this trigger further investigation? What complications can occur that warrant careful removal?
Keywords: Gunshot wound, ballistic, fragment, cervical, spine.
Approximately 120,000 gunshot wounds (GSWs) occur in the US annually [1]. Moreso, GSWs account for 13–17% of all spinal cord injuries each year [2-10]. Management of ballistic trauma requires careful consideration of multiple factors including injury location. At present, indications for surgery and potential removal of bullet fragments include: Intra-articular metallic fragments with concerns for plumbism, neural compression by fragments of bone or bullet in the spine, or if there is risk of bacterial contamination if the bullet traverses the bowel. Injury severity also plays a major role where high-energy GSWs create an extensive zone of injury with devitalized tissue which ultimately needs debridement. Considerations for surgical removal also include associated injuries and potential long-term consequences of treatment [11-13]. For retained ballistic fragments that do not meet these criteria, the decision to remove the fragment is often based on the surgeon’s experience and discussion with the patient. Several reports have investigated the outcomes of ballistic fragment removal from the spine in GSW patients. Moisi et al. found that removing ballistic fragments was necessary to avoid migration of foreign bodies and further degeneration of neurologic function [14]. Contrastingly, Benton et al. suggest that fragment removal does not significantly improve patient outcomes and may increase the risk of complications due to the surgical procedure [15]. These conflicting findings highlight the need for further research in this area to better comprehend the nuances of risks and benefits surrounding ballistic fragment removal from the spine in GSW patients. In this case report, we discuss the late-onset cervical prevertebral abscess which developed when a previously embedded bullet fragment migrated into the retropharyngeal space 11 years after an initial GSW.
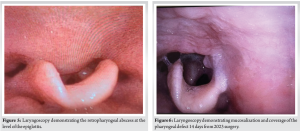
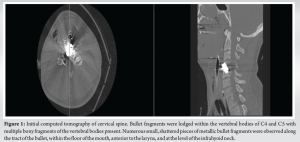
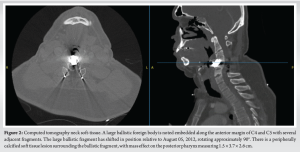
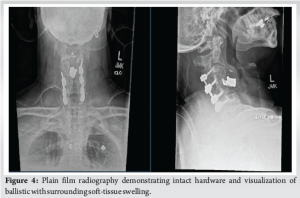
A 29-year-old male sustained a low-velocity GSW to the face (mandible and neck) in August 2011. He was shot from the front with an anterior entry site resulting in bodily injury to the mandible, injury and deformation to the anterior cervical spine at C4 and C5, and most importantly, developing a spinal cord injury. He was left an incomplete C6 tetraplegic. At the time of index injury, he was stabilized by the neurosurgery service with a posterior C3-C6 lateral mass instrumentation and fusion. The documented rationale for this approach was because of the anterior entrance wound, local trauma, and the presence of a tracheostomy which was performed in the acute setting. There were no attempts to remove the bullet fragments; the patient did not develop worsening dysphagia or worsening pain and did not demonstrate signs of plumbism. For the next decade, the patient did well and no further radiographs were obtained after 2012. In February 2023, the same patient presented to the Emergency Department after a 3-day history of worsening neck pain with a 1-day history of fever and a reported max temperature of 106℉ at home. The patient presented with leukocytosis and a white blood cell count of 13.96K. Soft-tissue computed tomography (CT) demonstrated a retropharyngeal abscess with interval rotation of the ballistic fragment by 90°, causing mass effect on the airway at C3–5. An esophagram was ordered to rule out esophageal erosion; however, the study did not show a leak or extravasation of contrast into the mediastinum. Surgery was performed in concert with otolaryngology (ENT) because of the patient’s large neck, previous tracheostomy, and concerns for potential esophageal complications. Before surgery, a laryngoscopy was performed by ENT. A traditional left-sided neck exposure performed by ENT did not reveal abnormality in the surgical planes: Deep cervical fascia, peritracheal fascia, and prevertebral fascia were identified. On retraction of the longus colli, a thick ovoid-shaped sac was noted anterior to the cervical vertebrae. The presumed abscess was fluid-filled with a freely mobile ballistic fragment within. More importantly, the abscess wall was intimate with the esophagus. The abscess was pierced and approximately 75–100 mL of thick, yellowish, purulent fluid was expressed and cultured. Pathogen on debridement was Cutibacterium acnes, which is normal oral flora and slow growing. The patient was previously treated by infectious disease: Initially with IV Unasyn for 10 days and then transitioned to oral Augmentin (amoxicillin/clavulanate) 875 mg twice daily for 6 months. A jagged bullet fragment was also recovered. The underlying anterior vertebral bone appeared normal. Excision of the abscess was then performed. A 5-cm defect in the pharynx was subsequently visualized as the retropharyngeal abscess wall comprising the posterior pharyngeal mucosa. The wound was copiously irrigated and the ENT team placed a nasogastric tube through the upper and lower limbs of the esophageal defect then primarily repaired the pharyngeal defect where it was feasible. A left sternocleidomastoid rotational flap was created and used to augment the pharyngeal repair. The patient was made NPO for 6 weeks, and a gastric tube was placed for tube feeds. At 6 weeks, an esophagram demonstrated no leak, and the patient was followed up for 1 year after surgery. The patient was informed that data concerning the case would be submitted for publication, the patient agreed, and institutional review board approval was obtained (#5230573). Fig. 1 demonstrates the patient’s CT of the cervical spine at the time of the initial GSW in 2011. Fig. 2 demonstrates the patient’s CT neck soft-tissue in 2023. Fig. 3 and 4 demonstrate the performed esophagram and plain film radiography, respectively. Fig. 5 and 6 demonstrate the patient’s laryngoscopy findings.
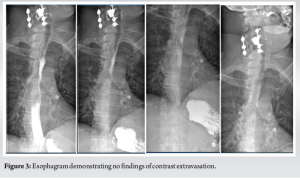
This case demonstrates the migration of a previously embedded bullet fragment. The initial treatment of stabilization distinct from the zone of injury falls within accepted criteria. However, there was not adequate radiographic follow-up to document bullet location and its subsequent migration, which resulted in the need for surgical intervention over a decade later. In addition to surgery, the patient was treated with IV Unasyn for 10 days and then transitioned to oral augmentin (amoxicillin/clavulanate) 875 mg twice daily for 6 months. The patient was made NPO for 6 weeks and a gastric tube was placed for tube feeds. At a 6-week follow-up, an esophagram demonstrated no leak. Literature suggests that the surgical removal of bullet fragments is beneficial in long-term patient outcomes [11,14]. However, other studies have established differing findings, such as how bullet fragment removal does not significantly improve patient outcomes and may increase the risk of complications due to surgery [15]. This case therefore highlights several important questions. The first, what are the criteria for radiographic surveillance of retained hardware? Should radiographs be performed annually or biannually? If there is documented movement, should this trigger further investigation?
Literature showcases conflicting findings regarding the outcomes of ballistic fragment removal from the spine in GSW patients. This case demonstrates the migration of a previously embedded bullet fragment into the retropharyngeal space, leading to a late-onset cervical prevertebral abscess. Radiographic surveillance of retained hardware may detect such rare occurrences and may improve outcomes.
Treatment for ballistic trauma requires careful consideration of multiple factors, and the removal of any fragments is often based on the surgeon’s experience and discussion with the patient. In the case of retained hardware, radiographic surveillance and further investigation may reduce the possibility of adverse fragment migration and improve patient outcomes.
References
- 1.Kaufman EJ, Wiebe DJ, Xiong RA, Morrison CN, Seamon MJ, Delgado MK. Epidemiologic trends in fatal and nonfatal firearm injuries in the US, 2009-2017. JAMA Intern Med 2021;181:237-44. [Google Scholar]
- 2.Sidhu GS, Ghag A, Prokuski V, Vaccaro AR, Radcliff KE. Civilian gunshot injuries of the spinal cord: A systematic review of the current literature. Clin Orthop 2013;471:3945-55. [Google Scholar]
- 3.Bono CM, Heary RF. Gunshot wounds to the spine. Spine J 2004;4:230-40. [Google Scholar]
- 4.Aarabi B, Alibaii E, Taghipur M, Kamgarpur A. Comparative study of functional recovery for surgically explored and conservatively managed spinal cord missile injuries. Neurosurgery 1996;39:1133-40. [Google Scholar]
- 5.Chittiboina P, Banerjee AD, Zhang S, Caldito G, Nanda A, Willis BK. How bullet trajectory affects outcomes of civilian gunshot injury to the spine. J Clin Neurosci 2011;18:1630-3. [Google Scholar]
- 6.Farmer JC, Vaccaro AR, Balderston RA, Albert TJ, Cotler J. The changing nature of admissions to a spinal cord injury center: Violence on the rise. J Spinal Disord 1998;11:400-3. [Google Scholar]
- 7.Gentleman D, Harrington M. Penetrating injury of the spinal cord. Injury 1984;16:7-8. [Google Scholar]
- 8.Lin SS, Vaccaro AR, Reisch S, Devine M, Cotler JM. Low-velocity gunshot wounds to the spine with an associated transperitoneal injury. J Spinal Disord 1995;8:136-44. [Google Scholar]
- 9.Robertson DP, Simpson RK. Penetrating injuries restricted to the cauda equina: A retrospective review. Neurosurgery 1992;31:265-9, discussion 269-70. [Google Scholar]
- 10.Roye WP Jr., Dunn EL, Moody JA. Cervical spinal cord injury--a public catastrophe. J Trauma 1988;28:1260-4. [Google Scholar]
- 11.Kennedy JM, Routsolias JC, Mycyk MB. Succimer mitigates the perioperative risk for an increase in blood lead levels during bulletectomy: A case report. JBJS Case Connect 2023;13:(2). doi: 10.2106/JBJS.CC.23.00011. [Google Scholar]
- 12.Hanson TM, Nierenberg DW, LaRoche HB, Mead KC, Ames JB. Symptomatic lead toxicity and joint pain because of migration of shotgun pellets into the Hip 12 years after injury: A case report. JBJS Case Connect 2021;11:(2). doi: 10.2106/JBJS.CC.20.00751. [Google Scholar]
- 13.Rohlfing G, Refaat M, Kollmorgen R. Pseudotumor caused by a retained intra-articular bullet: A case report. JBJS Case Connect 2020;10:e0209. [Google Scholar]
- 14.Moisi MD, Page J, Gahramanov S, Oskouian RJ. Bullet fragment of the lumbar spine: The decision is more important than the incision. Glob Spine J 2015;5:523-6. [Google Scholar]
- 15.Benton JA, Rahme R, Krystal J, Holland R, Houten JK, Kinon MD. Retained bullet in the cervical spinal canal and the associated surgical management conundrum: Case report and review of the literature. Spinal Cord Ser Cases 2020;6:77. [Google Scholar]