Adamantinoma recurrence highlights the significance of interdisciplinary care and long-term surveillance for the best possible patient outcomes.
Dr. Khalil Farooque, Department of Orthopedics, Shaukat Khanum Memorial Cancer Hospital and Research, Centre Lahore, Pakistan. E-mail: khalilfarooque@skm.org.pk
Introduction: Adamantinoma is a rare, locally aggressive bone tumor that primarily affects the long bones, with a predilection for the tibia. Although considered a low-grade malignancy, adamantinoma is notorious for its high propensity for recurrence, which poses significant clinical challenges in the management of affected individuals. This case report aims to explore the intricacies of recurrent adamantinoma of the tibia, shedding light on its clinical presentation, diagnostic modalities, treatment strategies, and prognostic factors.
Objective: This case report aims to evaluate surgical and functional outcomes of post-excision and reconstruction in recurrent adamantinoma.
Case Report: This retrospective case report includes the patient who presented in Shaukat Khanum Memorial Cancer Hospital and Research Center Lahore with recurrent adamantinoma. Data were collected after patient’s written and informed consent, and a retrospective analysis of the patient’s demographics was done with the Statistical Package for the Social Sciences using the information in the Hospital Information System with a predesigned pro forma. Histology slides were collected from the Department of Pathology. Variables that were included are categorized into demographics, history and examination findings, site, and size of the primary tumor, radiological findings, histological type, stage, and resection margins. The patient underwent wide margin excision and reconstruction with free vascularized fibula graft and his functional outcome was evaluated using the musculoskeletal tumor society score which showed good functional outcome.
Conclusion: Despite therapeutic challenges, wide excision of the tumor followed by free vascularized fibula grafting for reconstruction is a viable option to treat such patients where advanced prosthesis and allografts are not available.
Keywords: Case report, adamantinoma, recurrence, vascularized free fibula graft.
Adamantinoma is a rare primary bone tumor that primarily affects the long bones, most commonly the tibia [1]. Adamantinoma of the tibia was first described by Fischer in 1913 [2]. It accounts for a mere 0.1–0.5% of all primary bone tumors, rendering it an exceedingly rare pathology. Despite its infrequency, adamantinoma warrants attention due to its unique histological features, characterized by the presence of epithelial and osteofibrous components. This distinct histology contributes to the challenges in diagnosis and treatment. Recurrence remains a hallmark of adamantinoma, with reported rates ranging from 20% to 50% [3-5]. The reasons behind this high recurrence rate are multifactorial, including incomplete initial excision, the tumor’s locally infiltrative nature, and a paucity of effective adjuvant therapies [6]. Understanding the factors contributing to recurrence is imperative for improving patient outcomes and reducing the burden of this disease. This case report explores a recurrent adamantinoma case and delves into the clinical and pathological aspects, along with the management strategies for this enigmatic bone tumor.
A 23-year-old male presented in the outpatient department with biopsy-proven adamantinoma for which excision, curettage, and bone cementing were done in another hospital 15 days back before presentation in our hospital (Fig. 1). On examination, there was an 8 cm scar present on the anterior aspect of the left distal tibia which is healed by primary intention. No swelling was palpable below the scar and his neurovascular bundle was intact. The patient was re-scanned in our hospital to look for any possible residual disease and metastasis. On magnetic resonance imaging (MRI) of his leg, there were only post-surgical changes with no evidence of any residual disease; however, his computed tomography chest showed indeterminate subpleural nodule. The case was discussed in a multi-disciplinary team (MDT) meeting including orthopedic surgeons, oncologists, and radiation oncologists, and it was decided to keep the patient on close follow-up at 3-month intervals. The patient had stable disease on subsequent scans for 9 months when a recent MRI left lower limb showed an abnormal signal intensity area identified along the superolateral aspect along the surgical cavity showing post-contrast enhancement with diffusion restriction appearing suspicious for infective etiology/recurrence (Fig. 2). Hence, the case was again discussed in MDT and it was decided to get the patient’s infective profile and biopsy of the lesion. The patient’s infective profile came out to be negative. Moving forward ultrasound-guided trucut biopsy was performed to confirm the diagnosis, and histopathological examination revealed the characteristic biphasic pattern with epithelial nests within a fibrous stroma confirming the recurrence of the disease (Fig. 3). The patient was again discussed in MDT and radical resection of the tumor was decided. The surgical plan was discussed with the patient in detail and then after careful deliberation, the patient underwent a wide surgical resection followed by a limb-salvaging reconstruction procedure using a vascularized free fibula graft taken from the ipsilateral limb (Fig. 4 and 5). The patient had a smooth post-operative recovery and was discharged home after 5 days and was advised regular clinic follow-up. The patient was kept in a splint for about a month, and then, a range of motion exercises were advised. Partial weight-bearing was started at 2 months and full weight-bearing was allowed after 3 months. On the current 11-months follow-up, the patient had a revised musculoskeletal tumor society score of 24 which represents good functional outcome.
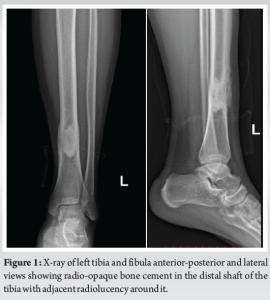
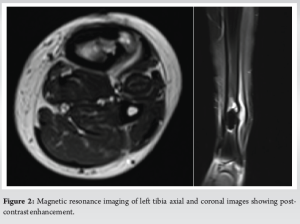
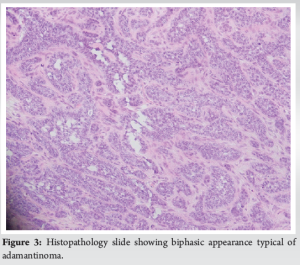

Adamantinoma is a rare entity, and recurrent cases are even more infrequent. This recurrent adamantinoma case underscores several important clinical and therapeutic aspects. The hallmark of adamantinoma is its biphasic histology, which includes both epithelial and stromal components [7]. This distinct histological pattern can assist in diagnosis and differentiation from other bone tumors. Individuals who have long bone adamantinoma frequently experience pain and gradually increasing swelling, and they may have experienced trauma in the affected location in the past [3]. Radiologically, adamantinoma is characterized by an eccentric, expansive, and osteolytic appearance; skip lesions, cortical disintegration, and moth-eaten edges are frequently observed [8]. Information regarding intramedullary extension and tumor-free margins can be obtained using MRI [9]. Adamantinoma is known for its propensity to recur after surgical resection, emphasizing the need for vigilant follow-up in treated patients. The mechanisms underlying this tendency are not yet fully understood, highlighting the importance of ongoing research in the field. Adamantinoma can spread to other areas and has a high probability of local recurrence. In a retrospective analysis, Houdek et al. found that 15% of 46 patients with surgically treated adamantinoma of the extremities experienced local recurrence [10]. According to Qureshi et al.’s assessment of 70 patients who underwent surgery for long bone adamantinoma, the local recurrence rate was 18.6% [3]. In addition, Scholfield et al. observed that following surgical therapy, three out of 12 patients with osteofibrous dysplasia-like adamantinoma developed a local recurrence [11]. Furthermore, long-term follow-up research showed that 27% of patients experienced metastasis, with the lung being the most common site [3]. The mean duration for a local recurrence was 8 years, and the mean duration for metastasis was 7 years in the prior study. The management of recurrent adamantinoma often necessitates a multidisciplinary approach, involving orthopedic surgeons, oncologists, and radiation specialists. Decisions regarding surgical techniques and the timing of radiation therapy must be individualized to each patient’s case [12]. Limb-salvaging surgery is considered in recurrent adamantinoma cases to maintain function and quality of life. The choice of surgical technique depends on the extent of the recurrence, patient factors, and the surgeon’s experience. Different modalities can be considered when deciding on local control of the disease with their pros and cons. Options of wide local excision alone, or with reconstructive limb salvaging procedures can be considered using autografts or allografts, or endoprosthesis. Rarely, patients may require amputation for non-reconstructable tumors [3].
Recurrent adamantinoma is an uncommon but challenging clinical scenario. This case report highlights the importance of early diagnosis, comprehensive evaluation, and a multidisciplinary approach in the management of recurrent adamantinoma. While surgical resection remains the primary mode of treatment, the propensity for recurrence underscores the need for vigilant follow-up and research to better understand the underlying mechanisms. This enigmatic bone tumor continues to pose clinical challenges, and further studies are essential to improve our understanding and treatment outcomes for adamantinoma patients.
Recurrent incidents of adamantinoma highlight a clinical message that underscores the need of continuing surveillance and interprofessional teamwork. To improve patient outcomes and quality of life, it emphasizes the necessity of maintaining vigilant monitoring even after initial therapy, ensuring prompt discovery and management of recurrences. This stresses the significance of a patient-centered approach that incorporates multidisciplinary interventions and routine follow-ups to properly manage the intricacies of this uncommon malignancy.
References
- 1.Moon NF, Mori H. Adamantinoma of the appendicular skeleton-updated. Clin Orthop Relat Res (1976-2007) 1986;204:215-37. [Google Scholar]
- 2.Fischer B. Uber ein primares adamantinoma der tibia. Z Pathol 1913;12:422-41. [Google Scholar]
- 3.Qureshi AA, Shott S, Mallin BA, Gitelis S. Current trends in the management of adamantinoma of long bones: An international study. J Bone Joint Surg 2000;82:1122-31. [Google Scholar]
- 4.Keeney GL, Unni KK, Beabout JW, Pritchard DJ. Adamantinoma of long bones. A clinicopathologic study of 85 cases. Cancer 1989;64:730-7. [Google Scholar]
- 5.Jain D, Jain VK, Vasishta RK, Ranjan P, Kumar Y. Adamantinoma: A clinicopathological review and update. Diagn Pathol 2008;3:8. [Google Scholar]
- 6.Varvarousis DN, Skandalakis GP, Barbouti A, Papathanakos G, Filis P, Tepelenis K, et al. Adamantinoma: An updated review. In Vivo 2021;35:3045-52. [Google Scholar]
- 7.Lucas RB, Thackray AC. The histology of adamantinoma. Br J Cancer 1951;5:289. [Google Scholar]
- 8.Khanna M, Delaney D, Tirabosco R, Saifuddin A. Osteofibrous dysplasia, osteofibrous dysplasia-like adamantinoma and adamantinoma: Correlation of radiological imaging features with surgical histology and assessment of the use of radiology in contributing to needle biopsy diagnosis. Skeletal Radiol 2008;37:1077-84. [Google Scholar]
- 9.Van der Woude HJ, Hazelbag HM, Bloem JL, Taminiau AH, Hogendoorn PC. MRI of adamantinoma of long bones in correlation with histopathology. Am J Roentgenol 2004;183:1737-44. [Google Scholar]
- 10.Houdek MT, Sherman CE, Inwards CY, Wenger DE, Rose PS, Sim FH. Adamantinoma of bone: Long‐term follow‐up of 46 consecutive patients. J Surg Oncol 2018;118:1150-4. [Google Scholar]
- 11.Scholfield DW, Sadozai Z, Ghali C, Sumathi V, Douis H, Gaston L, et al. Does osteofibrous dysplasia progress to adamantinoma and how should they be treated? Bone Joint J 2017;99:409-16. [Google Scholar]
- 12.Rastogi S, Varshney MK, Trikha V, Khan SA, Choudhury B, Safaya R. Treatment of adamantinoma of long bones: An evolving concept. Clin Orthop Relat Res 2010;468:2461-6. [Google Scholar]









