Physeal growth arrest in distal radius fractures, while uncommon, can present with ulnar-sided pain and positive ulnar variance that is treatable with ulnar shortening osteotomy
Mr. Brian Le, Department of Orthopaedics, Children's Hospital New Orleans, Louisiana, USA. E-mail: ble3@tulane.edu
Introduction: Distal radius fractures account for nearly one-third of all pediatric fractures, making it among the most common of all pediatric fractures. Studies report that distal radius physeal arrest rates following trauma to the distal radius seem to occur in only about 5% of patients. Significant ulnar variance can develop leading to notable pain and limitations in function.
Case Report: We present a case of a 17-year-old right-hand dominant adolescent Caucasian male with persistent ulnar wrist pain. The patient presented to our outpatient clinic for evaluation of his left wrist following 6–8 months of persistent ulnar-sided pain. Ten months prior, the patient had fallen off a shed and was treated in the emergency room and referred to the outpatient clinic for follow-up. The patient initially sustained a Salter–Harris Type 2 distal radius fracture treated with closed reduction and short arm cast application in the emergency room. The short arm cast was removed at 8 weeks, and then, the patient was placed in a brace. The patient was lost to follow-up before returning to the clinic 16 months after the original injury when he noticed worsening pain in the left wrist, localized to the distal radioulnar joint with increased hand usage at a new job. Radiographs at that time showed a worsening positive ulnar variance as well as a partially open distal ulnar physis. After 6 months of occupational therapy and over-the-counter pain management, the ulnar-sided pain had not resolved. The radiograph showed a positive Ulna variance of 2.5 mm, which was corrected with a 5 mm excision osteotomy of the distal ulna. The patient reported significant pain relief and a 42-point improvement in his patient-rated wrist evaluation score.
Conclusion: Distal radius growth arrest, while uncommon, can present with ulnar-sided pain and positive ulnar variance that is safely treatable with ulnar shortening osteotomy.
Keywords: Distal radius fracture, growth arrest, ulnar variance.
Distal radius fractures account for nearly one-third of all pediatric fractures, making it among the most common of all pediatric fractures [1]. Growth abnormalities such as sequela to distal radius fractures are both uncommon and often unnoticed. Studies report that distal radius physeal arrest rates following trauma to the distal radius seem to occur in only about 5% of patients [2]. In those cases, significant ulnar variance can develop leading to notable pain and limitations in function. We present a case of an adolescent male with persistent ulnar wrist pain due to distal radius growth arrest secondary to trauma that was corrected with an acute ulnar shortening osteotomy (USO).
A 17-year-old right-hand dominant adolescent caucasian male presented to our outpatient clinic for evaluation of his left wrist following 6–8 months of persistent ulnar-sided pain. 10 months prior the patient had fallen off a shed and was treated in the emergency room and referred to the outpatient clinic for follow-up. The patient initially sustained a Salter–Harris Type 2 distal radius fracture treated with closed reduction and short arm cast application in the emergency room (Fig. 1-3).
The patient was reviewed in the clinic in 3, 4, 5, and 8 weeks with serial radiographs. The short arm cast was removed at 8 weeks and then the patient was placed in a brace. The pain was well controlled with over-the-counter pain medication. The patient was subsequently lost to follow-up. The patient took up a job in construction and with increased hand usage he noticed worsening pain in the left wrist, localized to the distal radioulnar joint (DRUJ). The patient returned to the clinic 16 months after the original injury with complaints of pain. The patient’s range of motion at the wrist were: 40° of flexion, 20° of extension, full pronation, and 30° of supination. Radiographs at that time showed a worsening positive ulnar variance as well as a partially open distal ulnar physis. The patient was placed back in a brace and referred to occupational therapy (Fig. 4).
Six months later, that is, 22 months after the initial injury, after occupational therapy and over-the-counter pain management, the ulnar-sided pain had not resolved. The pain caused the patient to leave work repeatedly, which prompted further evaluation. On clinical examination, the left wrist was tender to palpation at the distal ulna and ulnar styloid. The wrist exhibited 60° of flexion and 40° of extension with full pronation and supination.
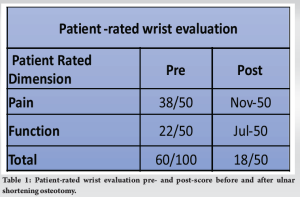
Wrist function was evaluated using the patient-rated wrist evaluation (PRWE) score. The PRWE is a patient-reported outcome tool to measure both the patient’s rating of pain and function following a distal radius fracture [3]. While the tool does not stratify patients based on score, a change over time of 11.5 is a recommended minimally detectable change to be perceived as beneficial to the patient [4]. The patient had an initial PRWE score of 60/100 (Table 1).
Radiographically, the patient demonstrated a healed left distal radius fracture, with 2.5-mm ulnar positive variance. The positive ulnar variance measured using the adapted perpendicular method was 2.5 mm. The adapted perpendicular method is recommended for patients with skeletal ages ≥14 years [5]. Immediate post-injury reduction radiograph showed a negative ulna variance of 2.5 mm which was considered to be a baseline for this patient. Therefore, it was planned to shorten the ulna by 5 mm. A magnetic resonance imaging was obtained to rule out any other significant pathology which revealed a mild lunate contusion and a distal triangular fibrocartilage complex (TFCC) tear; however, the triangular cartilage was intact.
An USO was performed under general anesthesia. A 5-mm excision osteotomy was planned through a direct approach of the distal ulna. An Acumed ulnar osteotomy plate (Acumed, Hillsboro, OR, USA) was secured using a Kirschner wire, and the plate position was verified through fluoroscopy. The osteotomy guide was attached to the plate and a microsagittal saw was utilized to resect a 5-mm bone block. The osteotomy site was reduced with compression utilizing the plate. Lag screws were used to secure the compression and the rest of the plate was secured by additional screws (Fig. 5-7).
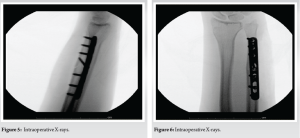
The patient was placed in an univalved short arm cast. The univalved cast was switched to a soft brace at 8 weeks and began physical therapy for strengthening and range of motion. At the 8 week follow-up radiographic imaging confirmed adequate union and the post-operative PRWE score improved to 18/100 (Fig. 8).
Distal physeal growth arrest remains a rare occurrence despite the prevalence of distal radius fractures in the pediatric population. Type 2 Salter–Harris fractures predominate, making up 75% of physeal fractures [6]. While most forearm bone length discrepancies <1 cm are asymptomatic, it is known that even an ulnar length discrepancy of 2.5 mm can increase ulnar load from 18.4% to 42.0% of the total axial load [7]. In this case, a discrepancy of 2.5 mm in addition to a 30% tear in the distal TFCC caused progressive ulnar-sided pain for the patient, which warranted surgical intervention. Indications for surgical interventions are multifactorial including growth potential, nature of the deformity, and patient expectations [7]. Skeletal maturity guides decision-making regarding which method would be most beneficial for the patient. Skeletally mature patients would benefit from an USO, while a skeletally immature patient would benefit from an ulnar epiphysiodesis combined with USO [7]. In contrast, lengthening osteotomy of the radius is also an option [8]. In the case presented, the patient did not have enough potential for growth, and therefore, it was decided that he would benefit most from a USO. The literature surrounding the management of distal radial physeal arrest is growing, but there is a relative lack of consensus about the surgical management of larger variances. Even though >10 mm ulnar variance has been observed to be asymptomatic, ulnar impaction syndrome and ulnar-sided pain are observed in as little as 2.5 mm. One potential complication of ulnar shortening to relieve ulnar-sided pain is, worsening DRUJ incongruence. Radial corrective osteotomy is indicated in the displacement of the radius >10° in the sagittal plane [9]. Reducing ulnar variance to a neutral variance is necessary to minimize ulnar-sided pain. Previous literature had suggested the ulna should be shortened to a variance of −1 mm, but had a higher rate of osteoarthritis of the DRUJ, so a neutral variance would be needed to adequately relieve ulnar-sided pain [10]. Physeal bar resection is a consideration if there is a larger growth potential when the ulnar variation is identified early in a partial physeal bar arrest. Alternatively, an epiphysiodesis of the ulna could also be performed in a partial arrest to minimize the ulnar variance [7]. In this patient’s case, however, given his age, growth potential is limited and with a normal radial alignment, an USO was ultimately performed [2]. Despite the paucity of literature about the management of distal radial growth arrest, it was found on an average that a positive ulnar variance of 4.5 mm could be corrected with surgery with positive outcomes [11]. Cha et al. utilizing USO to manage 22 patients with ulnar impaction syndrome secondary to trauma published a case series. In these cases, the patients had both open physes with some growth potential and some closed physes with no growth potential. They reduced the mean ulnar variance of 2.91 mm to a more neutral variance of 0.23 mm. All of the patients in the study healed without substantial complications [12]. Waters et al. presented a case series of 30 patients with an average age of 14.8 years. In this study, patients were treated with ulnar epiphysiodesis, USO, radial osteotomy, or a combination of radial and ulnar epiphysiodesis. The average ulnar variance was 4.5 mm which was corrected to a neutral variance [8]. Waters found that surgical intervention for post-traumatic distal radial growth arrest can improve pain and mobility in symptomatic patients, and while preventative in asymptomatic patients. Hassan et al. published a case series on 20 patients who presented with positive ulnar variance after distal radius trauma. All 20 were treated with short oblique USO. Patients in this study had an average ulnar reduction of 5.74 mm with a mean pre-operative PRWE of 70.4 with a mean post-operative score of 17.2. The authors did caution that for dorsal tilt >20° and volar malunion >10°, multidirectional deformities usually require a distal radius osteotomy [13].
Long-term complications of a distal radius fracture can present with ulnar-sided pain due to physeal growth arrest and a resulting positive ulnar variance. This condition can be safely treated with an USO with favorable patient-rated outcomes.
This case report demonstrates the importance of potential healing complications of a distal radius fracture in adolescents. Physeal growth arrest and a resulting positive ulnar variance can present with ulnar-sided pain. This condition can be treated with an USO.
References
- 1.Randsborg PH, Gulbrandsen P, Šaltyte Benth J, Sivertsen EA, Hammer OL, Fuglesang HF, et al. Fractures in children: Epidemiology and activity-specific fracture rates. J Bone Joint Surg Am 2013;95:e42. [Google Scholar]
- 2.Bellaire L, Vuillermin C, Steinman S, Truong W, Bae D, Wallace CD, et al. Traumatic physeal arrests at the wrist: Current concept review. J Pediatr Orthop Soc N Am 2021;3:265. [Google Scholar]
- 3.MacDermid JC, Turgeon T, Richards RS, Beadle M, Roth JH. Patient rating of wrist pain and disability: A reliable and valid measurement tool. J Orthop Trauma 1998;12:577-86. [Google Scholar]
- 4.Walenkamp MM, De Muinck Keizer RJ, Goslings JC, Vos LM, Rosenwasser MP, Schep NW. The minimum clinically important difference of the patient-rated wrist evaluation score for patients with distal radius fractures. Clin Orthop Relat Res 2015;473:3235-41. [Google Scholar]
- 5.Kox LS, Jens S, Lauf K, Smithuis FF, Van Rijn RR, Maas M. Well-founded practice or personal preference: A comparison of established techniques for measuring ulnar variance in healthy children and adolescents. Eur Radiol 2020;30:151-62. [Google Scholar]
- 6.Ellanti P, Harrington P. Acute ulnar shortening for delayed presentation of distal radius growth arrest in an adolescent. Case Rep Orthop 2012;2012:928231. [Google Scholar]
- 7.Samora JB. Distal radius physeal bar and ulnar overgrowth: Indications for treatment. J Pediatr Orthop 2021;41:S6-13. [Google Scholar]
- 8.Waters PM, Bae DS, Montgomery KD. Surgical management of posttraumatic distal radial growth arrest in adolescents. J Pediatr Orthop 2002;22:717-24. [Google Scholar]
- 9.Löw S, Mühldorfer-Fodor M, Pillukat T, Prommersberger KJ, Van Schoonhoven J. Ulnar shortening osteotomy for malunited distal radius fractures: Results of a 7-year follow-up with special regard to the grade of radial displacement and post-operative ulnar variance. Arch Orthop Trauma Surg 2014;134:131-7. [Google Scholar]
- 10.Cha SM, Shin HD, Kim KC, Park E. Ulnar shortening for adolescent ulnar impaction syndrome: Radiological and clinical outcomes. J Hand Surg 2012;37:2462-67. [Google Scholar]
- 11.Gauger EM, Casnovsky LL, Gauger EJ, Bohn DC, Van Heest AE. Acquired upper extremity growth arrest. Orthopedics 2017;40:e95-103. [Google Scholar]
- 12.Cha SM, Shin HD, Kim YK, Lee KW. Ulnar shortening osteotomy for posttraumatic ulnar impaction syndrome in adolescent (younger than 18 years)-Based on the Cha and Shin assessment. Injury 2022;53:4038-47. [Google Scholar]
- 13.Hassan S, Shafafy R, Mohan A, Magnussen P. Solitary ulnar shortening osteotomy for malunion of distal radius fractures: Experience of a centre in the UK and review of the literature. Ann R Coll Surg Engl 2019;101:203-7. [Google Scholar]