This case underscores the rare diagnosis of multifocal skeletal tuberculosis, stressing the need for early intervention, multidisciplinary collaboration, and awareness of potential treatment delays with alternate medicine.
Dr. Ankith Chacko, Department of Orthopaedics and Spine Surgery, KIMS Health, Trivandrum, India. E-mail: ankithchacko02@gmail.com
Introduction: Tuberculosis (TB) remains a pervasive infectious disease, and extrapulmonary manifestations account for a significant proportion of cases. Skeletal involvement is observed in about 10% of extrapulmonary TB instances. While spinal TB is relatively common, sacroiliac (SI) joint TB is a rare occurrence, particularly in immunocompetent individuals.
Case Report: This case report discusses an unusual presentation in a 19-year-old immunocompetent lady where the spine, acetabulum, and SI joint were concurrently affected. The patient, initially undergoing alternative medicine, exhibited severe pain, weight loss, and restricted mobility. Radiological evaluations, including X-rays and magnetic resonance imaging, revealed extensive vertebral and pelvic destruction with abscess formation. Surgical debridement and stabilization, alongside antitubercular treatment, led to significant improvement.
Conclusion: This case emphasizes the challenges in diagnosing multifocal skeletal TB, highlights the importance of early intervention, and underscores the impact of alternative medicine on treatment delays. A multidisciplinary approach involving histopathological and microbiological examinations is crucial for optimal management.
Keywords: Multifocal skeletal tuberculosis, surgical intervention, antitubercular treatment.
Tuberculosis (TB) remains a significant infectious disease despite improvement in public health policies and recent developments in the antitubercular treatments (ATT). According to the World Health Organization, approximately 6.4 million cases of TB are reported in 2021 [1, 2]. Approximately 10% of patients with extrapulmonary TB exhibit skeletal involvement. Spine is the most common location of skeletal TB, with the Pott’s spine accounts for half of all musculoskeletal TB cases, followed by hip and knee [3, 4] affection of sacroiliac (SI) joints with TB is uncommon. The multifocal skeletal TB is exceedingly rare in non-immunocompromised individuals. This article reports an uncommon presentation of TB, where the spine, acetabulum, and SI joint are concurrently affected in an immunocompetent person.
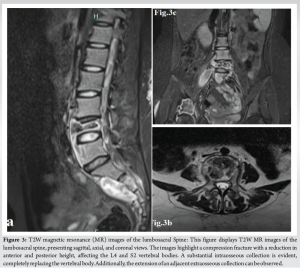
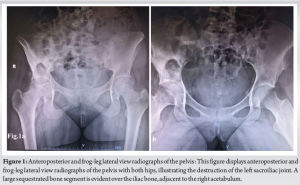
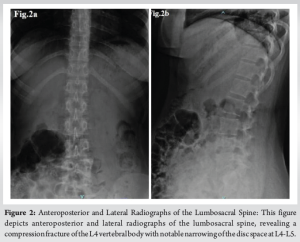
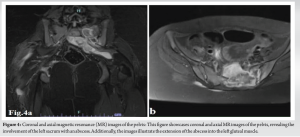
A 19-year-old lady reported to the spine clinic with a history of right hip and back pain persisting for 2 years. She has been undergoing alternative medicine (Siddha) treatment during this period. Three months before her visit to our clinic, she underwent surgical drainage for a swelling over the right gluteal area. The sample tested positive for tuberculous infection reverse transcription polymerase chain reaction, leading to the initiation of ATT. At the time of presentation, she was unable to walk due hip pain and back pain, accompanied by significant weight loss over the past few months. Notably, she did not exhibit any pulmonary symptoms. Clinical examination revealed tenderness over lumbosacral spine, right and left SI joints, and the right hip. The left hip appeared clinically normal. Movements of the lumbosacral spine and right hip were grossly restricted due to pain. The patient was unable to perform straight leg raise (SLR) and passive SLR was 50° bilaterally. She did not present with fever and her chest examination was clear. Hematological evaluation indicated anemia (hemoglobin: 10.9) and an elevated erythrocyte sedimentation rate (39 mm/h). Plain radiographs of pelvis and spine revealed destruction of left SI joint, sequestrum in the right iliac bone involving the acetabular wall, and narrowing of L4-L5 disc space with collapse of the L4 vertebral body. (Fig. 1 and 2) The magnetic resonance (MR) study of the lumbosacral region, including sagittal and axial T1-weighted, T2-weighted, and coronal short-tau inversion recovery (STIR) sequences (Fig. 3), revealed a compression fracture of L4 and S2 vertebral bodies, resulting in reduced anterior and posterior height. Notably, a large intraosseous collection (abscess) completely replaced the vertebral bodies. The collection within the L4 vertebral body measured 3.5 × 1.2 cm, with a subligamentous extension measuring 7.3 × 1.3 cm from the superior endplate of L3 to the inferior endplate of L5. This extension reached into the right psoas muscle, measuring 6.5 × 3.4 cm. In addition, the collection within the S2 vertebral body measured 3 × 2.3 cm, with an anterior subligamentous extension measuring 6.5 × 2.9 cm. This extension reached into the posterior elements through the left pedicle, causing compression over the thecal sac and impingement on nerve roots. Laterally, the abscess extended through the left lateral surface of the sacral promontory into the left SI joint and left greater sciatic foramen, reaching into the left gluteal muscles.
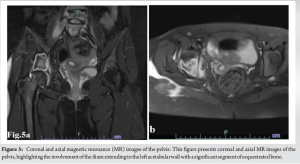
The T2/STIR study of the pelvis revealed a substantial collection measuring 8 × 7.6 cm in the sacral body and left sacral promontory (Fig. 4). The images also showed associated diffusion restriction. This collection extends into the left SI joint, with an inflammatory collection within the joint. Further extension is observed into the extraosseous plane through the greater sciatic foramen into the left gluteal muscles. Another hyperintense collection, displaying similar signal intensity, measures 5.4 × 4.5 cm noted in the right ilium, extending to the acetabular wall (Fig. 5). Multiple focal cortical defects noted, allowing the collection to extend into the extraosseous plane. Posterolaterally, it extended deep to the right gluteus muscles. Medially, the collection tracked adjacent to the right superior pubic ramus and was limited by the right pelvic diaphragm.
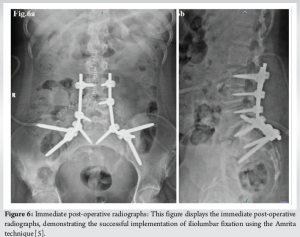
She underwent planned debridement with posterior stabilization, utilizing the Mercedes-Benz skin incision approach. During the procedure, the left hemisacrum was discovered to be entirely destroyed. Sequestrated bone fragments were removed, and the area debrided. Decompression of nerve roots was achieved with the assistance of a microscope. Posterior stabilization was accomplished through Iliolumbar fixation (Amrita technique [5]. and posterolateral fusion using morselized local autograft. The sequestrated bone in the iliac bone adjacent to the right acetabulum was not removed. She commenced anti-tubercular treatment, with the dosage adjusted according to her body weight. Immediate post-operative radiographs (Fig. 6) depict the iliolumbar fixation.
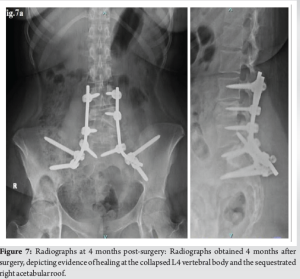
At the 4-month post-operative review, she demonstrated ambulation without support, although an abductor lurch was noted on the right side. The resolved back pain and improved general condition were corroborated by radiographs (Fig. 7), revealing signs of healing at the collapsed L4 vertebral body and the sequestrated acetabular area. Histopathological evaluations indicated necrotizing granulomatous inflammation, suggestive of tuberculous inflammation. Zehl–Neelsen staining yielded negative results for acid–fast bacilli, and acid–fast bacilli culture showed no growth even after 6 weeks of incubation period.
Multifocal skeletal TB refers to the simultaneous occurrence of osteoarticular lesions at two or more locations and is a rare manifestation, accounting for approximately 10–35% of extrapulmonary TB cases. While TB can affect various organs, multifocal skeletal involvement, initially termed “polycystic tuberculous osteitis” [6], was later replaced by the term “Multifocal bone TB” [7,8]. First clinically described in 1910 by Jungling, this condition is typically observed in immunocompromised individuals [9]. It is uncommon in immunocompetent individuals, particularly those without pulmonary involvement [10,11], making the presented case of multifocal skeletal TB in an immunocompetent patient unusual. The diagnosis and treatment of multifocal skeletal TB may be delayed due to the rarity and vague symptoms of the disease [12–14]. Radiological evaluation, including plain radiography (X-ray), computed tomography (CT), and MR imaging, may aid in early detection of the condition. The delay in diagnosing and delivering proper treatment may result in progression of disease with development of severe deformities including functional impairments. Lack of awareness among the general population or when the link between health provider and public is weak, along with involvement in alternative medical practices as observed in our case report, may hamper early optimal treatment. In general, tuberculous affections of the spine involve two adjacent vertebrae because one intervertebral artery supplies two adjacent vertebrae [3,15,16]. Usually, tuberculous infection begins from the anterior elements, and involvement of posterior elements is rare. The characteristic radiological findings in spinal TB include destruction of adjacent vertebral bodies with destruction of the intervening disc, along with epidural and paravertebral abscesses, which may track to various locations and can present as cold abscess. However, plain radiography is of little help in diagnosing a spinal TB unless disease is advanced and the disc is completely destroyed, leading to the narrowing of the intervertebral space or collapse of the vertebral body. In our case, the collapse of the L4 vertebral body and narrowing of the intervertebral space were evident. MRI is a more specific and sensitive modality in diagnosing skeletal TB at an earlier stage. The TB-affected vertebrae show hypointensity on T1W and heterogeneous increased signal on T2W MR images [17,18]. The disc appears as a bright signal on T2W images and decreases on T1W images and enhances after contrast administration. A hyperintense signal in a chronic scenario may be specific to TB, and the signal normalizes with treatment [19]. In our case, the osseous lesion and abscess were hyperintense on T2W and hypointense on T1W images. Frequently, TB sacroiliitis diagnosis is delayed until it presents as psoas abscess tracking to the groin or posterior thigh. In the presented case, she was initially seen at a local health-care center with buttock pain and swelling in the thigh, where it was surgically drained. Plain radiographs may not show early sacroiliitis; haziness or loss of articular line may be an early finding. CT, MRI, or bone scan may aid in early detection of the condition. TB sacroiliitis were classified by Kim et al. [20] to four types, according to severity of clinical and radiological findings. The presented case belongs to Type 4, in which lesions of SI joint with abscess formation or other affected vertebrae are included. There are two thoughts for the treatment for TB sacroiliitis. ATT without surgery is one method. The second option is surgery with ATT, which has the advantage of abscess drainage, confirmation of diagnosis, and the effects of arthrodesis, including pain relief [21–23]. The hip joint is the second most common site for TB after the spine, it constitutes 15–20% of skeletal TB [24,25]. Tuberculous bacteria may lodge in the synovium, epiphyseal or metaphyseal area of the head and neck of femur, greater trochanter, or acetabulum. When the lesion is located outside the joint, it may be present as an extra-articular or juxta-articular lesion. Extra-articular lesions may further progress to involve the joint [24]. In the presented case, the lesion found in the ilium extends to the acetabular wall, but the hip joint was not involved. We planned to manage the lesion non-surgically and did not attempt debridement.
Multifocal tuberculous osteomyelitis is a rare entity that can be associated with severe complications, necessitating a multidisciplinary approach. Multifocal skeletal TB must be considered in the differential diagnosis for patients presenting with multiple destructive osseous lesions. A high index of suspicion is crucial to prevent delay in diagnosis and to initiate early treatment, potentially averting devastating consequences. One reason for delayed optimal treatment initiation, as in the presented case, may be patients seeking alternative medicine. Histopathological and microbiological examinations are essential for confirming the diagnosis. Antitubercular chemotherapy (ATT), along with surgery in selected cases of deformities or neurological impairments, yields satisfactory outcomes.
- This case highlights the importance of considering TB as a potential diagnosis in patients presenting with multifocal skeletal involvement, even in rare locations such as the SI joint.
- The delayed presentation of the patient due to initial reliance on alternative medicine underscores the impact of treatment delays on disease progression.
- Managing multifocal skeletal TB requires a multidisciplinary approach involving histopathological and microbiological examinations along with early surgical and medical intervention.
References
- 1.Global Tuberculosis Report; 2022. Available from: https://www.who.int/publications-detail-redirect/9789240061729 [Last accessed on 2024 Apr 11]. [Google Scholar]
- 2.Falzon D, Zignol M, Bastard M, Floyd K, Kasaeva T. The impact of the COVID-19 pandemic on the global tuberculosis epidemic. Front Immunol 2023;14:1234785. [Google Scholar]
- 3.Garg RK, Somvanshi DS. Spinal tuberculosis: A review. J Spinal Cord Med 2011;34:440-54. [Google Scholar]
- 4.Pigrau-Serrallach C, Rodríguez-Pardo D. Bone and joint tuberculosis. Eur Spine J 2013;22:556-66. [Google Scholar]
- 5.Acharya NK, Bijukachhe B, Kumar RJ, Menon VK. Ilio-lumbar fixation-the amrita technique. J Spinal Disord Tech 2008;21:493-9. [Google Scholar]
- 6.Blankoff B. Osteitis tuberculous multiplex cystica (Jungling’s disease). Scalpel (Brux) 1957;110:835-43. [Google Scholar]
- 7.Komins C. Multiple cystic tuberculosis; a review and a revised nomenclature. Br J Radiol 1952;25:1-8. [Google Scholar]
- 8.Nataprawira HM, Ediwan NA, Diana IA, Dwiyana RF, Febrina D. Multifocal osteomyelitic tuberculosis at rare locations with metastatic tuberculosis abscess. Am J Case Rep 2019;20:503-7. [Google Scholar]
- 9.Dlimi F, Abouzahir M, Mahfoud M, Berrada MS, El Bardouni A, El Yaacoubi M. Multifocal bone tuberculosis: A case report. Foot Ankle Surg 2011;17:e47-50. [Google Scholar]
- 10.Marudanayagam A, Gnanadoss JJ. Multifocal skeletal tuberculosis: A report of three cases. Iowa Orthop J 2006;26:151-3. [Google Scholar]
- 11.De Araujo PS, de Melo HR, de Melo FL, Medeiros Z, Maciel MA, Florêncio R, et al. Multifocal skeletal tuberculosis in an immunocompetent patient: A case report. BMC Infect Dis 2015;15:235. [Google Scholar]
- 12.Yilmaz MH, Kantarci F, Mihmanli I, Kanberoglu K. Multifocal skeletal tuberculosis. South Med J 2004;97:785-7. [Google Scholar]
- 13.Hong L, Wu JG, Ding JG, Wang XY, Zheng MH, Fu RQ, et al. Multifocal skeletal tuberculosis: Experience in diagnosis and treatment. Med Mal Infect 2010;40:6-11. [Google Scholar]
- 14.Zhang L, Wang J, Feng X, Tao Y, Yang J, Zhang S, et al. Multifocal skeletal tuberculosis: A case report. Exp Ther Med 2016;11:1288-92. [Google Scholar]
- 15.Leowattana W, Leowattana P, Leowattana T. Tuberculosis of the spine. World J Orthop 2023;14:275-93. [Google Scholar]
- 16.Liu Z, Wang J, Chen GZ, Li WW, Wu YQ, Xiao X, et al. Clinical characteristics of 1378 inpatients with spinal tuberculosis in general hospitals in south-central China. Biomed Res Int 2019;2019:9765253. [Google Scholar]
- 17.Trivedi R, Saksena S, Gupta RK. Magnetic resonance imaging in central nervous system tuberculosis. Indian J Radiol Imaging 2009;19:256-65. [Google Scholar]
- 18.Gupta RK, Agarwal P, Rastogi H, Kumar S, Phadke RV, Krishnani N. Problems in distinguishing spinal tuberculosis from neoplasia on MRI. Neuroradiology 1996;38 (Suppl 1):S97-104. [Google Scholar]
- 19.Moore SL, Rafii M. Imaging of musculoskeletal and spinal tuberculosis. Radiol Clin North Am 2001;39:329-42. [Google Scholar]
- 20.Kim NH, Lee HM, Yoo JD, Suh JS. Sacroiliac joint tuberculosis. Classification and treatment. Clin Orthop 1999;358:215-22. [Google Scholar]
- 21.Rajasekaran S, Soundararajan DC, Shetty AP, Kanna RM. Spinal tuberculosis: Current concepts. Glob Spine J 2018;8(4 Suppl):96S-108. [Google Scholar]
- 22.Tuli SM. Results of treatment of spinal tuberculosis by “middle-path” regime. J Bone Joint Surg Br 1975;57:13-23. [Google Scholar]
- 23.Dhillon MS, Agashe V, Patil SD. Role of surgery in management of osteo-articular tuberculosis of the foot and ankle. Open Orthop J 2017;11:633-50. [Google Scholar]
- 24.Saraf SK, Tuli SM. Tuberculosis of hip: A current concept review. Indian J Orthop 2015;49:1-9. [Google Scholar]
- 25.Gautam D, Jain VK, Iyengar KP, Vaishya R, Malhotra R. Total hip arthroplasty in tubercular arthritis of the hip - Surgical challenges and choice of implants. J Clin Orthop Trauma 2021;17:214-7. [Google Scholar]