Implement a comprehensive patient evaluation to uncover contributing factors like concurrent medical conditions, adopt a multifaceted approach to address both the deformity and associated illnesses and balance patient perspectives and surgical recommendations for optimized recovery.
Dr. Arpit Agrawal, Department of Orthopaedics, Sri Ramachandra Institute of Higher Education and Research, Chennai - 600056, Tamil Nadu, India. E-mail: arpitagrawal411@gmail.com
Introduction: Fixed flexion deformity (FFD) following total knee arthroplasty occurs in approximately 4% of patients undergoing primary total knee arthroplasty. Treatment modalities for significant disabling FFD post-arthroplasty encompass manipulation under anesthesia, osteophyte resection, soft tissue release, peroneal nerve decompression, and revision knee replacement.
Case Report: A 43-year-old lady, a known case of rheumatoid arthritis and psoriasis, presented with fixed flexion contracture of the left knee following total knee arthroplasty. The range of motion (ROM) at the left knee was 60°–110°. With the help of the plastic surgery team, the patient underwent an extensive posterior soft tissue release. Intra-operatively, the ROM achieved was 5°–110°. After 3 weeks, the patient was mobilized with full weight bearing with a knee brace. But unfortunately, there was a gradual recurrence of deformity at 3-month follow-up in spite of adequate and aggressive rehabilitation.
Conclusion: Patients with FFD for more than 2 years following a total knee arthroplasty may not benefit from extensive radical posterior soft tissue release. Revision knee replacement may be the better option.
Keywords: Fixed flexion deformity, total knee arthroplasty, idiopathic stiffness, treatment modalities, post-operative complications.
According to Tibbo et al. [1], a fixed flexion deformity (FFD) is an acquired idiopathic stiffness. The prevalence of acquired idiopathic stiffness after primary total knee arthroplasty in 35 studies was 4%. Various causes for FFD are arthritis, post-total knee arthroplasty, contractures due to burns and trauma, prolonged immobilization, etc. [2] FFD, also called flexion contracture, is relatively rare but a demanding functional limitation that both surgeons and patients may have to deal with [3]. Various factors affecting FFD following total knee arthroplasty include implant design, surgical technique, reduced preoperative range of motion (ROM), trauma sequelae, prior knee surgery, inflammatory diseases, and incipient arthrofibrosis [4]. As mentioned by Kyriakidis et al. [5] in their paper “Mid-term outcomes of posterior capsular release for fixed flexed deformity after total knee arthroplasty,” various treatment modalities for FFD developed post-total knee arthroplasty are manipulation under general anesthesia, meticulous resection of the osteophytes and over-resection of the distal femur, combined posterior soft-tissue release (posterior capsule and hamstring tendons) with prophylactic peroneal nerve decompression and botulinum toxin Type A injection and revision surgery for painful post-operative flexion contractures.
A 43-year-old lady presented with chief complaints of pain and difficulty in walking for 6 months. The patient, a known case of inflammatory arthritis (rheumatoid arthritis + psoriasis), had undergone left total knee replacement in 2019. She had significant flexion contracture postoperatively, for which a posterior-medial hamstring release was done elsewhere in 2021, which did not lead to any improvement. The flexion deformity at the left knee gradually worsened, making the patient unable to bear weight over the affected limb for the past 6 months (Fig. 1 and 2). The ROM of the left knee was from 60° to 110° (FFD of 60°). She also had arthritic involvement of multiple other joints, which was making her ambulation difficult with the deformity.
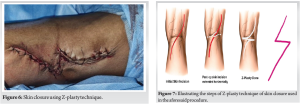
X-rays of the left knee confirmed a well-fixed total knee prosthesis (Fig. 3) without any implant loosening. Given the stable implant, a posterior soft tissue release was chosen to address the flexion contracture. Unfortunately, prior conservative measures, including physiotherapy, bracing, and traction, proved ineffective in improving knee flexion. Therefore, surgery was deemed necessary to correct the deformity. The other option would have been a revision of the total knee prosthesis to increase the extension gap. It was anticipated that an extensive posterior release would be required after isolating the critical neurovascular structures for which plastic surgical help was sought. The plastic surgery team was also involved in the decision-making in anticipation of difficulty in soft tissue closure following the release. Under general anesthesia with the patient in the prone position and under tourniquet control (total tourniquet time-11/2 h), the previous posteromedial longitudinal surgical scar was incised and extended distally over the proximal third leg region. The popliteal artery, tibial nerve, and common peroneal nerve were identified and isolated (Fig. 4) by the plastic surgical team aided by magnification. The hamstrings (medial and lateral) and posterior capsule (prosthesis was visualized) were incised and released through the two windows on either side of the popliteal artery. The medial gastrocnemius was also erased from origin on the medial femoral condyle. Partial release of the medial collateral ligament and posterior cruciate ligament was done. The biceps femoris was cut at the level of insertion. The short saphenous vein, sural nerve, and saphenous vein were sacrificed to facilitate exposure. Following the release, the knee could be easily extended to near full extension (Fig. 5). Following the dissection of soft tissues, closure was done by the plastic surgical team. Z-plasty of the skin was done to facilitate closure (Fig. 6 and 7). The drain was placed in situ. The leg was splinted with an above-knee splint, both anteriorly and posteriorly.
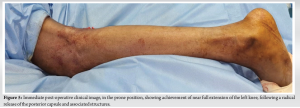
The patient was on an anterior and posterior slab to maintain the correction. Once the wound sutures were removed at 3 weeks postoperatively, the patient was started on total weight-bearing mobilization with a knee brace. The active ROM at 6-week follow-up was 15°–110° with 15° residual flexion contracture (Fig. 8 and 9).

However, as we further followed up with the patient, the patient continued total weight-bearing mobilization with a knee brace. Still, the residual flexion of the left knee by the end of 10 weeks was increased up to 25° with a ROM from 25° to 110°. There was a gradual worsening of the flexion, possibly resulting from inadequate bracing at night time noticed at this follow-up. Considering the patient’s ongoing debilitating illness, could we consider this as a good outcome?
A 43-year-old lady had developed significant fixed flexion contracture of the left knee following a total knee replacement, which was done 4 years back. The prosthesis was well fixed, so it was decided to do a radical posterior soft tissue release assisted by the plastic surgical team. A limited posteromedial release done previously had already failed, so the decision was taken for a more radical release. Radical posterior release was done as described. There was an excellent correction of FFD to an acceptable degree, which translated to a good functional outcome. A patient who had not ambulated for the past 6 months was started on ambulatory mobilization 3 weeks following surgery. She found walking easier even though the left knee had a mild persistent flexion contracture. But unfortunately on follow-up of the patient, there was a worsening of the flexion contracture to nearly 30° at 3-month follow-up. The patient was finding it more difficult to walk as the flexion contracture recurred. Even though the short-term and immediate outcome was good, the medium-term follow-up showed a recurrence of deformity which would have translated to a poor long-term result. Kyriakidis et al. [5], in their paper “Mid-term outcomes of posterior capsular release for fixed flexed deformity after total knee arthroplasty,” mentioned various treatment modalities for FFD developed post-total knee arthroplasty. A less invasive option is manipulation under anesthesia (MUA), which is most effective within the first 3 months of the index procedure and in minor FFD. Indeed, in their retrospective study, Namba and Inacio [6] concluded that flexion contractures are not significantly improved after late MUA (after 90 days). Moreover, Cates and Schmidt [7] reported that this technique is associated with poor outcomes in the case of extensive flexion contractures. Bellemans et al. [8] confirmed the efficacy of posterior capsular release in concomitance with bone resections through their four-step algorithm to correct flexion contracture in primary total knee arthroplasty. They described that almost 99% of knees with flexion contracture under 30° could be rectified with posterior capsular release, meticulous resection of the osteophytes, and over-resection of the distal femur. In their retrospective review, Vahedi et al. [9] recently described a more invasive procedure. They combined all the following methods: Posterior capsular release, hamstring tenotomy, prophylactic peroneal nerve decompression (at the level of the fibular neck and head by cutting both fascial bands that pass over the nerve and the deep intermuscular septum between the anterior and lateral compartments), and botulinum toxin Type A injections (150–200 units in both the gastrocnemius and hamstring muscles each). Nineteen patients (21 knees) were included in their study, with a knee mean flexion contracture of 27° before surgery. At the final follow-up of 2 years, they reported a significant improvement as all patients regained full extension to 5° of hyperextension. Fehring et al. [10] evaluated the efficacy of revision surgery for painful post-operative flexion contractures. They reported good clinical and functional outcomes at an average of 79-month follow-up. Extension improved from an average of 32.9° preoperatively to 2.9° postoperatively. They concluded that revision surgery for significantly symptomatic flexion contractures after total knee arthroplasty could improve ROM and diminish pain. This suggests that whatever the reasons for developing a fixed flexion contracture following total knee replacement, be it a tight gap between the femoral and tibial components of the implant, inadequate implant insertion, overstuffing of the extension gap, inadequate post-operative rehabilitation or any underlying conditions such as rheumatoid arthritis/inflammatory arthritis, a radical posterior capsular release may be beneficial. Several factors may have contributed to the development of flexion contracture after total knee arthroplasty (TKR) in this case. These include incomplete treatment of pre-existing inflammatory arthritis, insufficient physiotherapy or inadequate strengthening of the quadriceps muscles, and limited patient adherence to rehabilitation protocols before surgery. The reasons for recurrence likely involve inconsistent use of a night splint, persistence of the underlying inflammatory condition, and continued challenges with patient compliance.
Patients with fixed flexion contracture following total knee arthroplasty may not benefit from a radical posterior capsular release. Even though this is a single case report, the case illustrates the high risk of recurrence of flexion deformity following this extensive procedure. There are also very few clinical case series in this regard. Hence, surgeons should be cautious and probably revision knee replacement, and increasing the extension gap may be a better option.
Radical posterior release may not be effective in the correction of FFD following total knee replacement when the extension gap is tight.
References
- 1.Tibbo ME, Limberg AK, Salib CG, Ahmed AT, van Wijnen AJ, Berry DJ, et al. Acquired idiopathic stiffness after total knee arthroplasty: A systematic review and meta-analysis. J Bone Joint Surg Am 2019;101:1320-30. [Google Scholar]
- 2.Su EP. Fixed flexion deformity and total knee arthroplasty. J Bone Joint Surg Br 2012;94(11 Suppl A):112-5. [Google Scholar]
- 3.Cheng K, Ridley D, Bird J, McLeod G. Patients with fixed flexion deformity after total knee arthroplasty do just as well as those without: Ten-year prospective data. Int Orthop 2010;34:663-7. [Google Scholar]
- 4.Khatri K, Bansal D, Rajpal K. Management of flexion contracture in total knee arthroplasty. In: Knee Surgery - Reconstruction and Replacement. London: IntechOpen; 2020. [Google Scholar]
- 5.Kyriakidis T, Tasios N, Vandekerckhove B, Verdonk P, Cromheecke M, Verdonk R. Mid-term outcomes of posterior capsular release for fixed flexed deformity after total knee arthroplasty. Acta Orthop Belg 2022;88:329-34. [Google Scholar]
- 6.Namba RS, Inacio M. Early and late manipulation improve flexion after total knee arthroplasty. J Arthroplasty 2007;22(6 Suppl 2):58-61. [Google Scholar]
- 7.Cates HE, Schmidt JM. Closed manipulation after total knee arthroplasty: Outcome and affecting variables. Orthopedics 2009;32:398. [Google Scholar]
- 8.Bellemans J, Vandenneucker H, Victor J, Vanlauwe J. Flexion contracture in total knee arthroplasty. Clin Orthop Relat Res 2006;452:78-82. [Google Scholar]
- 9.Vahedi H, Khlopas A, Szymczuk VL, Peterson MK, Hammouda AI, Conway JD. Treatment with posterior capsular release, botulinum toxin injection, hamstring tenotomy, and peroneal nerve decompression improves flexion contracture after total knee arthroplasty: Minimum 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 2020;28:2706-14. [Google Scholar]
- 10.Fehring TK, Odum SM, Griffin WL, McCoy TH, Masonis JL. Surgical treatment of flexion contractures after total knee arthroplasty. J Arthroplasty 2007;22(6 Suppl 2):62-6. [Google Scholar]