The paper highlights the evidence-based management of four cases of stress fractures syndrome based on various etiopathogenesis and supporting clinical evidence, with suggestion for evidence-based and structured rehabilitation for permanent remission of pain and return to sports and return to preinjury functional levels.
Dr. Siddharth Rai, Apex Trauma Center, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, Uttar Pradesh, India. E-mail: Siddharth.bmc@gmail.com
Introduction: A stress fracture is a painful condition which occurs when the adaptive ability of the bone is unbalanced. This imbalance predominantly occurs due to increased intensity, frequency, or duration of training. Identifying the etiology of stress fracture and its proper treatment prevents recurrence. Besides, evidence-based and supervised rehabilitation is indispensable for permanent remission of pain and return to sports to preinjury functional levels. The case series discusses the continuum of stress reaction to stress fracture in athletes, causes of stress fractures, their management, and return to sport. The paper aims to give a clear discussion about the management with rehabilitation guidelines for metabolic causes of stress fractures.
Case Report: This study was a case series of five cases coming to Sports Medicine outpatient clinic of Sports Injury Centre, VMMC and Safdarjung Hospital, New Delhi, and physical medicine and rehabilitation outpatient clinic of Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow over a period of 1 year. The discussed cases are young Indian athletes, both male and females, who have presentation along the continuum of medial tibial stress syndrome (MTSS) to stress reactions and stress fracture.
Conclusion: The findings of the paper highlight the significance of rehabilitation for individuals suffering from MTSS. Accurate diagnosis with targeted rehabilitation leads to quicker return to sports. The rehabilitation program comprises of identifying and treating the cause of stress fracture, removing any risk factors, biomechanical correction wherever indicated, structured exercise program, training in underwater treadmill, cyclical increase in loading, reducing activity every 3rd week.
Key words: Medial tibial stress syndrome, stress fracture, shin splints, rehabilitation, return to sports.
Stress fractures were first reported in military personnel as “march foot” in the mid-19th century [1]. Normal bone is constantly remodeled by osteoclasts absorbing and osteoblasts laying down new bone. A stress fracture is a painful condition which occurs when the adaptive ability of the bone is unbalanced. This imbalance predominantly occurs due to increased intensity, frequency, or duration of training, also known as Overtraining Syndrome [2]. The etiology of stress fractures can be divided into three causes: metabolic or insufficiency fractures, biomechanical stress fractures, and biological failure. Besides, intrinsic and extrinsic factors contribute to the injury’s development. Intrinsic factors include poor physical conditioning, female sex, hormonal disorder, menstrual disorder, poor bone density, reduced muscle mass, genu valgus knees, and a short leg. Extrinsic factors include high-impact sports activities such as running, abrupt increase in physical activity, irregular running surface, poor footwear, deficient Vitamin D and calcium, and smoking [1]. The most common stress fractures in decreasing order of occurrence are the tibia (23.6%), tarsal navicular (17.6%), metatarsals (16.2%), femur (6.6%), and pelvis (1.6%) [3].
Running more than 25 miles/week on average puts runners at significant risk for stress fractures, which make up about 20% of all sports medicine injuries [4]. Approximately 16% of injuries sustained by runners are stress fractures [4]. In India, a study compared the epidemiology of stress fractures between military trainees of both genders and found the combined incidence of stress fractures to be 8.6% [5]. This paper presents a series of five cases, explaining various causes of stress fractures and their respective management strategies.
Case I
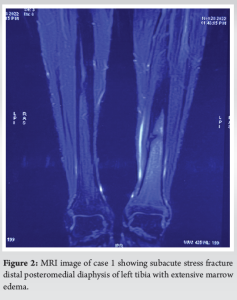
This is a case of a 20-year-old male endurance athlete who presented to the outpatient clinic with severe pain on the inner side of his left leg for the past three months. The pain aggravated on walking and was relieved on taking rest. On examination, there was severe tenderness on the medial side of the left tibia. His routine blood investigations were within normal limits. Radiological tests showed a clear-cut break in the continuity of his tibia at the lower and middle third junctions. MRI confirmed the diagnosis of a stress fracture (Frederickson grade 4) (Fig. 1 and 2).

Management
Ice packs, rest, and patient counseling constituted the management approach. A 6-week above-knee plaster of Paris (PoP) cast followed by patellar tendon bearing PoP was given. For 1 week, he was provided anti-inflammatory drugs and a maintenance dose of 1000 IU of Vitamin D3 and 1000 mg of calcium citrate for 12 weeks. Patient was made aware of the importance of cross-training during this rest period. It was recommended that the patient start isometric strengthening exercises for the hamstrings and quadriceps along with knee joint mobilizations to avoid quadriceps atrophy and knee joint stiffness. With a systematic return to play program that comprised of cyclical increase in loading, reducing activity every 3rd week, aerobic training, lower limb strengthening, balance, and proprioceptive training, the patient was able to return to sport around 6 months.
Case II
A 35-year-old female professional runner presented to the outpatient clinic, with complaints of persistent pain in her right lower leg. She denied any recent changes in her training routine or history of trauma to her lower leg. On physical examination, localized tenderness was noted along the posteromedial aspect of the right tibia. Routine blood tests were within normal limits. In the imaging studies, X-ray was unremarkable however MRI showed signs consistent with medial tibial stress syndrome (MTSS), including periosteal edema and bone marrow edema along the posteromedial aspect of the tibia. (Frederickson Grade 2). Based on these, she was diagnosed with MTSS.
Management
The management included a multi-faceted approach aimed at reducing pain, promoting healing, and preventing recurrence. She was advised to rest for 3 weeks. The patient was also advised to avoid activities that exacerbated her symptoms and reduce her running activities especially if on hard surface and downhill running. She was encouraged to engage in low-impact activities, such as swimming or cycling, to maintain her fitness level without exacerbating her symptoms.
Rehabilitation
The patient was started with a comprehensive rehabilitation program. Manual therapy techniques were initiated to relieve soft-tissue tension and provided exercises to strengthen the lower leg muscles, including the calves and shin muscles. The patient was also educated on proper running form and given exercises to improve her running mechanics along with proper footwear guidance. Once the patient’s symptoms improved, she was instructed on a gradual return to running program. This included gradual progression of weight-bearing with emphasis on cyclical increase in loading and reducing activity every 3rd week.
Case III
A 27-year-old female professional runner presented to the outpatient clinic with a chief complaint of gradually worsening left lower leg pain for the past 4 weeks. She reported that the pain initially started during her training sessions, which were recently increased in intensity and duration.
On examination, the patient appeared to be thin built. Palpation along the middle third of the left tibia elicited tenderness over a localized area. Other orthopedic and neurological examinations were unremarkable. Nutritional history revealed excessively reduced intake of fats and carbohydrates to reduce weight. On calculating her energy deficit, it came out to be very low, amounting to around 10 Kcal. A plain radiograph of the left tibia showed no evidence of any bony abnormalities or fractures. MRI of the left lower leg revealed increased signal intensity on T2-weighted images along the middle third of the left tibia, consistent with a tibial stress reaction. It implied Fredericson’s Grade 2 category on MRI. Routine blood tests were within normal limits, Vitamin D3 was extremely low in the range of 11 nmol/l. Based on the patient’s history, physical examination findings, and imaging results, the diagnosis of MTSS was made.
Management
The patient was advised to rest for 2 weeks, ice, and NSAIDS to reduce active pain. Modification of the training regimen was advised along with rehabilitation exercises to strengthen the lower limb muscles. She was suggested to start a cyclical increase in loading and decrease activity every third week. Besides footwear modification was requested to correct foot overpronation. Most importantly, she was assessed for relative energy deficiency. She was advised on a diet plan according to her level of activity. The patient was followed up regularly, and her symptoms gradually improved throughout 6 weeks.
Case IV
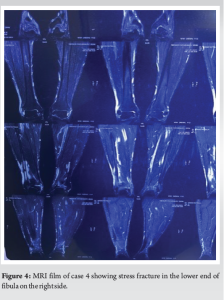
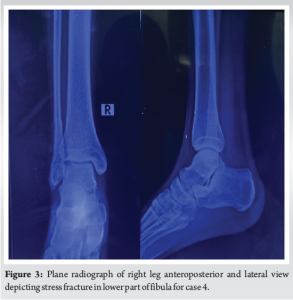
A 25-year-old female endurance athlete, a long-distance runner, presented to the OPD with severe pain in the leg around the lower lateral aspect of the leg at the junction of the upper 2/3rd and lower 1/3rd fibula. She also gave a history of overtraining with many instances of stretching her limits beyond her capacity. On probing about nutritional history, her diet was deficient in carbohydrates and proteins. Her energy deficit turned out to be around 8 kcal, which proved to be a case of Relative Energy Deficiency Syndrome (REDS). Routine blood investigations were within normal range. X-ray film showed an apparent stress fracture was evident in the lower lateral fibular region (Fig. 3). MRI also showed a stress fracture with bone marrow edema (Fig. 4).
Treatment
She was counseled and immobilized with an above-knee cast for 4 weeks with upper body strengthening with free weights and core abdominal strengthening. After 4 weeks, she was given a below-knee pneumatic brace for another 2 weeks. She was started on quadriceps and hamstring strengthening, core abdominal strengthening and hydrotherapy, underwater treadmill, and cycling. Her nutritional deficiencies were also catered to, comprising a high carbohydrate and high protein diet. Her diet also included pre-workout carbohydrate intake and post-workout protein and carbohydrate intake. She was made to follow a gradual return to her previous sport with an emphasis on cyclical increase in loading and decrease in activity every 3rd week.
Case V
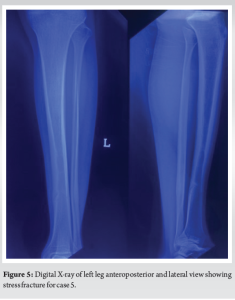
A 35 year-old woman came to the outpatient clinic with left the leg sharp pain for 6 months. She was a long distance runner for the past 10 years. The patient gave birth 8 months ago. The severity of pain increased with walking and prolonged standing. The patient had no history of trauma, previous fractures, systemic or metabolic diseases, or eating disorders. Despite being a lactating mother, she did not take any supplements for Vitamin D and calcium. Local examination showed a tender spot around the posteromedial tibia. Plain radiographs of the left leg showed a cortical break depicting stress fracture of tibia (Fig. 5). Magnetic resonance imaging (MRI) showed an incomplete fracture line at the medial distal tibia and bone marrow edema throughout the distal tibia. The laboratory tests revealed Vitamin D deficiency (12 ng/mL) with normal parathyroid hormone (60 pg/mL) and serum total calcium levels (8.8 mg/dL). Other laboratory findings were normal. Dual-energy X-ray absorptiometry (DXA) was requested to rule out possible underlying osteoporosis. The DXA results were compatible with osteopenia in the lumbar region (total T-score of lumbar vertebrae: −1.5, total Z-score: −1.7; total T-score of femur: 0.4, total Z-score: 0.4). The patient was diagnosed with pregnancy-related osteopenia and stress fracture of the left distal tibia.
Treatment
As part of her treatment, she had to stop bearing weight and wear a cast above the knee for 6 weeks. She also received calcium and Vitamin D supplements at doses of 60,000 IU per week for 10 weeks and 60,000 IU monthly for 6 months. On an SOS basis, paracetamol was administered to her. She was later started on aerobic training, muscle strengthening, balance, and proprioceptive training.
Robert Jones described stress fractures as early as 1902 when he described a fracture of the fifth metatarsal bone of the foot in maypole dancers [6]. Stress fractures are common injuries that begin with repetitive and excessive stress on the bone. The concept of relative energy deficiency syndrome (REDS) was described in 2014 by the International Olympic Committee, which described it as a cause of impaired physiological function, including metabolic rate, menstrual function, bone health, immunity, protein synthesis, and cardiovascular health. The optimal energy expenditure is 45 Kcal/ kg FFM/day [7]. Plain radiographs can be used as a baseline for diagnosis. Stress fractures are usually identified by indirect findings: periosteal thickening or sclerosis, cortical changes with initial decreased density (“grey cortex”), and, more commonly, later callus formation, or endosteal thickening and sclerosis [8, 9]. More precisely, an MRI or a bone scan can distinguish stress reactions. The best method for accurately determining activity level is SPECT imaging. However, MRI may also identify reactive bone remodeling (interpreted as early stress injuries) and, therefore, should be clinically correlated with stress fracture [10]. In the case of metabolic issues, the metabolic deficiency needs to be evaluated and corrected accordingly. The differential diagnosis for such a clinical presentation included delayed onset muscle soreness (DOMS), exercise-induced muscle dysfunction, exercise-induced compartment syndrome, popliteal artery entrapment syndrome, and stress fractures. The cases discussed describe a metabolic cause as the predisposing factor, leading to an evident stress fracture and stress reaction in respective cases. Management in all cases is essentially rest, support to the involved part, and abstinence from the strenuous physical activity. This should be accompanied by identifying the physiological failure, allowing metabolic processes to catch up and gradually reintroducing activity. Literature and clinical practice mention and recommend the following treatment methods: Stretching of calf muscles and wearing orthopedic insoles to reduce overpronation [11], massage, electrotherapy [12], and acupuncture [13]; however, no clear recommendations are given. Recent research has shown that extracorporeal shock wave therapy (ESWT) efficiently treats MTSS with promising results [14]. There are also excellent clinical trials using pulsed low-frequency ultrasound (LIPUS) in non-union cases [15]. The use of Teriparatide (synthetic Parathhormone) in stress fractures has also proved promising due to the benefits of ongoing remodeling. Intravenous pamidronate has been shown to inhibit the activation of cortical osteoclasts and increase cortical thickness [16]. Stretching and strengthening specific muscles are crucial in correcting muscle imbalances.
A single case series cannot recommend treatment for the whole population. However, there needs to be a precise decision and recommendation about the efficacy and advantage of any treatment.
An imbalance in the bone’s ability to adapt results in a stress fracture. Recurrence can be avoided by determining the cause of stress fractures and treating them appropriately. A return to pre-injury functional levels in sports requires evidence-based and structured rehabilitation.
After the stress fracture heals, a gradual return to the previous sport should be encouraged with emphasis on a cyclical increase in loading and decrease in activity every 3rd week. Sports nutrition and looking for REDS constitute an indispensable adjunct in the effective management of the metabolic cause of MTSS.
References
- 1.McCormick F, Nwachukwu BU, Provencher MT. Stress fractures in runners. Clin Sports Med 2012;31:291-306. [Google Scholar]
- 2.Meeusen R, Duclos M, Foster C, Fry A, Gleeson M, Nieman D, et al. Prevention, diagnosis, and treatment of the overtraining syndrome: Joint Consensus Statement of the European College of Sport Science and the American College of Sports Medicine. Med Sci Sports Exerc 2013;45:186-205. [Google Scholar]
- 3.Kahanov L, Eberman LE, Games KE, Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med 2015;6:87-95. [Google Scholar]
- 4.Moreira CA, Bilezikian JP. Stress fractures: Concepts and therapeutics. J Clin Endocrinol Metab 2017;102:525-34. [Google Scholar]
- 5.Kunte R, Basannar D, Chatterjee K, Agarwal PK, Prasad L, Dubey P, et al. Gender differential and implications in the epidemiology of stress fractures among cadets of Indian Armed Forces. Med J Armed Forces India 2017;73:356-62. [Google Scholar]
- 6.Jones R. I. Fracture of the base of the fifth metatarsal bone by indirect violence. Ann Surg 1902;35:697-700. [Google Scholar]
- 7.Mountjoy M, Sundgot-Borgen J, Burke L, Carter S, Constantini N, Lebrun C, et al. The IOC consensus statement: Beyond the Female Athlete Triad--Relative Energy Deficiency in Sport (RED-S). Br J Sports Med 2014;48:491-7. [Google Scholar]
- 8.Ishibashi Y, Okamura Y, Otsuka H, Nishizawa K, Sasaki T, Toh S. Comparison of scintigraphy and magnetic resonance imaging for stress injuries of bone. Clin J Sport Med 2002;12:79-84. [Google Scholar]
- 9.Ohta-Fukushima M, Mutoh Y, Takasugi S, Iwata H, Ishii S. Characteristics of stress fractures in young athletes under 20 years. J Sports Med Phys Fitness 2002;42:198-206. [Google Scholar]
- 10.Batt ME, Ugalde V, Anderson MW, Shelton DK. A prospective controlled study of diagnostic imaging for acute shin splints. Med Sci Sports Exerc 1998;30:1564-71. [Google Scholar]
- 11.Loudon JK, Dolphino MR. Use of foot orthoses and calf stretching for individuals with medial tibial stress syndrome. Foot Ankle Spec 2010;3:15-20. [Google Scholar]
- 12.Morris RH. Medial tibial syndrome: A treatment protocol using electric current. Chiropract Sports Med 1991;5:5-8. [Google Scholar]
- 13.Schulman RA. Tibial shin splints treated with a single acupuncture session: Case report and review of the literature. J Am Med Acupuncture 2002;13:7-9. [Google Scholar]
- 14.Moen MH, Rayer S, Schipper M, Schmikli S, Weir A, Tol JL, et al. Shockwave treatment for medial tibial stress syndrome in athletes; a prospective controlled study. Br J Sports Med 2012;46:253-7. [Google Scholar]
- 15.Rubin C, Bolander M, Ryaby JP, Hadjiargyrou M. The use of low-intensity ultrasound to accelerate the healing of fractures. J Bone Joint Surg Am 2001;83-A(2):259-70. [Google Scholar]
- 16.Stewart GW, Brunet ME, Manning MR, Davis FA. Treatment of stress fractures in athletes with intravenous pamidronate. Clin J Sport Med 2005;15:92-4. [Google Scholar]