With this technique, a full control of the orthopaedic traction table can be achieved and consequently a closed anatomic reduction can be performed.
Dr. Pierre-Baptiste Arnaud, Department of Orthopaedics, HFR Fribourg, Chem. des Pensionnats 2/6, 1752 Villars-sur-Glâne, Switzerland. E-mail: pba0193@gmail.com
Introduction: Closed anatomical reduction of per-trochanteric fractures requires 3-axis control of the orthopedic traction table (OTT) which is challenging in patients having suffered a previous ipsilateral Gritti-Stokes amputation.
Case Report: A 52-year-old man, known by Gritti-Stokes amputated (GSA) 10 years before, was admitted to our trauma center after a fall from his height. We describe a simple method for positioning a previously ipsilateral GSA patient in an OTT to reduce displaced a femoral per-trochanteric fracture site and to maintain it during surgery. The proposed method attaches non-adhesive bands to the stump, reinforced by the wire guide package to increase rigidity and allow 3-axis control of the OTT.
Conclusion: This method can be performed in a standard trauma operating room, it only uses materials that were planned to be used during surgery, and consequently, it does not increase operative costs.
Keywords: Gritti-Stokes amputation, per-trochanteric femoral fracture, patient positioning, orthopedic trauma, orthopedic traction table.
Patients having suffered a lower limb amputation often are autonomous with a limb prosthesis and they present an increased risk of fall and fracture to the proximal femur [1]. In trauma surgery, patient’s positioning is crucial as it allows easier fracture reduction. Without three-axis control, orthopedic traction table (OTT) becomes impossible to be accurately used. There are reports describing how to position a patient having suffered under-the-knee amputations, either using invasive means as trans-epicondylar pins or external-fixators, either using very expensive carbon molds securing the stump [2]. To the best of our knowledge, there are no reports on Gritti-Stokes amputated (GSA) patients. The following method describes a non-invasive solution to position a previously ipsilateral GSA patient on an OTT, permitting a three-axis control, exclusively using materials, we could easily find in a standard trauma operating room.
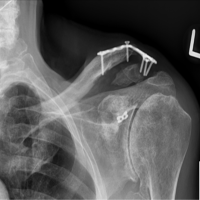
A 52-year-old man, known by GSA 10 years before, was admitted to our trauma center after a fall from his height. The radiological assessment showed a 31-A1 per-trochanteric fracture, according to AO/OTA (Fig. 1 and 2a). The mean dual-energy X-ray absorptiometry T-score of the femoral trochanteric area was 2.7, indicating osteoporosis.
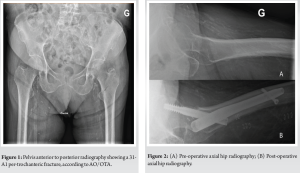
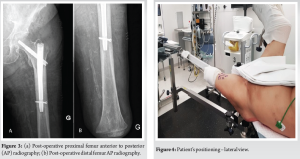
Before this accident, he was able to walk independently and perform basic daily activities with his limb prosthesis. Surgical treatment would prevent decubitus, respiratory, and thrombotic complications and make nursing care easier. We planned for the gold-standard treatment: A closed reduction and antegrade intra-medullary nail (Fig. 2b, 3a and 3b). The patient would benefit from such a minimally-invasive surgery which would provide a shorter moment arm combined with a stiff construction.
Patient positioning
The patient was placed on supine position on an OTT under general anesthesia. The contralateral limb was secured at 90° of hip and knee flexion, abducted, and internally rotated thanks to a standard leg support device (Fig. 3 and 4). To obtain rotation control, we used the wire guide’s package (Stryker T2® ball-tipped Ø3 × 1000 mm) folded once (Fig. 4-6). The proximal end was put together with the stump and was fixed through a skin-pulling band (Fig. 4). The skin was protected with gauze. The distal end was connected to the OTT thanks to auto-adhesive band (Fig. 4 and 5). As a result, adequate traction and rotation could be applied to a protected stump.


Surgical procedure
The fracture’s closed reduction was accomplished by stump’s proper traction, slight flexion, and internal rotation. After proximal reaming, a 125° Gamma nail (Stryker®) was inserted, followed by the positioning of a cervicocephalic screw of appropriate length (Fig. 2b and 3). The nail was locked in a static position.
Rehabilitation protocol
The patient was allowed to start walking, helped by a pair of crutches, on full weight-bearing, the day after surgery.
Literature does not support for or against any specific positioning on the above-mentioned situation. It was challenging to find a simple, efficient, and economical way, only using materials available in a standard trauma operating room, to install a patient having suffered a previous ipsilateral GSA on an OTT. There are a couple of reports on the management of femur per-trochanteric fractures in patients having suffered a previous ipsilateral below-the-knee amputation, which are not reproducible in these patients [3,4]. One of the methods described in patients having suffered an above-the-knee amputation is the insertion of a Steinmann pin in the distal part of the femur [2]. Even though a Steinmann pin and the rope method can maintain adequate traction and abduction/adduction position, it is difficult to obtain rotational stability if counter-resistance force needs to be applied [5]. The second method described by Gamulin and Farshad consists in introducing an external fixator to the stump and fix the rod and the external fixator together to the OTT [6]. This allows good stump’s stability but makes the intra-operative adjustments more delicate to perform [7]. The above-mentioned methods will increase costs, the risk of soft tissue damage, and infection at the entry points of the pins [8]. They also put the distal femur at increased risk of fracture by performing traction on an osteoporotic bone. Finally, the new scars may cause discomfort when using conventional prostheses. A third non-invasive method, described by Rethnam et al., consists of an assistant handily maintaining the fracture’s reduction during surgery [9]. This method is not ideal because it is difficult to obtain sufficient traction and torque while maintaining the fracture reduced during the entire surgery. Our method permits closed-controlled three-axis reduction in previously GSA or distal transfemoral amputated patients. In this context, attaching non-adhesive bands to the stump reinforced by the wire guide package to increase rigidity, it would result in enough stump’s traction and rotation. This method can be used in any standard OTT without increasing operative costs. Our technique is not free of limitations. There is a risk of band loosening, which would also increase the risk of surgical field contamination and loss of reduction during surgery. There is also the risk of stump and skin damage due to skin traction (Fig. 7) [10]. Thus, we do not advise this technique in patients with fragile stump’s skin and complex types of fractures (which would mean stronger traction and longer operative time). To minimize this risk, we would also recommend that the surgery should be performed by experienced surgical teams to shorten operative time.

It is important to emphasize that planning and surgical technique are of core importance when a closed anatomical reduction is to be obtained. Although there are several options to the surgical treatment of per-trochanteric fractures in standard patients, it still remains a challenge in previously ipsilateral GSA patients. All in all, per-trochanteric fractures can be managed in patients having suffered an ipsilateral GSA through a skin traction band on the stump associated with the package of the wire guide to be used during the surgery. With this technique, a full control of the OTT can be achieved and consequently, a closed anatomic reduction can be performed. All materials needed are available in a standard trauma operating room and costs are not increased. Stump’s skin should be attentively surveilled after the surgical procedure.
This technique allows full control of the OTT and consequently, permitting a closed anatomic reduction can be performed.
References
- 1.O’Keeffe B, Rout S. Prosthetic rehabilitation in the lower limb. Indian J Plast Surg 2019;52:134-43. [Google Scholar | PubMed]
- 2.Berg AJ, Bhatia C. Neck of femur fracture fixation in a bilateral amputee: An uncommon condition requiring an improvised fracture table positioning technique. BMJ Case Rep 2014;2014:bcr2013203504. [Google Scholar | PubMed]
- 3.Al-Harthy A, Abed R, Campbell AC. Manipulation of hip fracture in the below-knee amputee. Injury 1997;28:570. [Google Scholar | PubMed]
- 4.Ramseier LE, Werner CM, Hug T, Preiss S. Suprakondylare extension einer pertrochantaren femurfraktur bei einem patienten mit unterschenkelamputation. Unfallchirurg 2005;108:239-40. [Google Scholar | PubMed]
- 5.Paley D, Jackson RW. Surgical scrub sponges as part of the traction apparatus: An alternative to pin site care to reduce pin track infections. Injury 1985;16:605-6. [Google Scholar | PubMed]
- 6.Gamulin A, Farshad M. Amputated lower limb fixation to the fracture table. Orthopedics 2015;38:679-82. [Google Scholar | PubMed]
- 7.Checketts R, Otterburn M, MacEachern A. Pin tract infection: Definition, incidence and prevention. Int J Orthop Trauma 1993;3:16-9. [Google Scholar | PubMed]
- 8.Parameswaran AD, Roberts CS, Seligson D, Voor M. Pin tract infection with contemporary external fixation: How much of a problem? J Orthop Trauma 2003;17:503-7. [Google Scholar | PubMed]
- 9.Rethnam U, Yesupalan RS, Shoaib A, Ratnam TK. Hip fracture fixation in a patient with below-knee amputation presents a surgical dilemma: A case report. J Med Case Rep 2008;2:296. [Google Scholar | PubMed]
- 10.Portnoy S, Siev-Ner I, Yizhar Z, Kristal A, Shabshin N, Gefen A. Surgical and morphological factors that affect internal mechanical loads in soft tissues of the transtibial residuum. Ann Biomed Eng 2009;37:2583-605. [Google Scholar | PubMed]