This incident highlights the importance of clinically examining the patient’s scrotum in severe injuries to ensure the testis position and it also reminds us to look at CT scans carefully for the same. Orchidopexy can provide good reproductive function if performed at the right time.
Dr. G Siva Srivastava, Department of Orthopedics, Jai Prakash Narayan Apex Trauma Center, AIIMS, New Delhi, India. E-mail: dr.sivasrivastava@gmail.com
Introduction: With advancement, the occurrence of road traffic accidents is common. Timely management of fractures of the spine and pelvis is of the utmost importance for survival, ambulation, and maintenance of normal life. Genitourinary complications following pelvic ring injuries are not unknown; however, testicular dislocation is rare and can cause significant morbidity if not managed appropriately.
Case Report: Our case was a 25-year-old male who was presented to the tertiary trauma center following a motorcycle accident. He had an anteroposterior compression (APC) fracture of the pelvic ring (APC-III, Arbeitsgemeinschaft für Osteosynthesefragen 61–C1.2), D8-D9 vertebra compression fracture, fracture of the left distal radius, and radio-carpal dislocation. However, no concomitant genitourinary injury was noticed at the initial assessment. After resuscitation, the pelvis was planned to be fixed with an anterior symphyseal plate and posterior sacroiliac joint fixation using 2 cancellous screws. While using Stoppa’s approach, surprisingly, the right testicle was observed to be inferior to the pubis. Trauma surgery help was sought and the dislocated testis was reduced and managed with orchidopexy after checking the viability. At the follow-up of 1 year, the pelvic fracture was united without urogenital complication.
Conclusion: In cases of complex pelvic ring injury, a careful genital examination should be performed and a multi-disciplinary team approach with compromising of radiology, traumatology, and orthopedics departments should be adopted for better patient outcomes.
Keywords: Genito-urinary injuries,traumatic testicular dislocation, pelvic fracture
The incidence of pelvic fracture following a high-energy trauma is approximately 1–3% [1]. The overall incidence of combined spinal and pelvis fractures is reported to be around 10.4%. The genitourinary injuries following pelvic fracture are not uncommon. However, the association of testicular dislocation is a rare event. Fewer than 60 cases have been documented in the literature [2]. Testicular dislocation in the setting of pelvic ring injury most commonly occurs as a result of “fuel tank” or “straddle”-type injuries, in motorcycle accidents [3]. Delay in diagnosis and treatment is associated with an increased rate of orchidectomy and loss of testicular and spermatic function, which can lead to impaired fertility. We present a unique case of missed traumatic unilateral testicular dislocation with a fracture of the spine and pelvic ring that was not diagnosed until surgery. We discuss the review of literature about such injuries, their outcomes, and steps that may be taken to prevent any delays in diagnosis.
A 25-year-old man was presented to the trauma emergency after a motorcycle collision with a heavy four-vehicle. The primary management was done elsewhere and then referred to our center for definitive management. The patient was re-evaluated using advanced trauma life support guidelines and was resuscitated. Upon primary assessment, the patient was Borderline [4].
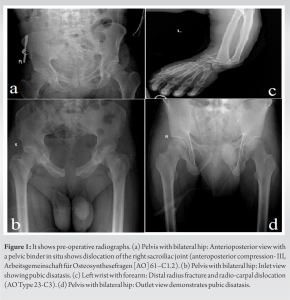
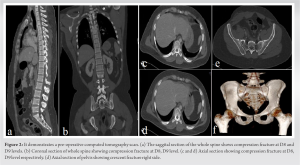
In the primary survey, there was a lacerated wound of size 3 × 2 cm over the anterior aspect of the left elbow and 10 × 2 cm over the left wrist without distal neuro-vascular deficit. There were bruises on the scrotum and penile base with palpable testis in the scrotum. Upon subsequent radiological evaluation, he was diagnosed with D8, D9 vertebra compression fracture with ASIA E neurology, pubic diastasis, and right sacroiliac joint dislocation (anteroposterior compression-III, Arbeitsgemeinschaft für Osteosynthesefragen [AO] 61–C1.2), gustilo-anderson open grade 3a fracture of the left distal radius and radio-carpal dislocation (AO Type 23-C3) (Fig. 1 and 2). After a secondary survey assessment, the patient was taken to the operation theatre for management of an open grade 3A fracture of the left distal radius and radio-carpal dislocation.
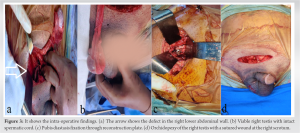
Once the patient improved clinically and built up his hematocrit level, he was posted for elective pelvic fracture fixation i.e. on day 4 following trauma. Surgery was planned to apply a reconstruction plate for pubic diastasis through Stoppa’s approach and closed reduction internal fixation for Sacro-Iliac (SI) joint fixation using percutaneous cannulated cancellous screws (CCS). Intra-operatively during deep dissection in Stoppa’s approach, inadvertently an ovoid smooth white swelling was seen protruding out from below the pubis on the right side internally through the inguinal canal into the abdominal cavity (Fig. 3).
On careful examination, the right testis was found to have migrated into the pelvis through the abdominal wall defect. In an operative assessment from the trauma surgeons, it was sought and the dislocated testis was reduced by manual manipulation and orchidopexy was done. This was followed by anterior pubic diastasis fixation with a 5-hole reconstruction plate and the right SI joint close reduction internal fixation was done through two CCS. The associated spine fracture was managed conservatively.
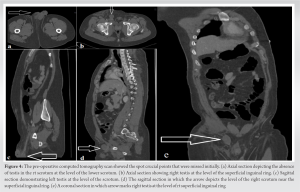
In the post-operative period, retrospective analysis of an abdominal computed tomographic scan confirmed the diagnosis of right testicular dislocation (Fig. 4). The patient did not any history of cryptorchidism, retractile testis, or hernia. Hence, the diagnosis of missed right testicular dislocation was confirmed. There were no immediate post-operative complications noted. The wound was healed in the follow-up. The patient was followed regularly for up to 1 year. On ultrasonography of the bilateral scrotum, there was adequate blood flow in the bilateral testis during his last visit. However, the patient and his relatives were counseled about the occurrence of inguinal hernia in the future.
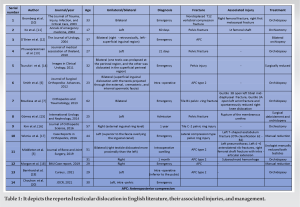
Claubry first described this entity in 1818; traumatic testicular dislocation to the extra scrotal migration of one or both testicles as a consequence of direct scrotal trauma [5]. Motorcycle collisions are the most frequent causative mechanism; the sudden deceleration of the motorcycle catapults the rider forward. Because the rider is straddled over the saddle, his perineum and scrotum are struck in the midline by the bike tank, which presses the testes upward, forcibly displacing them in a lateral and upward direction [6]. Boudissa et al. emphasized the importance of initial physical examination, including palpation and inspection [7]. It is important to ask about any history of cryptorchidism, testicular retraction, or previous inguinal hernia. On clinical evaluation, testicular dislocation may appear as an empty scrotum, loose skin (Brockman’s sign), testicular hematoma, and inguinal mass. This physical examination may be hampered by pain, edema, hematoma, hematocele, deep testicular dislocation, damage to neighboring structures, or obesity of the patient. Naseer et al. also mentioned the importance of scrotal examination in a traumatic patient [8]. Doppler ultrasonography is helpful in detecting the blood flow and therefore the viability of the testicle. In addition, Ezra et al. [9] emphasized the need for computed tomography (CT) for the rapid diagnosis of scrotal trauma, including testicular rupture, torsion, dislocation, hematoma, or contusion, as well as epididymal, scrotal, and urethral injuries, because most polytrauma or pelvic trauma patients are initially assessed by CT. In our case, an initial CT scan (Fig. 4) revealed right traumatic testis dislocation. However, we did not take cognizance because the testis was palpable when the patient had a pelvis binder. To avoid such mistakes in the future, we must be alert to the feasibility of testicular dislocation in addition to fracture patterns when initial CT scans are performed in cases of pelvic fractures. Surgeons should be aware that inattention to testicular injuries including testis dislocation, rupture, and torsion in cases of polytrauma or pelvic fracture may lead to inevitable testicular resection in the future. Reported cases in English literature are mentioned in Table 1 with their management.
This incident highlights the importance of clinically examining the patient’s scrotum in severe injuries to ensure the testis position and it also reminds us to look at CT scans carefully for the same.
Close suspicion should be considered particularly in adults in the case of a pelvic fracture who had a fuel tank type of injury pattern. Orchidopexy can provide good reproductive function if performed at the right time.
References
- 1.Ankarath S, Giannoudis PV, Barlow I, Bellamy MC, Mathews SJ, Smith RM. Injury pattern associated with mortality following motorcycle crashes. Injury 2002;33:473-7. [Google Scholar]
- 2.Shefi S, Mor Y, Dotan ZA, Ramon J. Traumatic testicular dislocation: A case report and review of published reports. Urology 1999;43:743-5. [Google Scholar]
- 3.Middleton AH, Martin JM, Wittmann TA, Schmeling GJ. Testicular dislocation after pelvic ring injury: A report of 2 cases. JBJS Case Connect 2019;9:141. [Google Scholar]
- 4.Pape HC, Giannoudis P, Krettek C. The timing of fracture treatment in polytrauma patients: Relevance of damage control orthopedic surgery. Am J Surg 2002;183:622-9. [Google Scholar]
- 5.Claubry EG. Observacions sur une retrocession subite des deux testicles dans l0 abdomen, a la suite d’une violente compression de la parte infe´rieure de la paroid abdominale par une roue´ de la charrette. J Gen Med Chir Phram 1818;64:325-8. [Google Scholar]
- 6.Smith CS, Rosenbaum CS, Michael Harris A. Traumatic bilateral testicular dislocation associated with an anterior posterior compression fracture of the pelvis: A case report. J Surg Orth Adv 2012;21:162-4. [Google Scholar]
- 7.Boudissa M, Ruatti S, Maisse N, Arvin-Berod A, Trilling B, Long JA, et al. Bilateral testicular dislocation with pelvic ring fracture: A case report and literature review. Orthop Traumatol Surg Res 2013;99:485-7. [Google Scholar]
- 8.Naseer A, King D, Lee H, Vale J. Testicular dislocation: the importance of scrotal examination in a trauma patient. Ann R Coll Surg Eng 2012;94:e109-10. [Google Scholar]
- 9.Ezra N, Afari A, Wong J. Pelvic and scrotal trauma: CT and triage of patients. Abdom Imaging 2009;34:541-4. [Google Scholar]
- 10.Bromberg W, Wong C, Kurek S, Salim A. Traumatic bilateral testicular dislocation. J Trauma Acute Care Surg 2003;54:1009-11. [Google Scholar]
- 11.Ko SF, Ng SH, Wan YL, Huang CC, Lee TY, Kung CT, et al. Testicular dislocation: An uncommon and easily overlooked complication of blunt abdominal trauma. Ann Emerg Med 2004;43:371e5. [Google Scholar]
- 12.O’Brien MF, Collins DA, McElwain JP, Akhtar M, Thornhill JA. Traumatic retrovesical testicular dislocation. J Urol 2004;171:798. [Google Scholar]
- 13.Phuwapraisirisan S, Lim M, Suwanthanma W. Surgical reduction in a delayed case of traumatic testicular dislocation. J Med Assoc Thai 2010;93:1317-20. [Google Scholar]
- 14.Tsurukiri J, Kaneko N, Mishima S. Bilateral traumatic testicular dislocation. Urology 2011;78:1306. [Google Scholar]
- 15.Gómez RG, Storme O, Catalán G, Marchetti P, Djordjevic M. Traumatic testicular dislocation. Int Urol Nephrol 2014;46:1883-7. [Google Scholar]
- 16.Kim WY, Lee SW, Jang H, Kim DY. Delayed detection of testicular dislocation with pelvic ring fracture: A case report. J Orthop Sci 2016;21:702-4. [Google Scholar]
- 17.Wiznia DH, Wang M, Yeon-Kim C, Tomaszewski P, Leslie MP. Traumatic testicular dislocation associated with lateral compression pelvic ring injury and T-shaped acetabulum fracture. Case Rep Orthop 2016;2016:9706392. [Google Scholar]
- 18.Morgan O, Davenport D, Enright K. Pelvic injury is not just pelvic fracture. BMJ Case Rep 2019;12:e232622. [Google Scholar]
- 19.Bernhard Z, Myers D, Passias BJ, Taylor BC, Castaneda J. Testicular dislocation after unstable pelvic ring injury. Cureus 2021;13:e13119. [Google Scholar]
- 20.Chouhan V, Ladhania M, Chouhan K. Pelvic fracture associated with intrapelvic dislocation of testis. J Orthop Case Rep 2021;11:90-4. [Google Scholar]